Tooth wear is a common dental condition. In some cases the extent of wear can be catastrophic with severe loss of tooth tissue, resulting in poor esthetic and functional outcomes. The terminology used by various authors and practitioners in different countries can be confusing; the same processes are not referred to consistently when describing the various elements of tooth wear.
Traditionally, the main three types of wear are described as attrition, abrasion, and erosion. “Attrition” is wear of teeth by opposing teeth; “abrasion” is wear of teeth by an external object, such as a toothbrush, and “erosion” is wear of teeth by acids. Some believe that tooth wear results from contributions from all three processes, and others classify smooth surface lesions as erosion and any lesions on the occlusal surfaces as attrition. Acids play a major role in tooth wear. Erosion doesn’t often happen in isolation. There are contributions from attrition and abrasion. This article discusses “erosive tooth wear,” a terminology that has been accepted by international authorities as a good representation of the above concepts. 1Carvalho T S, Colon P, Ganss C, et al. Consensus Report of the European Federation of Conservative Dentistry: Erosive tooth wear diagnosis and management. Swiss Dent J 2016;126:342-6.
Pathological or Physiological Wear
Some degree of tooth wear happens physiologically over time and, therefore, with age some wear is expected and normal, unlike dental caries which is always pathological and preventable. One would expect wear and tear of teeth in an 80-year-old patient, but the same level of wear in a younger patient in his/her 20s could be pathological. It is therefore important to consider this when assessing patients and classifying the wear as either pathological or physiological.
Prevalence
Several studies suggest that pathological erosive wear is common. Comparison of the various reports is difficult as the definitions and the scoring systems used vary. However, it is safe to say between 2% and 30% of adults and children are affected.2Xhonga FA, Valdmanis S. Geographic comparisons of the incidence of dental erosion: a two centre study. J Oral Rehabil 1983;10:269-77.,3Van’t Spijker A, Rodriguez JM, Kreulen CM, et al. Prevalence of tooth wear in adults. Int J Prosth 2009;22:35-42.,4Kreulen CM, Van‘t SA, Rodriguez JM, et al. Systematic review of the prevalence of tooth wear in children and adolescents. Caries Res 2010;44:151-9.,5Jaeggi, T, Lussi A. Prevalence, incidence and distribution of erosion. Monogr Oral Sci 2014;25:55-73. A recent multicenter pan-European study assessing erosive wear in 3,187 18- to 35-year-olds reported that 30% of adults had visible tooth wear, 3% of which was severe. 6Bartlett DW, Lussi A, West NX, et al. Prevalence of tooth wear on buccal and lingual surfaces and possible risk factors in young European adults. J Dent 2013;41:1007-13.
Etiology of Erosive Tooth Wear
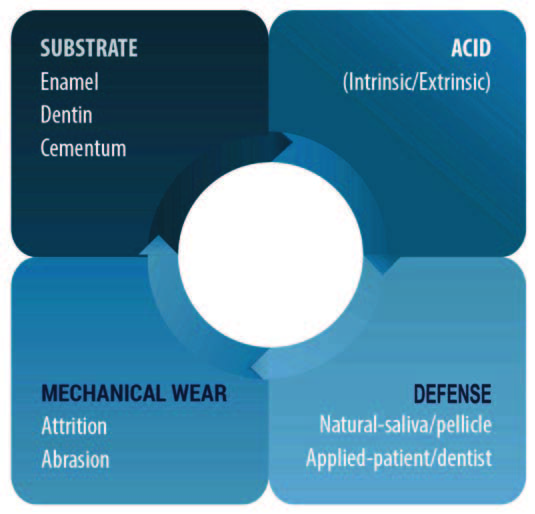
The processes involved in erosive tooth wear are very different than those involved in dental caries. Acids in dental caries are produced as a result of fermentation of sugars by bacteria in dental plaque over time, and surfaces affected by caries are normally covered with dental plaque. Erosive tooth wear results when acids either from foods and drinks or regurgitated/vomited from the stomach contact the teeth directly. In this process no bacteria are involved and the tooth surfaces are usually plaque-free and clean. The processes involved in erosive tooth wear are not simple and there is an interaction of various factors that could result in tissue loss. Acids contact the teeth, resulting in demineralization and softening of the tooth surface. This is referred to as “early erosion,” and at this stage the process is reversible and re-hardening can occur. If the process continues, the softened surface is eventually lost. This process is accelerated by attrition or abrasion which results in more tissue loss. 7Shellis RP, Ganss C, Ren Y, Zero DT, Lussi A. Methodology and models in erosion research: discussion and conclusions. Caries Res 2011;45(Suppl 1):69-77.,8Addy M, Shellis RP. Interaction between attrition, abrasion and erosion in tooth wear. Monogr Oral Sci 2006;20:17-31.,9Amaechi BT, Higham SM, Edgar WM. Influence of abrasion in clinical manifestation of human dental erosion. J Oral Rehabil 2003;30:407-13. Current research and thinking has focused on prevention of demineralization and facilitation of re-hard-ening/remineralization to prevent the process from starting, or reverse it once it has started. Figure 1 represents these concepts. The reversal of the process can happen either through natural, inherent biological defense mechanisms or through the application of products. Saliva and pellicle provide natural protection against demineralization and facilitate remineralization.
