Identification of Carotid Artery Calcifications in Panoramic Dental Radiographs
Atherosclerosis, and the resulting cardiovascular and cerebrovascular diseases (CVD), are the major cause of morbidity and mortality in the developed world1Chen S, Kuhn M, Prettner K, Bloom DE. The macroeconomic burden of noncommunicable diseases in the United States: Estimates and projections. PLoS One 2018;13:e0206702.,2Collaborators GBDLRoS, Feigin VL, Nguyen G, et al. Global, Regional, and Country-Specific Lifetime Risks of Stroke, 1990 and 2016. N Engl J Med 2018;379:2429-2437.. Concepts regarding the pathogenesis of atherosclerotic disease have changed dramatically over the past 25 years. While elevated concentration of cholesterol, primarily low-density lipoprotein, is recognized as an important risk factors for CVD, the mechanisms that explain the development of atheromas have been elucidated and clearly point to the importance of an inflammatory response to the development of atherosclerotic lesions. The specific steps in the development of these lesions were defined and illustrated in a classic review by Russell Ross, published in 19993Ross R. Atherosclerosis is an inflammatory disease. Am Heart J 1999;138:S419-420.. As an interesting sidebar, Russell Ross was originally trained as a dentist, graduating from the Columbia University School of Dental and Oral Surgery (now the Columbia University College of Dental Medicine).
The stages of atheroma development are:
- Initial endothelial dysfunction: the cells that line the arteries become more permeable to lipoproteins
- Formation of fatty streaks: monocytes/macrophages, which are derived from the blood stream, become laden with lipids, and accumulate just below the endothelial cell layer. Lymphocytes and smooth muscle cells also are present in the fatty streaks.
- Atherosclerotic lesion development: the fatty streaks progress and become more complex. The more advanced lesions are characterized by formation of a fibrous cap, which is an attempt to isolate the lesion from the arterial lumen.
- Unstable atherosclerotic lesion: as this lesion becomes more complex, the cap may thin in certain areas, which can cause rupture and then thrombosis.
Calcification within these atherosclerotic lesions is fairly common, and then these lesions are identifiable on standard radiographs. The significance of coronary and other artery calcifications is still being studied, but this finding is seen in persons with CVD and has been associated with increased risk for adverse cardiovascular events4Margolis JR, Chen JT, Kong Y, Peter RH, Behar VS, Kisslo JA. The diagnostic and prognostic significance of coronary artery calcification. A report of 800 cases. Radiology 1980;137:609-616..
There is great interest in the relationship of oral disease and CVD. This has primarily focused on the role of periodontal infection and subsequent inflammation as a risk factor for CVD5Chapple IL, Genco R, working group 2 of the joint EFPAAP workshop. Diabetes and periodontal diseases: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J Periodontol 2013;84:S106-112.. However, studies have also examined another aspect of the relationship of dentistry and CVD: the identification of calcification in the carotid arteries as detected in panoramic radiographs (CCPR), initially described by Friedlander and Lande in 19816Friedlander AH, Lande A. Panoramic radiographic identification of carotid arterial plaques. Oral Surg Oral Med Oral Pathol 1981;52:102-104.. Evaluating 1,000 films, 2% of patients were identified as having CCPR. A publication by Friedlander and Gratt reported on 6 patients with bilateral calcification, and using thermography and ultrasound confirmed that patients with calcifications had lower facial skin temperatures consistent with reduced blood flow and perfusion, and reduced diameter of the vessel lumen7Friedlander AH, Gratt BM. Panoramic dental radiography as an aid in detecting patients at risk for stroke. J Oral Maxillofac Surg 1994;52:1257-1262.. Subsequently, many additional studies have examined the occurrence of plaques in the carotid arteries detected in dental panoramic radiographs.
The prevalence of CCPR has been studied in a variety of populations. Friedlander and Friedlander8Friedlander AH, Friedlander IK. Identification of stroke prone patients by panoramic radiography. Aust Dent J 1998;43:51-54. noted that atherosclerotic lesions of the carotid artery occur at the bifurcation of the common carotid, and when these lesions are calcified they can appear on panoramic radiographs as nodular calcifications or as vertical radiopacities. They stressed the need for careful evaluation of these films in patients who are at risk for CVD, including older individuals and those with other risk factors such as being overweight, smoking, hypercholesterolemia and having a diagnosis of diabetes mellitus.
