Oral Health Literacy
Health literacy and oral health literacy (OHL) are factors in achieving oral and systemic health. By one estimate, limited health literacy costs up to more than $200 billion annually, associated with inadequate personal preventive care and greater use of emergency care.1Vernon JA, Trujillo A, Rosenbaum S, DeBuono B. Low health literacy: implications for national policy. Available at: https://publichealth.gwu.edu/departments/healthpolicy/CHPR/downloads/LowHealthLiteracyReport10_4_07.pdf. OHL is defined as ‘the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate oral health decisions.’2American Dental Association. Health Literacy in Dentistry. Available at: https://www.ada.org/en/public-programs/health-literacy-in-dentistry.,3National Institute of Dental and Craniofacial Research. The invisible barrier: Literacy and its relationship with oral health. J Pub Health Dent 2005;65(3):174-92. Poor health literacy is linked to poor health outcomes,4Baskaradoss JK. Relationship between oral health literacy and oral health status. BMC Oral Health 2018;18:172. Available at: https://doi.org/10.1186/s12903-018-0640-1.,5Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155(2):97-107.,6Horowitz AM, Kleinman DV. Oral health literacy: a pathway to reducing oral health disparities in Maryland. J Public Health Dent 2012;72(Suppl 1):S26-30. and poor OHL to poor oral health. Identifying individuals and communities with poor OHL enables and informs interventions to promote OHL and oral health.
OHL and Oral Health
In a systematic review of 10 cross-sectional studies, a weak association was found for lower parental/caregiver OHL and dental caries in the primary dentition. A lower level of OHL in adults was associated with more missing teeth and clinical attachment loss. Results were inconclusive for treatment needs and dental plaque.7Firmino RT, Ferreira FM, Paiva SM, Granville-Garcia AF, Fraiz FC, Martins CC. Oral health literacy and associated oral conditions: A systematic review. J Am Dent Assoc 2017;148(8):604-13. In a systematic review of 11 studies, dental caries prevalence and experience was greater for children if their parents had low OHL. However, no association was found for oral health behaviors, parental perceptions or dental visits.8Firmino RT, Ferreira FM, Martins CC, Granville-Garcia AF, Fraiz FC, Paiva SM. Is parental oral health literacy a predictor of children’s oral health outcomes? Systematic review of the literature. Int J Paediatr Dent 2018 Jul 8. doi: 10.1111/ipd.12378. In a subsequent review, low OHL was associated with dental anxiety and bottle-feeding at night, while high OHL was associated with greater oral health knowledge.9Firmino RT, Martins CC, Faria LDS, Martins Paiva S, Granville-Garcia AF, Fraiz FC, Ferreira FM. Association of oral health literacy with oral health behaviors, perception, knowledge, and dental treatment related outcomes: a systematic review and meta-analysis. J Public Health Dent 2018 Mar 2. doi: 10.1111/jphd.12266. No association was found for OHL and frequency of dental visits by adults. In addition, results were inconclusive for OHL and dental treatment outcomes, oral health behaviors and oral health perception. Twenty-one of 25 studies were cross-sectional and found to be at high risk of bias.9Firmino RT, Martins CC, Faria LDS, Martins Paiva S, Granville-Garcia AF, Fraiz FC, Ferreira FM. Association of oral health literacy with oral health behaviors, perception, knowledge, and dental treatment related outcomes: a systematic review and meta-analysis. J Public Health Dent 2018 Mar 2. doi: 10.1111/jphd.12266.