Sources of Acids
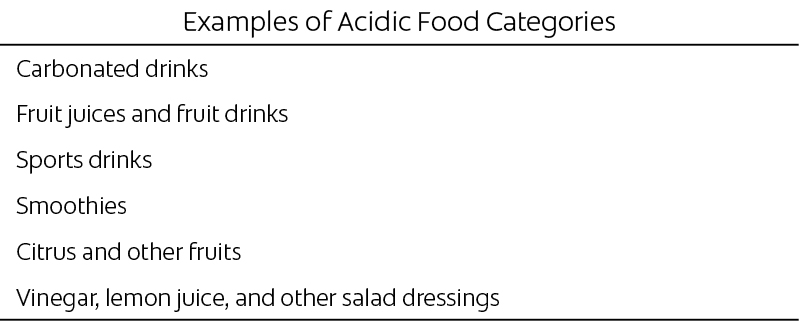
Dietary Acids. Various acidic foods and drinks have been reported to have erosive potential (Table 1). These can be categorized into carbonated drinks, juices and smoothies, sports drinks, citrus fruits, and others, such as vinegar and lemon dressings. 10Järvinen VK, Rytömaa II, Heinonen OP. Risk factors in dental erosion. J Dent Res 1991;70:942-7.,11Lussi A, Jaeggi T, Zero D. The role of diet in the aetiology of dental erosion. Caries Res 2004;38(Suppl 1):34-44.,12Cavadini C, Siega-Riz AM, Popkin BM. US adolescent food intake trends from 1965 to 1996. Arch Dis Child 2000;83:18-24.,13Bardolia P, Burnside G, Ashcroft A, Milosevic A, Goodfellow SA, Rolfe EA, Pine CM. Prevalence and risk indicators of erosion in thirteen- to fourteen-year-olds on the Isle of Man. Caries Res 2010;44:165-8.,14Milosevic A. Dental erosion in a series of referred patients was statistically associated with gastric reflux, acidic drink intake of more than 0.5 L per day, and low salivary buffering capacity. J Evid Based Dent Pract 2010;10:176-8.
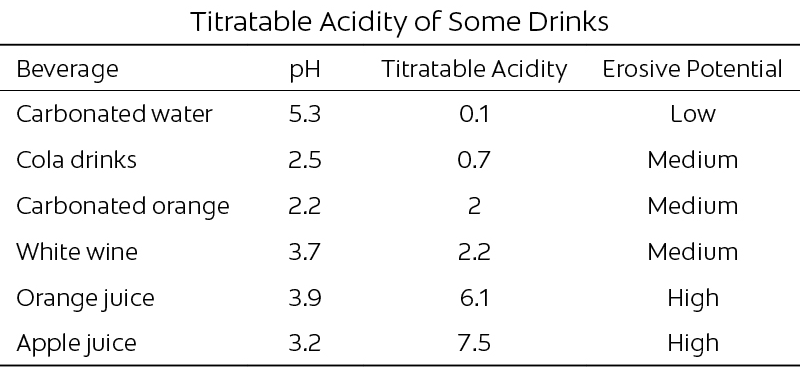
Categorizing foods and drinks in this simplistic way can be misleading. Some other points to consider are the titratable acidity, buffering capacity, and mineral contents of the foods and drinks, and not simply the pH. Titratable acidity measures the amount of acid in a solution; pH measures the strength of the acid (see Table 2). Other important factors include the method, frequency, and timing of the consumption. 15Millward A, Shaw L, Harrington E, Smith A. Continuous monitoring of salivary flow rate and pH at the surface of the dentition following consumption of acidic beverages. Caries Res 1997;31:44-9.,16Moazzez R, Smith BG, Bartlett DW. Oral pH and drinking habit during ingestion of a carbonated drink in a group of adolescents with dental erosion. J Dent 2000;28:395-7.