A review of studies published between 1981 and 2003 indicated a general prevalence of CCPR between 3% and 5%, with increased prevalence associated with the presence of identified risk factors9Almog DM, Illig KA, Carter LC, Friedlander AH, Brooks SL, Grimes RM. Diagnosis of non-dental conditions. Carotid artery calcifications on panoramic radiographs identify patients at risk for stroke. N Y State Dent J 2004;70:20-25.. A later review published in 2016 emphasized the association of CCPR with stroke (cerebrovascular hemorrhage and ischemia). This review stressed that the identification of these calcifications can result in early diagnosis and intervention10Borba DL, Hipolito UV, Pereira YCL. Early diagnosis of atherosclerosis with panoramic radiographs: a review. J Vasc Bras 2016;15:302-307. .
Studies of patients with specific risk factors can help clinicians identify patients who should be carefully evaluated for CCPR.
Cardiovascular disease and stroke: In a study of more than 4000 subjects 50 years of age and older who received both medical and dental examinations, 6.2% demonstrated calcification in the carotid artery as visualized on a panoramic radiograph11Lee JS, Kim OS, Chung HJ, et al. The prevalence and correlation of carotid artery calcification on panoramic radiographs and peripheral arterial disease in a population from the Republic of Korea: the Dong-gu study. Dentomaxillofac Radiol 2013;42:29725099. . This population had a prevalence of peripheral artery disease of 2.6%. Persons with CCPR had a greater prevalence of peripheral artery disease versus persons without carotid calcification (5.5% versus 2.4%). Further, regression analysis indicated than if a carotid calcification was present, the odds ratio of having peripheral artery disease was 1.84, after full adjustment for confounders. Another study examined panoramic radiographic findings in persons who had been diagnosed with carotid stenosis of at least 50%. 84% of patients demonstrated calcification of the carotids observed in panoramic radiographs12Garoff M, Johansson E, Ahlqvist J, Jaghagen EL, Arnerlov C, Wester P. Detection of calcifications in panoramic radiographs in patients with carotid stenoses >/=50%. Oral Surg Oral Med Oral Pathol Oral Radiol 2014;117:385-391.. Further, an association of CCPR and a history of recent myocardial infarction has been reported 13Gustafsson N, Ahlqvist JB, Naslund U, et al. Calcified carotid artery atheromas in panoramic radiographs are associated with a first myocardial infarction: a case-control study. Oral Surg Oral Med Oral Pathol Oral Radiol 2018;125:199-204 e191.. More than a third of patients with a history of myocardial infarction had coronary calcification (33.8%) vs. 27.6% for controls without an infarct. Nevertheless, a study comparing the ability of panoramic radiographs to detect carotid artery calcifications as confirmed by carotid doppler sonography only observed a sensitivity of 66.6% (a measure of the percent of true positives that are correctly identified). The authors concluded that panoramic radiography is not a reliable method of identifying calcifications of the carotid 14Khosropanah SH, Shahidi SH, Bronoosh P, Rasekhi A. Evaluation of carotid calcification detected using panoramic radiography and carotid Doppler sonography in patients with and without coronary artery disease. Br Dent J 2009;207:E8; discussion 162-163.. It is important to emphasize, however, that studies reporting carotid calcifications in panoramic radiographs do not propose this finding as diagnostic for all such calcifications.
Diabetes mellitus and the metabolic syndrome: The prevalence of CCPR was observed to be much higher in non-insulin dependent patients with diabetes (now type 2 diabetes; 24%) and insulin-dependent patients with diabetes (now type 1 diabetes; 36%) as compared to the 4% prevalence in a general population 15Friedlander AH, Garrett NR, Norman DC. The prevalence of calcified carotid artery atheromas on the panoramic radiographs of patients with type 2 diabetes mellitus. J Am Dent Assoc 2002;133:1516-1523.. Further, the prevalence of CCPR was much higher in individuals with the metabolic syndrome (an important group of metabolic findings associated with an elevated risk for developing diabetes mellitus and cardiovascular disease) than the general population 16Pornprasertsuk-Damrongsri S, Virayavanich W, Thanakun S, Siriwongpairat P, Amaekchok P, Khovidhunkit W. The prevalence of carotid artery calcifications detected on panoramic radiographs in patients with metabolic syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:e57-62.. In this study, calcifications were detected in 22.4% of the patients.