Individual studies have found associations for OHL, oral health and health behaviors. In two recent cross-sectional studies, lower OHL in adults was significantly associated with periodontal disease (p<0.015).4Baskaradoss JK. Relationship between oral health literacy and oral health status. BMC Oral Health 2018;18:172. Available at: https://doi.org/10.1186/s12903-018-0640-1.,10Wehmeyer MM, Corwin CL, Guthmiller JM, Lee JY. The impact of oral health literacy on periodontal health status. J Public Health Dent 2014;74(1):80-7. In one study, 8% and 75% of individuals with low OHL had no/mild and severe periodontal disease, respectively.10Wehmeyer MM, Corwin CL, Guthmiller JM, Lee JY. The impact of oral health literacy on periodontal health status. J Public Health Dent 2014;74(1):80-7. In contrast, 27% and 39% of individuals with higher levels of OHL, respectively, had no/mild and severe periodontal disease. (Figure 1) As OHL decreased, adjusted risk for periodontal disease increased. In a third study, individuals within the top 25% of OHL scores had fewer bleeding sites, less dental plaque and had lost fewer teeth than individuals in the lowest 25%, after adjusting for other factors.11Holtzman JS, Atchison KA, Macek MD, Markovic D. Oral health literacy and measures of periodontal disease. J Periodontol 2017;88(1):78-88. An association was found for low OHL and infrequent dental visits, increased DMFT, self-reported poor oral health and reduced dental knowledge.11Holtzman JS, Atchison KA, Macek MD, Markovic D. Oral health literacy and measures of periodontal disease. J Periodontol 2017;88(1):78-88.,12Baskaradoss JK. The association between oral health literacy and missed dental appointments. J Am Dent Assoc 2016;147(11):867-74. Further, in another study 77% and 44% of individuals with high and below-basic health literacy, respectively, had a dental visit in the prior year.13White S, Chen J, Atchison R. Relationship of preventive health practices and health literacy: a national study. Am J Health Behav 2008;32(3):227-42. Childhood dental anxiety, which impacts oral health and related quality of life, has been found to be associated with poor parental OHL.14Armfield JM, Stewart JF, Spencer AJ. The vicious cycle of dental fear: exploring the interplay between oral health, service utilization and dental fear. BMC Oral Health 2007;7:1.,15Shin WK, Braun TM, Inglehart MR. Parents’ dental anxiety and oral health literacy: effects on parents’ and children’s oral health-related experiences. J Public Health Dent 2014;74(3):195-201.
Figure 1. Prevalence and severity of periodontitis in individuals with low and higher levels of OHL
Findings in other countries using local-language assessment tools also include associations for OHL and oral health, after adjusting for other factors.16Blizniuk A, Ueno M, Zaitsu T, Kawaguchi Y. Association of oral health literacy with oral health behaviour and oral health status in Belarus. Community Dent Health 2015;32(3):148-52.,17Ueno M, Takeuchi S, Oshiro A, Kawaguchi Y. Relationship between oral health literacy and oral health behaviors and clinical status in Japanese adults. J Dent Sci 2013;8:170-6.,18Batista MJ, Lawrence HP, Sousa MDLR. Oral health literacy and oral health outcomes in an adult population in Brazil. BMC Public Health 2017;18(1):60.,19Sistani MMN, Virtanen J, Yazdani R, Murtomaa H. Association of oral health behavior and the use of dental services with oral health literacy among adults in Tehran, Iran. Eur J Dent 2017;11(2):162-7.,20Dickson-Swift V, Kenny A, Farmer J, Gussy M, Larkins S. Measuring oral health literacy: a scoping review of existing tools. BMC Oral Health 2014;14:148. Available at: http://www.biomedcentral.com/1472-6831/14/148 In a study in Russia, fewer missing teeth and more restored teeth were found in individuals with adequate OHL.16Blizniuk A, Ueno M, Zaitsu T, Kawaguchi Y. Association of oral health literacy with oral health behaviour and oral health status in Belarus. Community Dent Health 2015;32(3):148-52. In a Japanese study, lower OHL was associated with more missing teeth and dental caries, poorer oral health behaviors and a greater risk of periodontal disease.17Ueno M, Takeuchi S, Oshiro A, Kawaguchi Y. Relationship between oral health literacy and oral health behaviors and clinical status in Japanese adults. J Dent Sci 2013;8:170-6. In a Brazilian study, low OHL was a risk factor for dental biofilm accumulation, emergency dental care only, and reduced quality of life (OR = 1.83, 2.24 and 2.06, respectively).18Batista MJ, Lawrence HP, Sousa MDLR. Oral health literacy and oral health outcomes in an adult population in Brazil. BMC Public Health 2017;18(1):60. (Figure 2) In addition, in a study in Iran with more than 1,000 subjects, high OHL scores were significantly correlated with at least daily tooth brushing, less consumption of sugary snacks/beverages, and dental visits within the prior 6 months.19Sistani MMN, Virtanen J, Yazdani R, Murtomaa H. Association of oral health behavior and the use of dental services with oral health literacy among adults in Tehran, Iran. Eur J Dent 2017;11(2):162-7.