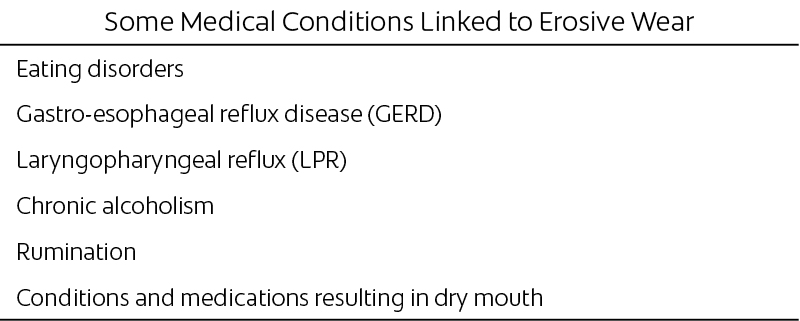
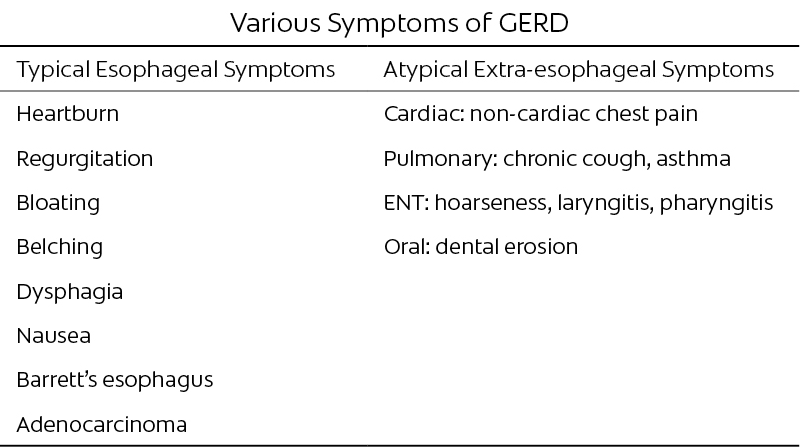
Regurgitated Acids and Medical Conditions. Acidic contents from the stomach can enter the oral cavity either by voluntary vomiting or involuntary regurgitation. Medical conditions that have been reported to be linked to erosive wear (Table 3) are eating disorders (anorexia and bulimia nervosa), gastro-esophageal reflux disease (GERD), laryngopharyngeal reflux (LPR), chronic alcoholism, pregnancy, and dietary rumination, a condition in which people repeatedly and unintentionally spit up (regurgitate) undigested or partially digested food from the stomach, rechew it, and then either reswallow the food or spit it out. One of the conditions most investigated in relation to erosive tooth wear is GERD. Symptoms of GERD are very common and have important adverse effects on patients’ health and quality of life. Up to 10% of the population seeks medical advice for reflux-related problems. There is no doubt that GERD and erosive tooth wear are related, but exactly why some people with GERD also suffer from erosive wear and others do not has not been established. Some theories are that the acid travels up into the mouth in some and not in others, the regurgitated juice may be non-acidic in those without erosive wear, and saliva and pellicle may vary between individuals. Symptoms and signs of GERD are either esophageal or extra-esophageal. Some of these have been listed in Table 4. The most common esophageal symptoms are heartburn and regurgitation. It is important to also consider the extra-esophageal symptoms, such as chronic cough and asthma, in relation to erosive wear, as these symptoms are usually indicative of acid traveling farther up the esophagus and therefore more likely to enter the oral cavity. A more recent term used for this group is “laryngo-pharyngeal reflux.” The prevalence of GERD-related chronic cough ranges from 5% to 41%. The prevalence of dental erosion in GERD patients ranges from 5% to 47.5%, with a mean of 32.5%. Another important point to remember is that some patients suffering from GERD have no other symptoms and signs other than erosive wear, a condition often referred to as “silent reflux.” 17Dent J, El-Serag HB, Wallander MA, Johansson S. Epidemiology of gastro-oe-sophageal reflux disease: a systematic review. Gut 2005;54:710-7.,18Fox M, Forgacs I. Gastro-oesophageal reflux disease. BMJ 2006;332:88-93.,19Moazzez R, Bartlett D, Anggiansah A. Dental erosion, gastro-oesophageal reflux disease and saliva: how are they related? J Dent 2004;32:489-94.,20Munoz JV, Herreros B, Sanchiz V, et al. Dental and periodontal lesions in patients with gastro-oesophageal reflux disease. Dig Liver Dis 2003;35:461-7.,21Schroeder PL, Filler SJ, Ramirez B, et al. Dental erosion and acid reflux dis-ease. Ann Intern Med 1995;122:809-15.
Diagnosis of Erosive Tooth Wear
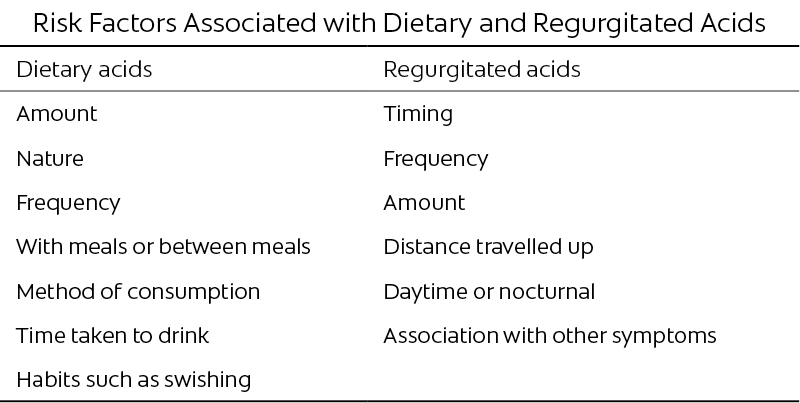
Diagnosis of erosive tooth wear includes not only information about patients’ complaints and concerns, but a thorough investigation of their lifestyle. This includes assessment of their diet in a holistic manner, including consumption of foods and drinks that are erosive, as well as those that are refluxogenic. The dietary analysis needs to be comprehensive and include all the risk factors; these are listed in Table 5. Some important points are snacking, sipping and swishing of erosive drinks, as well as frequency and amount consumed. In terms of regurgitated acids, questions should be asked regarding when, how often, and how far up the acid travels. Patients’ stress levels in relation to possible bruxism, lifestyle in terms of exercise, and other routines and various habits need to be thoroughly analyzed. One area of debate is the importance of delaying tooth brushing after the consumption of an acidic food or drink. Salivary remineralization after exposure to acids has been suggested to offer some protection, hence delaying tooth brushing after consumption of acids has been suggested.