Chronic kidney disease: An early study observed a higher percentage of CCPR in patients on hemodialysis, and those receiving a kidney transplant, versus age- matched systemically healthy controls 17Kansu O, Ozbek M, Avcu N, Genctoy G, Kansu H, Turgan C. The prevalence of carotid artery calcification on the panoramic radiographs of patients with renal disease. Dentomaxillofac Radiol 2005;34:16-19.. A report evaluating CCPR in patients with end-stage renal disease who were treated with peritoneal dialysis observed a very high prevalence (27.4%; 18Gokce C, Sisman Y, Sipahioglu M, et al. The prevalence of carotid artery calcification on the panoramic radiographs of end-stage renal disease patients with peritoneal dialysis: do incidental findings provide life-saving information? J Int Med Res 2008;36:47-53.). Another study of patients with chronic kidney disease treated with dialysis revealed that 15.9% demonstrated CCPR. Risk factors for CCPR in patients with chronic kidney disease included older age, being female, having diabetes mellitus, and having required hemodialysis for longer periods of time 19Maia PRL, Medeiros AMC, Pereira HSG, Lima KC, Oliveira PT. Presence and associated factors of carotid artery calcification detected by digital panoramic radiography in patients with chronic kidney disease undergoing hemodialysis. Oral Surg Oral Med Oral Pathol Oral Radiol 2018;126:198-204..
Menopause: Evaluations of a cohort of older African-American women who were military veterans, and either had CCPR or did not, revealed that those with calcifications had a greater chance of having calcifications of the aortic arch (as determined by a chest radiograph) than those that did not have a positive finding on a panoramic radiograph. This relationship was observed for postmenopausal women (>60 years of age) versus younger women 20Friedlander AH, El-Saden SM, Aghazadehsanai N, Chang TI, Harada ND, Garrett NR. Association of calcified carotid atheromas visualized on panoramic images and aortic arch calcifications seen on chest radiographs of postmenopausal women. J Am Dent Assoc 2014;145:345-351.. A subsequent larger study by these same investigators21Aghazadehsanai N, Chang TI, Garrett NR, Friedlander AH. Prevalence of calcified carotid artery atheromas on digital panoramic images among perimenopausal and postmenopausal African American women. Oral Surg Oral Med Oral Pathol Oral Radiol 2017;123:621-625. of perimenopausal and postmenopausal African- American women (mean age = 58.2 years) demonstrated a prevalence of CCPR of 24%. The presence of a CCPR was correlated with increased age, dyslipidemia and diagnosis of diabetes mellitus.
Periodontitis and tooth loss: A literature review that examined the interrelationship of CCPR, and risk for stroke and the presence of periodontitis, determined there was a higher prevalence of CCPR when periodontitis was present, but concluded that there was a paucity of appropriately designed studies in older adults 22Bengtsson VW, Persson GR, Renvert S. Assessment of carotid calcifications on panoramic radiographs in relation to other used methods and relationship to periodontitis and stroke: a literature review. Acta Odontol Scand 2014;72:401-412.. A subsequent study by the same authors 23Bengtsson VW, Persson GR, Berglund J, Renvert S. A cross-sectional study of the associations between periodontitis and carotid arterial calcifications in an elderly population. Acta Odontol Scand 2016;74:115-120. examined the relationship of carotid calcification to periodontitis in older individuals (age range of 60-96 years). Periodontitis was determined clinically and on the panoramic radiographs (>5mm distance between the cement-enamel junction and alveolar crest at more than 10% of surfaces). There was a high prevalence of CCPR (39.1%) and 18.4% of these individuals had a diagnosis of periodontitis. The relative risk of having a carotid calcification if periodontitis was present was 1.5 (p<0.05). Tooth loss was also been shown to be associated with a higher prevalence of CCPR 24Thanakun S, Pornprasertsuk-Damrongsri S, Izumi Y. C-reactive protein levels and the association of carotid artery calcification with tooth loss. Oral Dis 2017;23:69-77..