Measuring oral health literacy
A scoping review of studies conducted between 2007 and 2013 identified 32 studies with OHL measuring tools.20Dickson-Swift V, Kenny A, Farmer J, Gussy M, Larkins S. Measuring oral health literacy: a scoping review of existing tools. BMC Oral Health 2014;14:148. Available at: http://www.biomedcentral.com/1472-6831/14/148 The REALD-30 uses 30 dental terminology words in a word recognition test; it does not measure comprehensive OHL. Scores range from 0 to 30 (lowest to highest OHL).20Dickson-Swift V, Kenny A, Farmer J, Gussy M, Larkins S. Measuring oral health literacy: a scoping review of existing tools. BMC Oral Health 2014;14:148. Available at: http://www.biomedcentral.com/1472-6831/14/148,21Horn JM, Lee JY, Divaris K, Baker AD, Vann WF. Oral health literacy and knowledge among patients who are pregnant for the first time. J Am Dent Assoc 2012;143(9):972-80. Similar tools include the REALD-99, REALM-D and REALMD-20. The Test of Functional Health Literacy in Dentistry (TOFHLiD) uses 68 and 12 items, respectively, to measure literacy and numeracy. This tool has low reliability when used alone. Other measurement tools include the Oral Health Literacy Instrument (OHLI) which measures reading comprehension and numeracy, with the addition of an oral health knowledge test, and is validated and reliable.20Dickson-Swift V, Kenny A, Farmer J, Gussy M, Larkins S. Measuring oral health literacy: a scoping review of existing tools. BMC Oral Health 2014;14:148. Available at: http://www.biomedcentral.com/1472-6831/14/148,22Sabbahi DA, Lawrence HP, Limeback H, Rootman I. Development and evaluation of an oral health literacy instrument for adults. Community Dent Oral Epidemiol 2009;37(5):451-62. The Comprehensive Measure of Oral Health Knowledge (CMOHK) measures word recognition and oral health knowledge, and the Oral Health Literacy Inventory for Parents (OH-LIP) is used for pediatric patients. The Oral Health Literacy Adults Questionnaire (OHL-AQ) measures reading comprehension, listening, numeracy and decision-making. It has been validated and found to be reliable. An Oral Health Literacy Assessment in Spanish (OHLA-S) and English (OHLA-E) have been developed and validated.23Lee J, Stucky B, Rozier G, Lee SY, Zeldin LP. Oral health literacy assessment: development of an oral health literacy instrument for Spanish speakers. J Public Health Dent 2013;73(1):1-8.,24Bado FMR, Rebustini F, Jamieson L, Cortellazzi KL, Mialhe FL. Evaluation of the psychometric properties of the Brazilian version of the Oral Health Literacy Assessment in Spanish and development of a shortened form of the instrument. PLoS One 2018;13(11):e0207989. doi: 10.1371/journal.pone.0207989. These contain word recognition and comprehension sections, and are not interchangeable. Translations and adaptations of English-language OHL measurement tools have been evaluated and validated for use in other languages and cultures.19Sistani MMN, Virtanen J, Yazdani R, Murtomaa H. Association of oral health behavior and the use of dental services with oral health literacy among adults in Tehran, Iran. Eur J Dent 2017;11(2):162-7.,20Dickson-Swift V, Kenny A, Farmer J, Gussy M, Larkins S. Measuring oral health literacy: a scoping review of existing tools. BMC Oral Health 2014;14:148. Available at: http://www.biomedcentral.com/1472-6831/14/148,25Cartes-Velásquez RA, Luengo Machuca L. Adaptation and validation of the oral health literacy instrument for the Chilean population. Int Dent J 2017;67(4):215-20. (Table 1)
Table 1. Domains measured in OHL assessment tools
| Word recognition | Comprehension | Numeracy | Oral health knowledge | Decision making | |
|---|---|---|---|---|---|
| REALD-30 | Yes | No | No | No | No |
| TOFHLiD | Yes | No | Yes | No | No |
| OHLI | Yes | Yes | Yes | Yes | No |
| CMOHK | Yes | No | No | Yes | No |
| OHL-AQ | Yes | Yes | Yes | No | Yes |
| OHLA-E, OHLA-S | Yes | Yes | No | No | No |
Factors affecting OHL
Given that OHL requires basic literacy, cognition, social skills and knowledge,11Holtzman JS, Atchison KA, Macek MD, Markovic D. Oral health literacy and measures of periodontal disease. J Periodontol 2017;88(1):78-88.,20Dickson-Swift V, Kenny A, Farmer J, Gussy M, Larkins S. Measuring oral health literacy: a scoping review of existing tools. BMC Oral Health 2014;14:148. Available at: http://www.biomedcentral.com/1472-6831/14/148 these skills are factors in individual’s level of OHL. (Table 2) In a recent national assessment in the United States, an estimated 43% of adults had below-basic or basic abilities to locate or read and understand short prose.26National Center for Education Statistics. National Assessment of Adult Literacy, 2003. Available at: https://nces.ed.gov/naal/kf_demographics.asp. In addition, 34% of individuals had below-basic/basic skills in locating and following instructions in simple documents, or reading and understanding information in simple documents, and 55% had below-basic or basic quantitative skills. Healthcare information that is expressed above these levels will therefore not be understood by a significant proportion of the adult population.