That said, there is laboratory evidence to suggest that full remineralization of eroded dental tissues may not occur in a timely manner to be protective. A recent pan-European epidemiological study failed to observe clear patterns between timing of food intake and tooth brushing. This is an area in need of further research. 6Bartlett DW, Lussi A, West NX, et al. Prevalence of tooth wear on buccal and lingual surfaces and possible risk factors in young European adults. J Dent 2013;41:1007-13.,22Attin T, Knöfel S, Buchalla W, Tütüncü R. In situ evaluation of different remineralization periods to decrease brushing abrasion of demineralized enamel. Caries Res 2001;35:216-22.,23Jaeggi T, Lussi A. Prevalence, Incidence and Distribution of Erosion. In: Erosive Tooth Wear Volume 25, Lussi A, Ganss C, eds. Basel, Karger, pp. 55-74, 2014.,24Ganss C, Schlueter N, Friedrich D, Klimek J. Efficacy of waiting periods and topical fluoride treatment on toothbrush abrasion of eroded enamel in situ. Caries Res 2007;41:146-51.,25Lussi A, Lussi J, Carvalho TS, Cvikl B. Tooth brushing after an erosive attack: will waiting avoid tooth wear? Eur J Oral Sci 2014;122(5):353-9.Examination includes assessments of signs and symptoms of TMJ dysfunction, general assessment of the health of the soft and hard tissues, and the occlusion. More specifically, the wear facets need to be examined and assessed. Points to consider are the position, distribution, number, and shape of the facets, and whether the corresponding upper and lower facets meet and fit together (Figures 2–6).
Figure 5.
Wear facets due to a combination of attrition and erosion. There are corresponding wear facets due mainly to attrition and those that do not correspond due to erosive wear.
Clinical Indices
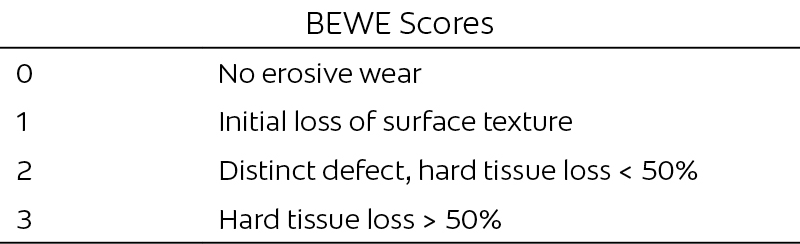
There are a number of indices to help assess the severity of erosive tooth wear. Some indices score erosion in isolation while others assess tooth wear regardless of the etiology. 26Eccles JD. Dental erosion of nonindustrial origin. A clinical survey and classification. J Prosthet Dent 1979;42:649-53.,27Smith BGN, Knight JK. An index for measuring the wear of teeth. Br Dent J 1984;156: 435–8 Within the last 10 years a new scoring system, the BEWE (Basic Erosive Wear Examination), was developed that uses a similar concept to the Basic Periodontal Examination (BPE) used in periodontal disease assessment. The index is designed for use in general practice to assess and record the presence and severity of erosive tooth wear, and not meant to be an accurate and reproducible assessment of all the facets, much in the same way as BPE is used. This is then followed by the necessary preventive measures being put into place. The index uses a 4-point scale, 0–3 (Table 6), where 0 is no erosive wear and 3 is hard tissue loss involving greater than 50% of the surface being scored. 28Bartlett D, Ganss C, Lussi A. Basic Erosive Wear Examination (BEWE): a new scoring system for scientific and clinical needs. Clin Oral Investig 2008;12 (Suppl 1):S65–8.
Other Investigations
Management of Erosive Tooth Wear
Management Goals
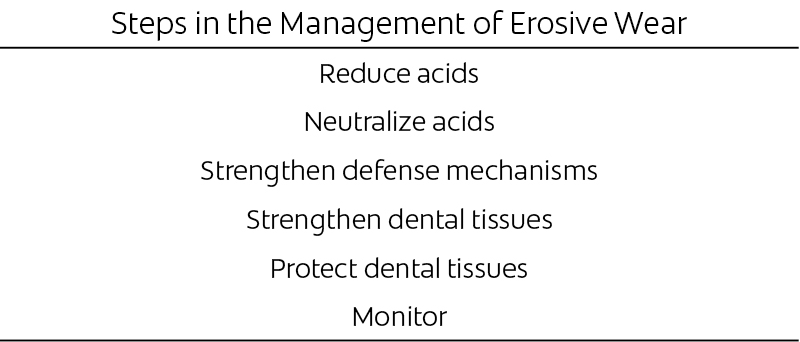
Management of most dental conditions is changing, with research concentrating on prevention and minimally invasive approaches to treatment. Erosive tooth wear is no exception, and, in fact, recent research and our further understanding of the processes emphasize the importance of this approach. This, together with the complicated nature of any restorative treatment of teeth affected by erosive tooth wear, means that the word management is a more suitable term than treatment for most cases. The aims of minimally invasive management of erosive tooth wear are listed in Table 7.