Conclusions
If a panoramic film is available, oral health care providers should examine these films for evidence of carotid calcifications. Identification of a suspected calcification should trigger questions to the patient, and likely a referral to a medical provider for further evaluation. Four examples of CCPR are provided in Figure 1.
A longitudinal study of patients who were identified with CCPR, compared to an age and sex-matched control group, had a significantly higher percentage of cardiovascular events (5.6%/yr vs. 2.4%/yr; p=0.004) over the following 5.4 years. However, when other risk factors for such events were considered in a regression model, this difference was not significant. The authors concluded that persons with CCPR will likely have a number of risk factors for cardiovascular disease, and a referral is required, especially if the patient is unaware of their risk. The authors could not determine from the study if the presence of such calcifications could be considered an added risk for future events 25Johansson E, Ahlqvist J, Garoff M, Levring Jaghagen E, Meimermondt A, Wester P. Carotid calcifications on panoramic radiographs: a 5-year follow-up study. Oral Surg Oral Med Oral Pathol Oral Radiol 2015;120:513-520..
Detection of carotid calcifications in panoramic radiographic is not always straightforward. Gustaffson and colleagues13Gustafsson N, Ahlqvist JB, Naslund U, et al. Calcified carotid artery atheromas in panoramic radiographs are associated with a first myocardial infarction: a case-control study. Oral Surg Oral Med Oral Pathol Oral Radiol 2018;125:199-204 e191. demonstrated that general dental practitioners could improve their accuracy of identification with a brief training course that included didactic information and an identification exercise during which 100 panoramic films was reviewed. The Kappa statistic (a measure of agreement) increased from 0.66 to 0.71 after the training exercise (p=0.04). This improvement was maintained one year after the training course.
The available research suggests that while the identification of a unilateral or bilateral CCPR is an important finding by itself, we should consider the identification of this risk factor for CVD as part of the larger interrelationship of oral infection/oral inflammation/oral disease (periodontitis, tooth loss) and the risk for non-communicable chronic diseases. The higher prevalence of CCPR in patients with CVD, diabetes mellitus and chronic kidney disease, each of which has been associated with periodontal disease, is further evidence that oral health care providers must be aware of the general health of their patients, and communicate with other health care providers to improve both the oral health and general health of individuals in their care.
Acknowledgement
Thanks are expressed to Dr. Arthur Friedlander and Dr. Urie Lee, Veterans Administration Greater Los Angeles Healthcare System, for their assistance.
Figure 1 (a-d): Examples of carotid calcifications detected on panoramic radiographs. Both standard (top) and enhanced (bottom) radiographs are provided. Digital enhancement is intended to improve visualization of the carotid calcifications, and is achieved with software provided by the manufacturer. Bilateral calcifications are present in all four patients (arrows).


Figure 1a
68 year old male with a history of hypertension, hyperlipidemia, type 2 diabetes, renal failure and a 15 pack-year smoking habit.
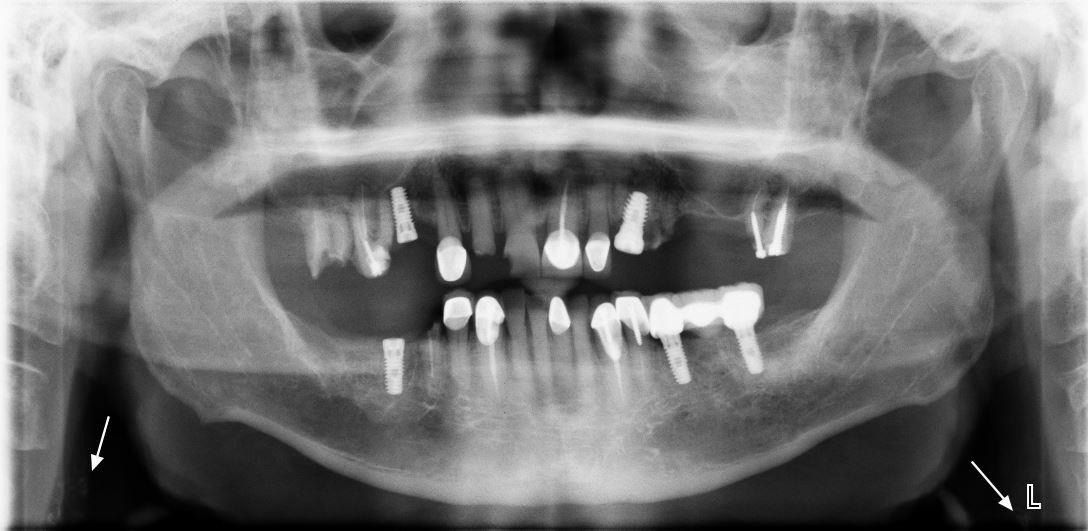

Figure 1b
69 year old male with a history of hypertension, type 2 diabetes, myocardial infarction, obstructive sleep apnea and a 60 pack-year smoking habit.