| Table 2. Factors affecting OHL |
|---|
| Basic literacy |
| Low levels of education |
| Low socio-economic status |
| Cognition |
| Social skills |
| Language |
| Knowledge |
| Culture and ethnicity |
| Aging |
| Healthcare system |
Poor OHL is associated with low levels of education and socio-economic status.4Baskaradoss JK. Relationship between oral health literacy and oral health status. BMC Oral Health 2018;18:172. Available at: https://doi.org/10.1186/s12903-018-0640-1.,21Horn JM, Lee JY, Divaris K, Baker AD, Vann WF. Oral health literacy and knowledge among patients who are pregnant for the first time. J Am Dent Assoc 2012;143(9):972-80.,27Butler M. Oral health literacy: How can we impact vulnerable populations. In: Roundtable on health literacy; Board on Population Health and Public Health Practice; Institute of Medicine. Washington (DC): National Academies Press (US); 2013 Feb 19. Available at: https://www.ncbi.nlm.nih.gov/books/NBK207117/. Further, language, culture, aging (cognitive decline) and healthcare system characteristics play a role.4Baskaradoss JK. Relationship between oral health literacy and oral health status. BMC Oral Health 2018;18:172. Available at: https://doi.org/10.1186/s12903-018-0640-1.,28Horowitz AM, Kleinman DV. Oral health literacy: The new imperative to better oral health. Dent Clin North Am 2008;52(2):333-44. (Table 2) Among individuals with below-basic prose literacy in 2003, 55% did not graduate from high school, 44% did not speak English until attending school, 39% and 20% respectively were Hispanic and African-American adults, and 26% were 65 years-of-age and older.26National Center for Education Statistics. National Assessment of Adult Literacy, 2003. Available at: https://nces.ed.gov/naal/kf_demographics.asp. (Figure 3) However, while individuals with higher levels of education are more likely to have adequate OHL, high levels of education do not guarantee high OHL.16Blizniuk A, Ueno M, Zaitsu T, Kawaguchi Y. Association of oral health literacy with oral health behaviour and oral health status in Belarus. Community Dent Health 2015;32(3):148-52. In one study with well-educated individuals, 33%, 31% and 37% of participants, respectively, had low, moderate and high OHL.10Wehmeyer MM, Corwin CL, Guthmiller JM, Lee JY. The impact of oral health literacy on periodontal health status. J Public Health Dent 2014;74(1):80-7. According to the Department of Health and Human Services, approximately 10% of adults are proficient at using everyday health information.29U.S. Department of Health and Human Services. National Action Plan to Improve Health Literacy. Available at: https://health.gov/communication/hlactionplan/pdf/Health_Literacy_Action_Plan.pdf.
Improving OHL
Strategies to improve OHL include tailoring communication to patients’ OHL, and making the system and dental setting more understandable and navigable.2American Dental Association. Health Literacy in Dentistry. Available at: https://www.ada.org/en/public-programs/health-literacy-in-dentistry. Communication techniques and teach-back are considered basic techniques.30“5 Oral Health Literacy Programs.” Institute of Medicine. 2013. Oral Health Literacy: Workshop Summary. Washington, DC: The National Academies Press. doi: 10.17226/13484.) Plain language includes but is not limited to providing key information first, breaking down complex information, and using simple language.31U.S. Department of Health and Human Services. Quick guide to health literacy. Fact Sheet. Available at: https://health.gov/communication/literacy/quickguide/factsbasic.htm#seven. (Figure 4) Using plain language and confirming that patients understood what you have communicated through teach-back, whereby patients are asked to repeat information received, fosters understanding.30“5 Oral Health Literacy Programs.” Institute of Medicine. 2013. Oral Health Literacy: Workshop Summary. Washington, DC: The National Academies Press. doi: 10.17226/13484.),31U.S. Department of Health and Human Services. Quick guide to health literacy. Fact Sheet. Available at: https://health.gov/communication/literacy/quickguide/factsbasic.htm#seven.,32Buerlein JK, Horowitz AM, Child WL. Perspectives of Maryland women regarding oral health during pregnancy and early childhood. J Public Health Dent 2011;71(2):131-5. Other methods fall under the categories of patient-friendly, assistance, and use of materials (such as visual diagrams, models, videos or DVDs).30“5 Oral Health Literacy Programs.” Institute of Medicine. 2013. Oral Health Literacy: Workshop Summary. Washington, DC: The National Academies Press. doi: 10.17226/13484.) Consideration should be given to a patient’s preferred method(s) of learning. Using written information if a patient prefers visual or verbal information creates a barrier.33Centers for Disease Control and Prevention. Health literacy for public health professionals. Available at: https://www.cdc.gov/healthliteracy/training/page1613.html. In a systematic review investigating techniques used for patients with low health literacy, the use of visual and verbal tools including adding icons to improve patients’ understanding of numerical data, showing videos, and presenting key information first/alone improved understanding.34Sheridan SL, Halpern DJ, Viera AJ, Berkman ND, Donahue KE, Crotty K. Interventions for individuals with low health literacy: a systematic review. J Health Commun 2011;16(Suppl 3):30-54.