Reduction and Neutralization of Acids
Reduction and neutralization of acids can be achieved first by means of diagnosis and identification of the source of acid to reduce the contact time between the acids and enamel/dentin. Some of these have been mentioned previously, e.g., reduction of frequency of intake, avoiding snacking outside meal times, and swallowing the drink without swishing in the mouth. Regurgitated acids can also be reduced by simple lifestyle adjustments. Consumption of reflux-ogenic foods, such as fatty foods, spicy foods, onions, and pickles, should be reduced. Advice can also be given regarding reducing the consumption of alcohol and avoiding intake of large meals, in particular shortly before going to bed. Treatment of GERD is mainly by the use of medications including over-the-counter antacids or more effectively by the use of proton pump inhibitors (PPIs). These medications are highly effective in the control of reflux and regurgitated acids, but like most medications have side effects. Concerns have been raised regarding long-term PPI therapy, including increased susceptibility to gastrointestinal and respiratory infections and risk of hip fracture. It is therefore highly desirable to consider non-medical methods to control acid reflux. 30Yang YX, Lewis JD, Epstein S, Metz DC. Long-term proton pump inhibitor therapy and risk of hip fracture. JAMA 2006; 296:2947-53.,31Laheij RJ, Sturkenboom MC, Hassing RJ, Dieleman J, Stricker BH, Jansen JB. Risk of community-acquired pneumonia and use of gastric acid-suppressive drugs. Jama 2004; 292:1955-60.,32Pereira SP, Gainsborough N, Dowling RH. Drug-induced hypochlorhydria causes high duodenal bacterial counts in the elderly. Aliment Pharmacol Ther 1998;12:99-104.
The Role of Saliva and Pellicle
The role of saliva and pellicle has been highlighted in recent research. Natural saliva is the most important inherent factor in the prevention of demineralization and facilitating remineralization in the processes involved in erosive wear. Saliva dilutes, neutralizes, and buffers acids. This results in the removal and reduction of acids in the oral cavity, but also the neutralization of any remaining acids. 33Hara AT, Zero DT. The potential of saliva in protecting against dental erosion. Monogr Oral Sci 2014;25:197-205.,34Zwier N, Huysmans MC, Jager DH, Ruben J, Bronkhorst EM, Truin GJ. Saliva parameters and erosive wear in adolescents. Caries Res 2013;47:548-52.,35Hannig, M, Hannig C. The pellicle and erosion. Monogr Oral Sci 2014;25:206-14.,36Carpenter G, Cotroneo E, Moazzez R, Rojas-Serrano M, Donaldson N, Austin R, Zaidel L, Bartlett D, Proctor G. Composition of enamel pellicle from dental erosion patients. Caries Res 2014;48:361-7.,37Lussi A, Schluete N, Rakhmatullina E, Ganss C. Dental erosion–an overview with emphasis on chemical and histopathological aspects. Caries Res 2011;45(Suppl1):2-12. Because of its inorganic components, another important role for saliva is to help remineralize enamel, although a complete remineralization is unlikely. 38Moazzez R, Bartlett D, Anggiansah A. The effect of chewing sugar-free gum on gastro-esophageal reflux. J Dent Res 2005;84:1062-5.,39Smoak BR, Koufman JA. Effects of gum chewing on pharyngeal and esophageal pH. Ann Otol Rhinol Laryngol 2001;110:1117-9.
Saliva also has a key role in the formation of acquired pellicle on the tooth surface, which starts immediately after tooth brushing. The important role of pellicle against erosive tooth wear has been shown in the literature. However, the preventive potential of pellicle varies between individuals and various formed pellicles. Studies have shown the differences in composition of pellicle proteins between individuals with and without erosion. 33Hara AT, Zero DT. The potential of saliva in protecting against dental erosion. Monogr Oral Sci 2014;25:197-205.,34Zwier N, Huysmans MC, Jager DH, Ruben J, Bronkhorst EM, Truin GJ. Saliva parameters and erosive wear in adolescents. Caries Res 2013;47:548-52.,35Hannig, M, Hannig C. The pellicle and erosion. Monogr Oral Sci 2014;25:206-14.,36Carpenter G, Cotroneo E, Moazzez R, Rojas-Serrano M, Donaldson N, Austin R, Zaidel L, Bartlett D, Proctor G. Composition of enamel pellicle from dental erosion patients. Caries Res 2014;48:361-7.,37Lussi A, Schluete N, Rakhmatullina E, Ganss C. Dental erosion–an overview with emphasis on chemical and histopathological aspects. Caries Res 2011;45(Suppl1):2-12. Stimulation of saliva to increase the flow rate and improve its buffering capacity can, therefore, be a preventive approach in the management of erosive wear, both in cases of dietary erosion and GERD. Previous work has shown the possible use of chewing gum as a simple method of reducing and neutralizing acids with some promising results. Future work and product development can also be aimed at modifying pellicle to enhance its protective potential. 40O’Toole S, Bartlett DW, Moazzez R. Efficacy of sodium and stannous fluoride mouthrinses when used before single and multiple erosive challenges. Aust Dent J 2016 [Epub ahead of print].,41O’Toole S, Mistry M, Mutahar M, Moazzez R, Bartlett D. Sequence of stannous and sodium fluoride solutions to prevent enamel erosion. J Dent 2015;43:1498-1503.