Figure 1c
71 year old male with a history of hypertension, hyperlipidemia and alcohol dependence
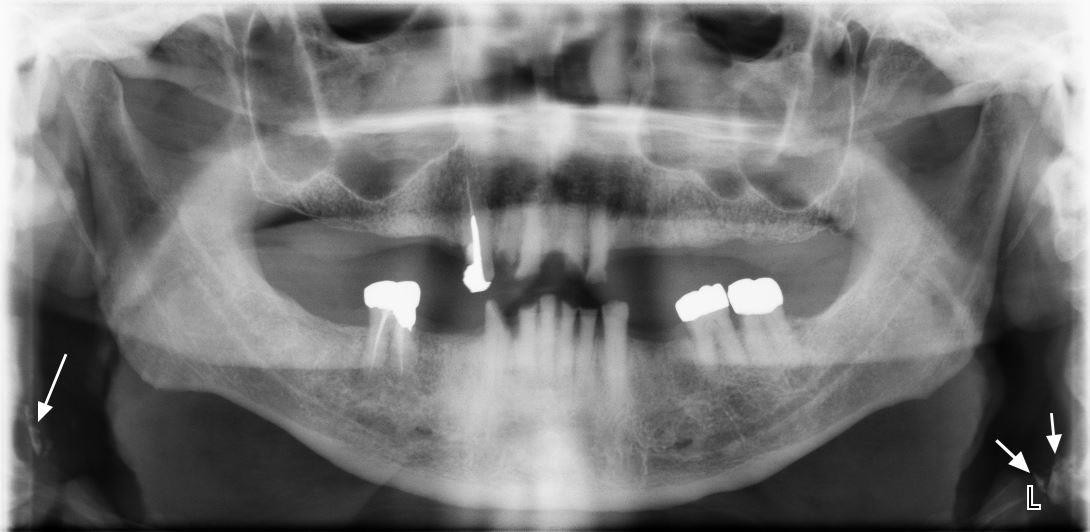
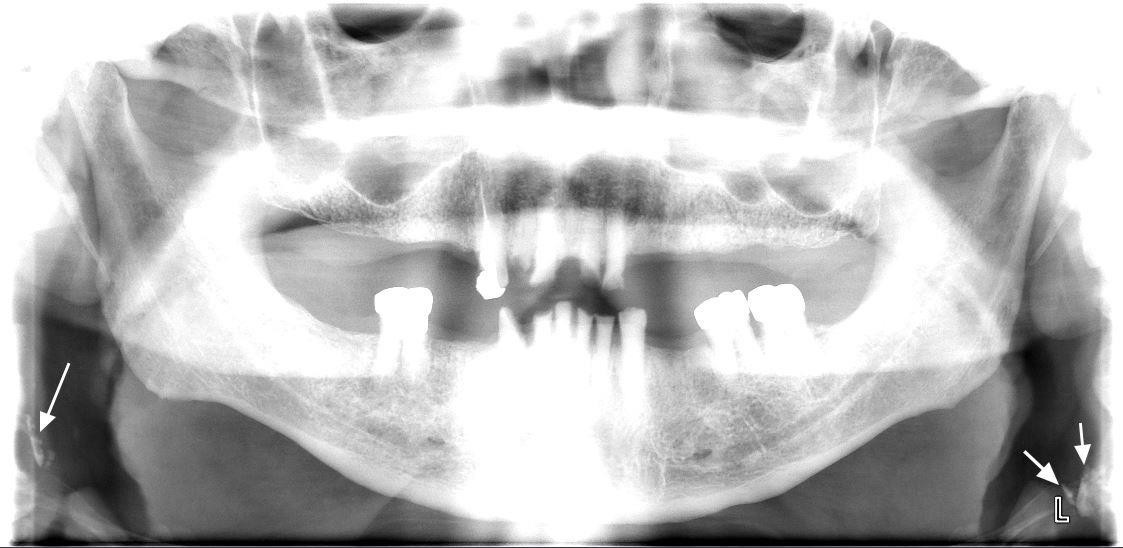
Figure 1d
87 year old male with a history of hypertension, hyperlipidemia, type 2 diabetes, obstructive sleep apnea, renal failure, gout, chronic obstructive pulmonary disease, abdominal aortic aneurysm and a 60 pack-year smoking habit.