In addition, programs and communication should be culturally sensitive.35U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion. Quick guide to health literacy. Fact sheet. Available at: https://health.gov/communication/literacy/quickguide/factsbasic.htm#seven. In a review of studies with indigenous populations, improvements in OHL to reduce health disparities were associated with culturally-adapted strategies and included involvement by members of the community in delivering programs and research.36Tiwari T, Jamieson L, Broughton J, Lawrence HP, Batliner TS, Arantes R, Albino J. Reducing indigenous oral health inequalities: A review from 5 nations. J Dent Res 2018;97(8):869-77. Collaborative programs involving public health, institutions, schools and companies, such as ‘Bright Smiles, Bright Futures’, also play a role in improving OHL, dental knowledge and oral health in children and adults.27Butler M. Oral health literacy: How can we impact vulnerable populations. In: Roundtable on health literacy; Board on Population Health and Public Health Practice; Institute of Medicine. Washington (DC): National Academies Press (US); 2013 Feb 19. Available at: https://www.ncbi.nlm.nih.gov/books/NBK207117/.
Figure 4. Plain language information for parents27Butler M. Oral health literacy: How can we impact vulnerable populations. In: Roundtable on health literacy; Board on Population Health and Public Health Practice; Institute of Medicine. Washington (DC): National Academies Press (US); 2013 Feb 19. Available at: https://www.ncbi.nlm.nih.gov/books/NBK207117/.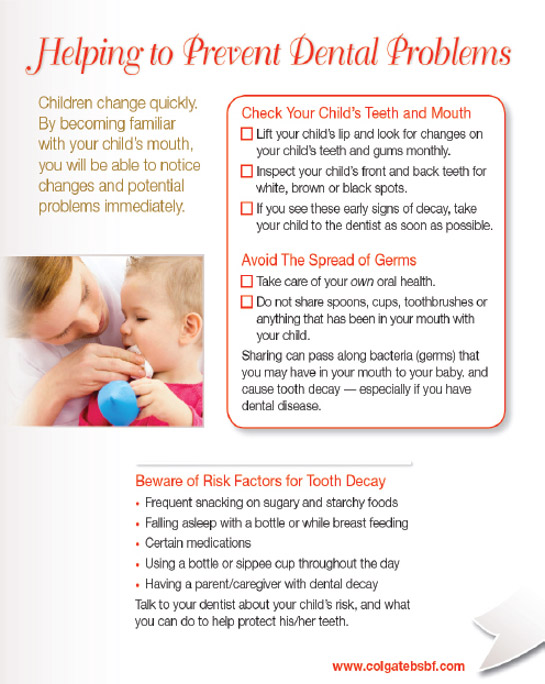
Implications for Dental Professionals
Dental professionals can assess their office for patient-friendliness, cultural competency, ability to effectively communicate and use of plain language. Based on a recent assessment, using an OHL assessment tool increases the number of communication techniques used for low-OHL patients.37Flynn P, Acharya A, Schwei K, VanWormer J, Skrzypcak K. Assessing dental hygienists’ communication techniques for use with low oral health literacy patients. J Dent Hyg 2016;90(3):162-9. Identifying the level of OHL enables the implementation of strategies that foster improvements in OHL with the goal of improving oral health and outcomes.18Batista MJ, Lawrence HP, Sousa MDLR. Oral health literacy and oral health outcomes in an adult population in Brazil. BMC Public Health 2017;18(1):60.,20Dickson-Swift V, Kenny A, Farmer J, Gussy M, Larkins S. Measuring oral health literacy: a scoping review of existing tools. BMC Oral Health 2014;14:148. Available at: http://www.biomedcentral.com/1472-6831/14/148,37Flynn P, Acharya A, Schwei K, VanWormer J, Skrzypcak K. Assessing dental hygienists’ communication techniques for use with low oral health literacy patients. J Dent Hyg 2016;90(3):162-9. Integrated electronic health records and motivational interviewing have also been found to be helpful with low-OHL patients.37Flynn P, Acharya A, Schwei K, VanWormer J, Skrzypcak K. Assessing dental hygienists’ communication techniques for use with low oral health literacy patients. J Dent Hyg 2016;90(3):162-9. Further, the adoption of digital technology has presented an opportunity for patient-friendly communication. Examples include the use of intraoral images, scans, visually-oriented risk assessment tools and on-line videos. Public health and community programs have been adopted that help children and adults improve their OHL and oral health.