Strengthening Dental Tissues
Strengthening the dental tissues can be achieved by various available products. The role of fluoride-containing products has been investigated in enamel, with promising results. This is important in the reversal and remineralization of early erosion. The role of fluoride-containing products in cases of dentin exposure has not been shown as effectively as enamel, although this area needs further research. There has been an increased focus by various oral health companies on the development of products to target erosive wear. The mode of action of fluorides is very similar to caries in terms of reversal of demineralization and influencing remineralization, hence resulting in hardening of the surface.Recent work has further suggested that various formulations of fluoride-containing products could have differing outcomes. Sodium and stannous-containing fluorides have been cited as being effective. The use of products containing high levels of fluoride has also been advocated. Various other products, such as tooth mousse, have also been specially formulated for this effect. 42Sundaram G, Bartlett, Watson T. Bonding to and protecting worn palatal surfaces of teeth with dentine bonding agents. J Oral Rehabil 2004;31:505-9.,43Bartlett D, Sundaram G, Moazzez R. Trial of protective effect of fissure sealants, in vivo, on the palatal surfaces of anterior teeth, in patients suffering from erosion. J Dent 2011;39:26-9.
Protection of the Tooth Surface
Monitoring
Treatment
The most common reason for treatment is patient-driven due to the appearance. Once the wear becomes severe there are other indications, such as the preservation of the structural integrity of the tooth and problems associated with restoration of a short clinical crown.Restorative treatment of teeth affected by erosive wear is complicated and time consuming. The main issues are the large number of teeth involved, as well as dento-alveolar compensation. This results in the loss of space for restorations. Generally speaking, erosive wear can be categorized into local or general wear. Localized wear most commonly tends to affect the upper anterior teeth, although in some cases, due to particular habits or the direction of travel of the refluxate, acids can only affect a couple of posterior teeth. Generalized wear tends to affect many anterior and posterior teeth. In terms of restorative treatment, the treatment concepts are discussed separately.
Localized Wear
Wear facets affecting areas such as the labial or buccal surfaces that are not in occlusion can simply be restored using composite restorations or veneers (direct or indirect). The problem arises when the wear is on the palatal surfaces of upper anterior teeth or occlusal surfaces of posterior teeth. In these cases, as most often no space is present for any restorations, the most common approach is to use the Dahl principle. As teeth wear down they become shorter, but contact is maintained through dento-alveolar compensation. In the 1980s, the concept of a Dahl appliance was introduced with the aim of reversing this compensation and, hence, recreating the space needed for restoration. This principle is often used when the palatal surfaces of upper anterior teeth have been affected. These surfaces are built up using composite resin to gain the necessary space. Initially the only teeth in contact are the anterior teeth, but the anterior teeth intrude and the posterior teeth extrude and allow posterior tooth contacts to be regained, leaving a space for restoration of the affected surfaces. In some instances the restorations can remain and no further treatment is necessary (Figure 6). In other cases the teeth may need to be crowned. The Dahl principle is effective in most cases, but on the rare occasions that it is not, other restorative options need to be pursued. 45Dahl BL, Krogstad O. Long-term observations of an increased occlusal face height obtained by a combined orthodontic/prosthetic approach. J Oral Rehabil 1985;12:173-6.
Generalized Wear
In cases where the wear affects several anterior and posterior teeth, the restorative procedures are more complicated, often requiring reorganization of the occlusion, change in the occlusal plane, occlusal plane, occlusal vertical dimension (OVD), and full mouth rehabilitation. This usually results in restoration of most, if not all the teeth. In some cases, due to the resulting short clinical crowns, crown lengthening surgery is also indicated. Further expansion on these procedures is beyond the scope if this article; needless to say, this option should be attempted as a last resort. This is due to problems with longevity of restorations and need for replacement, and the destructive nature of the treatment.In terms of materials, the two concepts are adhesive materials without need for much preparation, or crowns. The advantages of composite restorations are their conservative nature and effects of bonding and, hence, strengthening the remaining tooth tissues. However, composite restorations can stain and the longevity of the restorations has been shown to be less than crowns.