References
- 1.Dominy SS, et al. Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Sci Adv. 2019;5(1):eaau3333 https://www.ncbi.nlm.nih.gov/pubmed/30746447.
- 2.Sadrameli M, et al. Linking mechanisms of periodontitis to Alzheimer’s disease. Curr Opin Neurol. 2020;33(2):230-8 https://www.ncbi.nlm.nih.gov/pubmed/32097126.
- 3.Borsa L, et al. Analysis the link between periodontal diseases and Alzheimer’s disease: A systematic review. Int J Environ Res Public Health. 2021;18(17) https://www.ncbi.nlm.nih.gov/pubmed/34501899.
- 4.Costa MJF, et al. Relationship of Porphyromonas gingivalis and Alzheimer’s disease: A systematic review of pre-clinical studies. Clin Oral Investig. 2021;25(3):797-806 https://www.ncbi.nlm.nih.gov/pubmed/33469718.
- 5.Munoz Fernandez SS, Lima Ribeiro SM. Nutrition and Alzheimer disease. Clin Geriatr Med. 2018;34(4):677-97 https://www.ncbi.nlm.nih.gov/pubmed/30336995.
- 6.Aquilani R, et al. Is the Brain Undernourished in Alzheimer’s Disease? Nutrients. 2022;14(9) https://www.ncbi.nlm.nih.gov/pubmed/35565839.
- 7.Fukushima-Nakayama Y, et al. Reduced mastication impairs memory function. J Dent Res. 2017;96(9):1058-66 https://www.ncbi.nlm.nih.gov/pubmed/28621563.
- 8.Kim HB, et al. Abeta accumulation in vmo contributes to masticatory dysfunction in 5XFAD Mice. J Dent Res. 2021;100(9):960-7 https://www.ncbi.nlm.nih.gov/pubmed/33719684.
- 9.Miura H, et al. Relationship between cognitive function and mastication in elderly females. J Oral Rehabil. 2003;30(8):808-11 https://www.ncbi.nlm.nih.gov/pubmed/12880404.
- 10.Lexomboon D, et al. Chewing ability and tooth loss: association with cognitive impairment in an elderly population study. J Am Geriatr Soc. 2012;60(10):1951-6 https://www.ncbi.nlm.nih.gov/pubmed/23035667.
- 11.Elsig F, et al. Tooth loss, chewing efficiency and cognitive impairment in geriatric patients. Gerodontology. 2015;32(2):149-56 https://www.ncbi.nlm.nih.gov/pubmed/24128078.
- 12.Kim EK, et al. Relationship between chewing ability and cognitive impairment in the rural elderly. Arch Gerontol Geriatr. 2017;70:209-13 https://www.ncbi.nlm.nih.gov/pubmed/28214402.
- 13.Kim MS, et al. The association between mastication and mild cognitive impairment in Korean adults. Medicine (Baltimore). 2020;99(23):e20653 https://www.ncbi.nlm.nih.gov/pubmed/32502052.
- 14.Cardoso MG, et al. Relationship between functional masticatory units and cognitive impairment in elderly persons. J Oral Rehabil. 2019;46(5):417-23 https://www.ncbi.nlm.nih.gov/pubmed/30614023.
- 15.Popovac A, et al. Oral health status and nutritional habits as predictors for developing alzheimer’s disease. Med Princ Pract. 2021;30(5):448-54 https://www.ncbi.nlm.nih.gov/pubmed/34348313.