Conclusions
Studies have shown that OHL impacts oral health, oral health behaviors and individuals’ understanding of health information and instructions. While associations for oral health and OHL were not found in other studies, this may be due to differences in assessment tools and their effect on the information collected, lack of interchangeability, varying validity and reliability, and study heterogeneity.7Firmino RT, Ferreira FM, Paiva SM, Granville-Garcia AF, Fraiz FC, Martins CC. Oral health literacy and associated oral conditions: A systematic review. J Am Dent Assoc 2017;148(8):604-13.,20Dickson-Swift V, Kenny A, Farmer J, Gussy M, Larkins S. Measuring oral health literacy: a scoping review of existing tools. BMC Oral Health 2014;14:148. Available at: http://www.biomedcentral.com/1472-6831/14/148,38Aldoory L, Macek MD, Atchison KA, Chen H. Comparing well-tested health literacy measures for oral health: A pilot assessment. Health Commun 2016;21(11):1161-9. Robust prospective studies have been recommended to confirm the evidence on OHL.9Firmino RT, Martins CC, Faria LDS, Martins Paiva S, Granville-Garcia AF, Fraiz FC, Ferreira FM. Association of oral health literacy with oral health behaviors, perception, knowledge, and dental treatment related outcomes: a systematic review and meta-analysis. J Public Health Dent 2018 Mar 2. doi: 10.1111/jphd.12266. Further work has also been recommended to refine assessment tools.20Dickson-Swift V, Kenny A, Farmer J, Gussy M, Larkins S. Measuring oral health literacy: a scoping review of existing tools. BMC Oral Health 2014;14:148. Available at: http://www.biomedcentral.com/1472-6831/14/148 Improving OHL can empower patients to improve their oral health and navigate the healthcare system. In addition, more training in communication and OHL knowledge is recommended for dental professionals, including in professional educational settings.37Flynn P, Acharya A, Schwei K, VanWormer J, Skrzypcak K. Assessing dental hygienists’ communication techniques for use with low oral health literacy patients. J Dent Hyg 2016;90(3):162-9. Dental professionals are in a unique position to help patients and the community improve OHL. The influence of patient-clinician communication should be considered as a means to improve understanding, attendance, treatment acceptance and outcomes.
References
- 1.Dominy SS, et al. Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Sci Adv. 2019;5(1):eaau3333 https://www.ncbi.nlm.nih.gov/pubmed/30746447.
- 2.Sadrameli M, et al. Linking mechanisms of periodontitis to Alzheimer’s disease. Curr Opin Neurol. 2020;33(2):230-8 https://www.ncbi.nlm.nih.gov/pubmed/32097126.
- 3.Borsa L, et al. Analysis the link between periodontal diseases and Alzheimer’s disease: A systematic review. Int J Environ Res Public Health. 2021;18(17) https://www.ncbi.nlm.nih.gov/pubmed/34501899.
- 4.Costa MJF, et al. Relationship of Porphyromonas gingivalis and Alzheimer’s disease: A systematic review of pre-clinical studies. Clin Oral Investig. 2021;25(3):797-806 https://www.ncbi.nlm.nih.gov/pubmed/33469718.
- 5.Munoz Fernandez SS, Lima Ribeiro SM. Nutrition and Alzheimer disease. Clin Geriatr Med. 2018;34(4):677-97 https://www.ncbi.nlm.nih.gov/pubmed/30336995.
- 6.Aquilani R, et al. Is the Brain Undernourished in Alzheimer’s Disease? Nutrients. 2022;14(9) https://www.ncbi.nlm.nih.gov/pubmed/35565839.
- 7.Fukushima-Nakayama Y, et al. Reduced mastication impairs memory function. J Dent Res. 2017;96(9):1058-66 https://www.ncbi.nlm.nih.gov/pubmed/28621563.
- 8.Kim HB, et al. Abeta accumulation in vmo contributes to masticatory dysfunction in 5XFAD Mice. J Dent Res. 2021;100(9):960-7 https://www.ncbi.nlm.nih.gov/pubmed/33719684.