Conclusion
Future developments through further research are promising as we gain a better understanding of the processes involved in erosive wear and the role of saliva and pellicle, better diagnostic methods, better methods of in vivo monitoring including intraoral scanners and newly developed and targeted products for prevention and re-hardening/remineralization. The aim should be correct diagnosis and prevention in order to avoid structural damage and loss of tooth tissue that may lead to extensive restorative treatment.
References
- 1.Washington Post Staff. “The Opioid Files: Follow the Post’s Investigation of the Opiod Epidemic.” The Washington Post. 13 Sep 2013. https://www.washingtonpost.com/national/2019/07/20/opioid-files/?arc404=true.
- 2.Schroeder AR, Dehghan M, Newman TB, Bentley JP, Park KT. Association of Opioid Prescriptions From Dental Clinicians for US Adolescents and Young Adults With Subsequent Opioid Use and Abuse. JAMA Intern Med 2019;179:145-152.
- 3.Suda KJ, Durkin MJ, Calip GS, et al. Comparison of opioid prescribing by dentists in the united states and england. JAMA Netw Open 2019;2:e194303.
- 4.Dana R, Azarpazhooh A, Laghapour N, Suda KJ, Okunseri C. Role of dentists in prescribing opioid analgesics and antibiotics: an overview. Dent Clin North Am 2018;62:279-294.
- 5.Jimoh KO, Matthews DC, Brillant M, Sketris I. Pattern of opioid analgesic prescription for adults by dentists in Nova Scotia, Canada. JDR Clin Trans Res 2018;3:203-211.
- 6.Falk J, Friesen KJ, Magnusson C, Schroth RJ, Bugden S. Opioid prescribing by dentists in Manitoba, Canada: A longitudinal analysis. J Am Dent Assoc 2019;150:122-129.
- 7.Halling F, Heymann P, Ziebart T, Neff A. Analgesic prescribing patterns of dental practitioners in Germany. J Craniomaxillofac Surg 2018;46:1731-1736.
- 8.Teoh L, Stewart K, Marino RJ, McCullough MJ. Part 2. Current prescribing trends of dental non-antibacterial medicines in Australia from 2013 to 2016. Aust Dent J 2018.
- 9.Lino PA, Sohn W, Singhal A, Martins MAP, Silva M, Abreu M. A national study on the use of opioid analgesics in dentistry. Braz Oral Res 2019;33:e076.
- 10.Obadan-Udoh E, Lupulescu-Mann N, Charlesworth CJ, et al. Opioid prescribing patterns after dental visits among beneficiaries of Medicaid in Washington state in 2014 and 2015. J Am Dent Assoc 2019;150:259-268 e251.
- 11.Janakiram C, Chalmers NI, Fontelo P, et al. Sex and race or ethnicity disparities in opioid prescriptions for dental diagnoses among patients receiving Medicaid. J Am Dent Assoc 2018;149:246-255.
- 12.Koppen L, Suda KJ, Rowan S, McGregor J, Evans CT. Dentists’ prescribing of antibiotics and opioids to Medicare Part D beneficiaries: Medications of high impact to public health. J Am Dent Assoc 2018;149:721-730.
- 13.McCauley JL, Reyes S, Meyerowitz C, et al. Training experiences regarding pain management, addiction, and drug diversion of dentists enrolled in the National Dental Practice-Based Research Network. Subst Abus 2019:1-6.
- 14.McCauley JL, Gilbert GH, Cochran DL, et al. Prescription Drug Monitoring Program use: National Dental PBRN results. JDR Clin Trans Res 2019;4:178-186.
- 15.McCauley JL, Leite RS, Gordan VV, et al. Opioid prescribing and risk mitigation implementation in the management of acute pain: results from The National Dental Practice-Based Research Network. J Am Dent Assoc 2018;149:353-362.
- 16.McCauley JL, Nelson JD, Gilbert GH, et al. Prescription drug abuse among patients in rural dental practices reported by members of the National Dental PBRN. J Rural Health 2019.
- 17.Sun BC, Lupulescu-Mann N, Charlesworth CJ, et al. Variations in prescription drug monitoring program use by prescriber specialty. J Subst Abuse Treat 2018;94:35-40.
- 18.Tompach PC, Wagner CL, Sunstrum AB, Nadeau RA, Tu HK. Investigation of an opioid prescribing protocol after third molar extraction procedures. J Oral Maxillofac Surg 2019;77:705-714.
- 19.Matthews DC, Brillant MGS, Jimoh KO, Singleton W, McLean-Veysey P, Sketris I. Patterns of opioid prescribing by dentists in a pediatric population: a retrospective observational study. CMAJ Open 2019;7:E497-E503.
- 20.Alghofaily M, Romberg E, Aldahmash S, Tordik PA. Opioid-prescribing habits of practitioner and educator members of the American Association of Endodontists: report of a national survey. J Endod 2019;45:1265-1271.
- 21.Schroeder PL, Filler SJ, Ramirez B, et al. Dental erosion and acid reflux dis-ease. Ann Intern Med 1995;122:809-15.