- 16.Park T, et al. More teeth and posterior balanced occlusion are a key determinant for cognitive function in the elderly. Int J Environ Res Public Health. 2021;18(4) https://www.ncbi.nlm.nih.gov/pubmed/33669490.
- 17.Lin CS, et al. Association between tooth loss and gray matter volume in cognitive impairment. Brain Imaging Behav. 2020;14(2):396-407 https://www.ncbi.nlm.nih.gov/pubmed/32170642.
- 18.Kumar S, et al. Oral health status and treatment need in geriatric patients with different degrees of cognitive impairment and dementia: a cross-sectional study. J Family Med Prim Care. 2021;10(6):2171-6 https://www.ncbi.nlm.nih.gov/pubmed/34322409.
- 19.Delwel S, et al. Chewing efficiency, global cognitive functioning, and dentition: A cross-sectional observational study in older people with mild cognitive impairment or mild to moderate dementia. Front Aging Neurosci. 2020;12:225 https://www.ncbi.nlm.nih.gov/pubmed/33033478.
- 20.Da Silva JD, et al. Association between cognitive health and masticatory conditions: a descriptive study of the national database of the universal healthcare system in Japan. Aging (Albany NY). 2021;13(6):7943-52 https://www.ncbi.nlm.nih.gov/pubmed/33739304.
- 21.Galindo-Moreno P, et al. The impact of tooth loss on cognitive function. Clin Oral Investig. 2022;26(4):3493-500 https://www.ncbi.nlm.nih.gov/pubmed/34881401.
- 22.Stewart R, et al. Adverse oral health and cognitive decline: The health, aging and body composition study. J Am Geriatr Soc. 2013;61(2):177-84 https://www.ncbi.nlm.nih.gov/pubmed/23405916.
- 23.Dintica CS, et al. The relation of poor mastication with cognition and dementia risk: A population-based longitudinal study. Aging (Albany NY). 2020;12(9):8536-48 https://www.ncbi.nlm.nih.gov/pubmed/32353829.
- 24.Kim MS, Han DH. Does reduced chewing ability efficiency influence cognitive function? Results of a 10-year national cohort study. Medicine (Baltimore). 2022;101(25):e29270 https://www.ncbi.nlm.nih.gov/pubmed/35758356.
- 25.Ko KA, et al. The Impact of Masticatory Function on Cognitive Impairment in Older Patients: A Population-Based Matched Case-Control Study. Yonsei Med J. 2022;63(8):783-9 https://www.ncbi.nlm.nih.gov/pubmed/35914761.
- 26.Garre-Olmo J. [Epidemiology of Alzheimer’s disease and other dementias]. Rev Neurol. 2018;66(11):377-86 https://www.ncbi.nlm.nih.gov/pubmed/29790571.
- 27.Stephan BCM, et al. Secular Trends in Dementia Prevalence and Incidence Worldwide: A Systematic Review. J Alzheimers Dis. 2018;66(2):653-80 https://www.ncbi.nlm.nih.gov/pubmed/30347617.
- 28.Lopez OL, Kuller LH. Epidemiology of aging and associated cognitive disorders: Prevalence and incidence of Alzheimer’s disease and other dementias. Handb Clin Neurol. 2019;167:139-48 https://www.ncbi.nlm.nih.gov/pubmed/31753130.
- 29.Ono Y, et al. Occlusion and brain function: mastication as a prevention of cognitive dysfunction. J Oral Rehabil. 2010;37(8):624-40 https://www.ncbi.nlm.nih.gov/pubmed/20236235.
- 30.Kubo KY, et al. Masticatory function and cognitive function. Okajimas Folia Anat Jpn. 2010;87(3):135-40 https://www.ncbi.nlm.nih.gov/pubmed/21174943.
- 31.Chen H, et al. Chewing Maintains Hippocampus-Dependent Cognitive Function. Int J Med Sci. 2015;12(6):502-9 https://www.ncbi.nlm.nih.gov/pubmed/26078711.
- 32.Azuma K, et al. Association between Mastication, the Hippocampus, and the HPA Axis: A Comprehensive Review. Int J Mol Sci. 2017;18(8) https://www.ncbi.nlm.nih.gov/pubmed/28771175.
- 33.Chuhuaicura P, et al. Mastication as a protective factor of the cognitive decline in adults: A qualitative systematic review. Int Dent J. 2019;69(5):334-40 https://www.ncbi.nlm.nih.gov/pubmed/31140598.