- 9.Miura H, et al. Relationship between cognitive function and mastication in elderly females. J Oral Rehabil. 2003;30(8):808-11 https://www.ncbi.nlm.nih.gov/pubmed/12880404.
- 10.Lexomboon D, et al. Chewing ability and tooth loss: association with cognitive impairment in an elderly population study. J Am Geriatr Soc. 2012;60(10):1951-6 https://www.ncbi.nlm.nih.gov/pubmed/23035667.
- 11.Elsig F, et al. Tooth loss, chewing efficiency and cognitive impairment in geriatric patients. Gerodontology. 2015;32(2):149-56 https://www.ncbi.nlm.nih.gov/pubmed/24128078.
- 12.Kim EK, et al. Relationship between chewing ability and cognitive impairment in the rural elderly. Arch Gerontol Geriatr. 2017;70:209-13 https://www.ncbi.nlm.nih.gov/pubmed/28214402.
- 13.Kim MS, et al. The association between mastication and mild cognitive impairment in Korean adults. Medicine (Baltimore). 2020;99(23):e20653 https://www.ncbi.nlm.nih.gov/pubmed/32502052.
- 14.Cardoso MG, et al. Relationship between functional masticatory units and cognitive impairment in elderly persons. J Oral Rehabil. 2019;46(5):417-23 https://www.ncbi.nlm.nih.gov/pubmed/30614023.
- 15.Popovac A, et al. Oral health status and nutritional habits as predictors for developing alzheimer’s disease. Med Princ Pract. 2021;30(5):448-54 https://www.ncbi.nlm.nih.gov/pubmed/34348313.
- 16.Park T, et al. More teeth and posterior balanced occlusion are a key determinant for cognitive function in the elderly. Int J Environ Res Public Health. 2021;18(4) https://www.ncbi.nlm.nih.gov/pubmed/33669490.
- 17.Lin CS, et al. Association between tooth loss and gray matter volume in cognitive impairment. Brain Imaging Behav. 2020;14(2):396-407 https://www.ncbi.nlm.nih.gov/pubmed/32170642.
- 18.Kumar S, et al. Oral health status and treatment need in geriatric patients with different degrees of cognitive impairment and dementia: a cross-sectional study. J Family Med Prim Care. 2021;10(6):2171-6 https://www.ncbi.nlm.nih.gov/pubmed/34322409.
- 19.Delwel S, et al. Chewing efficiency, global cognitive functioning, and dentition: A cross-sectional observational study in older people with mild cognitive impairment or mild to moderate dementia. Front Aging Neurosci. 2020;12:225 https://www.ncbi.nlm.nih.gov/pubmed/33033478.
- 20.Da Silva JD, et al. Association between cognitive health and masticatory conditions: a descriptive study of the national database of the universal healthcare system in Japan. Aging (Albany NY). 2021;13(6):7943-52 https://www.ncbi.nlm.nih.gov/pubmed/33739304.
- 21.Galindo-Moreno P, et al. The impact of tooth loss on cognitive function. Clin Oral Investig. 2022;26(4):3493-500 https://www.ncbi.nlm.nih.gov/pubmed/34881401.
- 22.Stewart R, et al. Adverse oral health and cognitive decline: The health, aging and body composition study. J Am Geriatr Soc. 2013;61(2):177-84 https://www.ncbi.nlm.nih.gov/pubmed/23405916.
- 23.Dintica CS, et al. The relation of poor mastication with cognition and dementia risk: A population-based longitudinal study. Aging (Albany NY). 2020;12(9):8536-48 https://www.ncbi.nlm.nih.gov/pubmed/32353829.
- 24.Kim MS, Han DH. Does reduced chewing ability efficiency influence cognitive function? Results of a 10-year national cohort study. Medicine (Baltimore). 2022;101(25):e29270 https://www.ncbi.nlm.nih.gov/pubmed/35758356.
- 25.Ko KA, et al. The Impact of Masticatory Function on Cognitive Impairment in Older Patients: A Population-Based Matched Case-Control Study. Yonsei Med J. 2022;63(8):783-9 https://www.ncbi.nlm.nih.gov/pubmed/35914761.
- 26.Garre-Olmo J. [Epidemiology of Alzheimer’s disease and other dementias]. Rev Neurol. 2018;66(11):377-86 https://www.ncbi.nlm.nih.gov/pubmed/29790571.
- 27.Stephan BCM, et al. Secular Trends in Dementia Prevalence and Incidence Worldwide: A Systematic Review. J Alzheimers Dis. 2018;66(2):653-80 https://www.ncbi.nlm.nih.gov/pubmed/30347617.