- 22.Attin T, Knöfel S, Buchalla W, Tütüncü R. In situ evaluation of different remineralization periods to decrease brushing abrasion of demineralized enamel. Caries Res 2001;35:216-22.
- 23.Jaeggi T, Lussi A. Prevalence, Incidence and Distribution of Erosion. In: Erosive Tooth Wear Volume 25, Lussi A, Ganss C, eds. Basel, Karger, pp. 55-74, 2014.
- 24.Ganss C, Schlueter N, Friedrich D, Klimek J. Efficacy of waiting periods and topical fluoride treatment on toothbrush abrasion of eroded enamel in situ. Caries Res 2007;41:146-51.
- 25.Lussi A, Lussi J, Carvalho TS, Cvikl B. Tooth brushing after an erosive attack: will waiting avoid tooth wear? Eur J Oral Sci 2014;122(5):353-9.
- 26.Eccles JD. Dental erosion of nonindustrial origin. A clinical survey and classification. J Prosthet Dent 1979;42:649-53.
- 27.Smith BGN, Knight JK. An index for measuring the wear of teeth. Br Dent J 1984;156: 435–8
- 28.Bartlett D, Ganss C, Lussi A. Basic Erosive Wear Examination (BEWE): a new scoring system for scientific and clinical needs. Clin Oral Investig 2008;12 (Suppl 1):S65–8.
- 29.Rey E, Barceló M, Zapardiel J, Sobreviela E, Muñoz M,Díaz-Rubio. Is the reflux disease questionnaire useful for identifying GERD according to the Montreal definition? MBMC Gastroenterol 2014;14:17.
- 30.Yang YX, Lewis JD, Epstein S, Metz DC. Long-term proton pump inhibitor therapy and risk of hip fracture. JAMA 2006; 296:2947-53.
- 31.Laheij RJ, Sturkenboom MC, Hassing RJ, Dieleman J, Stricker BH, Jansen JB. Risk of community-acquired pneumonia and use of gastric acid-suppressive drugs. Jama 2004; 292:1955-60.
- 32.Pereira SP, Gainsborough N, Dowling RH. Drug-induced hypochlorhydria causes high duodenal bacterial counts in the elderly. Aliment Pharmacol Ther 1998;12:99-104.
- 33.Hara AT, Zero DT. The potential of saliva in protecting against dental erosion. Monogr Oral Sci 2014;25:197-205.
- 34.Zwier N, Huysmans MC, Jager DH, Ruben J, Bronkhorst EM, Truin GJ. Saliva parameters and erosive wear in adolescents. Caries Res 2013;47:548-52.
- 35.Hannig, M, Hannig C. The pellicle and erosion. Monogr Oral Sci 2014;25:206-14.
- 36.Carpenter G, Cotroneo E, Moazzez R, Rojas-Serrano M, Donaldson N, Austin R, Zaidel L, Bartlett D, Proctor G. Composition of enamel pellicle from dental erosion patients. Caries Res 2014;48:361-7.
- 37.Lussi A, Schluete N, Rakhmatullina E, Ganss C. Dental erosion–an overview with emphasis on chemical and histopathological aspects. Caries Res 2011;45(Suppl1):2-12.
- 38.Moazzez R, Bartlett D, Anggiansah A. The effect of chewing sugar-free gum on gastro-esophageal reflux. J Dent Res 2005;84:1062-5.
- 39.Smoak BR, Koufman JA. Effects of gum chewing on pharyngeal and esophageal pH. Ann Otol Rhinol Laryngol 2001;110:1117-9.
- 40.O’Toole S, Bartlett DW, Moazzez R. Efficacy of sodium and stannous fluoride mouthrinses when used before single and multiple erosive challenges. Aust Dent J 2016 [Epub ahead of print].
- 41.O’Toole S, Mistry M, Mutahar M, Moazzez R, Bartlett D. Sequence of stannous and sodium fluoride solutions to prevent enamel erosion. J Dent 2015;43:1498-1503.
- 42.Sundaram G, Bartlett, Watson T. Bonding to and protecting worn palatal surfaces of teeth with dentine bonding agents. J Oral Rehabil 2004;31:505-9.
- 43.Bartlett D, Sundaram G, Moazzez R. Trial of protective effect of fissure sealants, in vivo, on the palatal surfaces of anterior teeth, in patients suffering from erosion. J Dent 2011;39:26-9.
- 44.Dahl BL, Krogstad O, Karlsen K. An alternative treatment of cases with advanced localised attrition. J Oral Rehabil 1975;2:209-14.
- 45.Dahl BL, Krogstad O. Long-term observations of an increased occlusal face height obtained by a combined orthodontic/prosthetic approach. J Oral Rehabil 1985;12:173-6.


:sharpen(level=0):output(format=jpeg)/up/2023/05/Rebecca-Moazzez-1.jpg)
:sharpen(level=0):output(format=jpeg)/up/2017/06/Diagnosis-and-Minimally-Invasive-Management-of-Erosive-Tooth-Wear-2.jpg)