- 34.Lopez-Chaichio L, et al. Oral health and healthy chewing for healthy cognitive ageing: A comprehensive narrative review. Gerodontology. 2021;38(2):126-35 https://www.ncbi.nlm.nih.gov/pubmed/33179281.
- 35.Tada A, Miura H. Association between mastication and cognitive status: A systematic review. Arch Gerontol Geriatr. 2017;70:44-53 https://www.ncbi.nlm.nih.gov/pubmed/28042986.
- 36.Ahmed SE, et al. Influence of Dental Prostheses on Cognitive Functioning in Elderly Population: A Systematic Review. J Pharm Bioallied Sci. 2021;13(Suppl 1):S788-S94 https://www.ncbi.nlm.nih.gov/pubmed/34447202.
- 37.Tonsekar PP, et al. Periodontal disease, tooth loss and dementia: Is there a link? A systematic review. Gerodontology. 2017;34(2):151-63 https://www.ncbi.nlm.nih.gov/pubmed/28168759.
- 38.Nangle MR, Manchery N. Can chronic oral inflammation and masticatory dysfunction contribute to cognitive impairment? Curr Opin Psychiatry. 2020;33(2):156-62 https://www.ncbi.nlm.nih.gov/pubmed/31895157.
- 39.Nakamura T, et al. Oral dysfunctions and cognitive impairment/dementia. J Neurosci Res. 2021;99(2):518-28 https://www.ncbi.nlm.nih.gov/pubmed/33164225.
- 40.Weijenberg RAF, et al. Mind your teeth-The relationship between mastication and cognition. Gerodontology. 2019;36(1):2-7 https://www.ncbi.nlm.nih.gov/pubmed/30480331.
- 41.Asher S, et al. Periodontal health, cognitive decline, and dementia: A systematic review and meta-analysis of longitudinal studies. J Am Geriatr Soc. 2022;70(9):2695-709 https://www.ncbi.nlm.nih.gov/pubmed/36073186.
- 42.Lin CS. Revisiting the link between cognitive decline and masticatory dysfunction. BMC Geriatr. 2018;18(1):5 https://www.ncbi.nlm.nih.gov/pubmed/29304748.
- 43.Wu YT, et al. The changing prevalence and incidence of dementia over time – current evidence. Nat Rev Neurol. 2017;13(6):327-39 https://www.ncbi.nlm.nih.gov/pubmed/28497805.
- 44.National Psoriasis Foundation. Soriatane (Acitretin). https://www.psoriasis.org/soriatane-acitretin/.
- 45.National Psoriasis Foundation. Current Biologics on the Market. https://www.psoriasis.org/current-biologics-on-the-market/.
- 46.Dalmády S, Kemény L, Antal M, Gyulai R. Periodontitis: a newly identified comorbidity in psoriasis and psoriatic arthritis. Expert Rev Clin Immunol 2020;16(1):101-8. doi: 10.1080/1744666X.2019.1700113.
- 47.Mickenautsch S, Yengopal V. Effect of xylitol versus sorbitol: a quantitative systematic review of clinical trials. Int Dent J 2012;62(4):175-88.
- 48.Rethman MP, Beltrán-Aguilar ED, Billings RJ, Burne RA, Clark M, Donly KJ, Hujoel PP, Katz BP, Milgrom P, Sohn W, Stamm JW, Watson G, Wolff M, Wright T, Zero D, Aravamudhan K, Frantsve-Hawley J, Meyer DM; for the American Dental Association Council on Scientific Affairs Expert Panel on Nonfluoride Caries-Preventive Agents. Nonfluoride caries-preventive agents. Executive summary of evidence-based clinical recommendations. J Am Dent Assoc 2011;142(9):1065-71.
- 49.Milgrom P, Söderling EM, Nelson S, Chi DL, Nakai Y. Clinical evidence for polyol efficacy. Adv Dent Res 2012; 24(2):112-6.
:sharpen(level=0):output(format=jpeg)/up/2023/05/Ira-Lamster-3.jpg)
:sharpen(level=0):output(format=jpeg)/up/2019/06/Carotid-calcification-panoramic-radiography-2.jpg)