- 28.Lopez OL, Kuller LH. Epidemiology of aging and associated cognitive disorders: Prevalence and incidence of Alzheimer’s disease and other dementias. Handb Clin Neurol. 2019;167:139-48 https://www.ncbi.nlm.nih.gov/pubmed/31753130.
- 29.Ono Y, et al. Occlusion and brain function: mastication as a prevention of cognitive dysfunction. J Oral Rehabil. 2010;37(8):624-40 https://www.ncbi.nlm.nih.gov/pubmed/20236235.
- 30.Kubo KY, et al. Masticatory function and cognitive function. Okajimas Folia Anat Jpn. 2010;87(3):135-40 https://www.ncbi.nlm.nih.gov/pubmed/21174943.
- 31.Chen H, et al. Chewing Maintains Hippocampus-Dependent Cognitive Function. Int J Med Sci. 2015;12(6):502-9 https://www.ncbi.nlm.nih.gov/pubmed/26078711.
- 32.Azuma K, et al. Association between Mastication, the Hippocampus, and the HPA Axis: A Comprehensive Review. Int J Mol Sci. 2017;18(8) https://www.ncbi.nlm.nih.gov/pubmed/28771175.
- 33.Chuhuaicura P, et al. Mastication as a protective factor of the cognitive decline in adults: A qualitative systematic review. Int Dent J. 2019;69(5):334-40 https://www.ncbi.nlm.nih.gov/pubmed/31140598.
- 34.Lopez-Chaichio L, et al. Oral health and healthy chewing for healthy cognitive ageing: A comprehensive narrative review. Gerodontology. 2021;38(2):126-35 https://www.ncbi.nlm.nih.gov/pubmed/33179281.
- 35.Tada A, Miura H. Association between mastication and cognitive status: A systematic review. Arch Gerontol Geriatr. 2017;70:44-53 https://www.ncbi.nlm.nih.gov/pubmed/28042986.
- 36.Ahmed SE, et al. Influence of Dental Prostheses on Cognitive Functioning in Elderly Population: A Systematic Review. J Pharm Bioallied Sci. 2021;13(Suppl 1):S788-S94 https://www.ncbi.nlm.nih.gov/pubmed/34447202.
- 37.Tonsekar PP, et al. Periodontal disease, tooth loss and dementia: Is there a link? A systematic review. Gerodontology. 2017;34(2):151-63 https://www.ncbi.nlm.nih.gov/pubmed/28168759.
- 38.Nangle MR, Manchery N. Can chronic oral inflammation and masticatory dysfunction contribute to cognitive impairment? Curr Opin Psychiatry. 2020;33(2):156-62 https://www.ncbi.nlm.nih.gov/pubmed/31895157.
- 39.Nakamura T, et al. Oral dysfunctions and cognitive impairment/dementia. J Neurosci Res. 2021;99(2):518-28 https://www.ncbi.nlm.nih.gov/pubmed/33164225.
- 40.Weijenberg RAF, et al. Mind your teeth-The relationship between mastication and cognition. Gerodontology. 2019;36(1):2-7 https://www.ncbi.nlm.nih.gov/pubmed/30480331.
- 41.Asher S, et al. Periodontal health, cognitive decline, and dementia: A systematic review and meta-analysis of longitudinal studies. J Am Geriatr Soc. 2022;70(9):2695-709 https://www.ncbi.nlm.nih.gov/pubmed/36073186.
- 42.Lin CS. Revisiting the link between cognitive decline and masticatory dysfunction. BMC Geriatr. 2018;18(1):5 https://www.ncbi.nlm.nih.gov/pubmed/29304748.
- 43.Wu YT, et al. The changing prevalence and incidence of dementia over time – current evidence. Nat Rev Neurol. 2017;13(6):327-39 https://www.ncbi.nlm.nih.gov/pubmed/28497805.
- 44.National Psoriasis Foundation. Soriatane (Acitretin). https://www.psoriasis.org/soriatane-acitretin/.
- 45.National Psoriasis Foundation. Current Biologics on the Market. https://www.psoriasis.org/current-biologics-on-the-market/.
- 46.Dalmády S, Kemény L, Antal M, Gyulai R. Periodontitis: a newly identified comorbidity in psoriasis and psoriatic arthritis. Expert Rev Clin Immunol 2020;16(1):101-8. doi: 10.1080/1744666X.2019.1700113.


:sharpen(level=0):output(format=jpeg)/up/2023/05/Fiona-Collins-thumbnail-1-3.jpg)
:sharpen(level=0):output(format=jpeg)/up/2019/10/Oral-Health-Literacy-2.jpg)