Patient profile
74-year-old Caucasian male who is eager to receive dental work. Patient is 6 ft and 170lbs. He is well dressed and relaxed at the first meeting. He is retired and spends his free time with his grandkids and wife, he also uses his free time on various hobbies. The patient informs that his wife is also a patient at the dental college, and they are both eager to start with their dental work. He has a previous history of restorative dental work and presents with high blood pressure at the initial visit. The Patient considers himself to be in good health.
Chief Complaint: “I am concerned about my missing teeth”
Patient Expectations: To be able to chew properly and have current dental issues taken care of.
Patient history
Medical history
- At the initial visit, the patient indicates that he is currently taking no medication, has a noncontributory medical history, and no known drug allergies.
- Patient has not seen a physician in almost 2 years.
- Family history Includes paternal hypertension and diabetes. Father had coronary bypass surgery at 64.
- Patient presents with high blood pressure at the initial dental visit and at 2 subsequent visits and is referred to a physician to be evaluated and treated.
- Patient visits a physician and is currently on losartan 25mg.
- ASA 2.
- Review of Systems is noncontributory and within normal limits. Patient’s impression of overall health is good.
Social history
- Drinks 1-2 beers in a week.
- Previous history of smoking 8-10 cigarettes a day and quit about 46 years ago.
- Retired and lives with wife only
- Patient has previous history of unsuccessful dental treatment.
Cultural and socioeconomic considerations
- Patient is familiar with dentistry and has visited dentist when needed in the past. He has had multiple dental work done in the past and wants to commit to fixing any dental issues he currently has.
- Both the patient and his wife are committed to getting their dental work completed. Although they have tried to prioritize health care, due to busy work lifestyle and other expenses, dental visits were only on an as needed basis. It is inportant to emphasize importance of regular dental visits.
- Patient is currently uninsured which is the major reason why dental visits have been erratic. Both the patient and his wife are both retired but have savings and a pension that they want to use to complete dental work.
- Initially, the patient visited a private dental clinic but fees were too high for both the patient and his wife to complete all the dental work needed to be done. This is why the patient is here at the dental school where the fees for dental work is cheaper. Based on the fees of the dental school, finances are not an issue for the patient.
- The patient is an older male and has already solidified his techniques for oral hygiene over many years. It is important to know that frequent reinforcement at every appointment is needed for this kind of patient to improve their oral hygiene. Oral hygiene techniques should also be uncomplicated to maximize the patient’s involvement in their oral health.
Dental history
- Sensitivity in UL region and prefers to chew food on the right side. “I can feel my tooth when I tap on it and when I chew”
- Trouble chewing and is concerned about missing posterior teeth.
- Date of the last dental visit was approximately a year ago for extraction of UR tooth after the failure of root canal treatment. The patient is apprehensive about having any more root canals and says, “I will rather have the tooth extracted than have another root canal.”
- History of extractions: wisdom teeth extractions, non – restorable teeth and failed root canal treatments
- Brushes x2 day with soft manual toothbrush and flosses x1 day
- Patient uses Colgate toothpaste and mouthwash
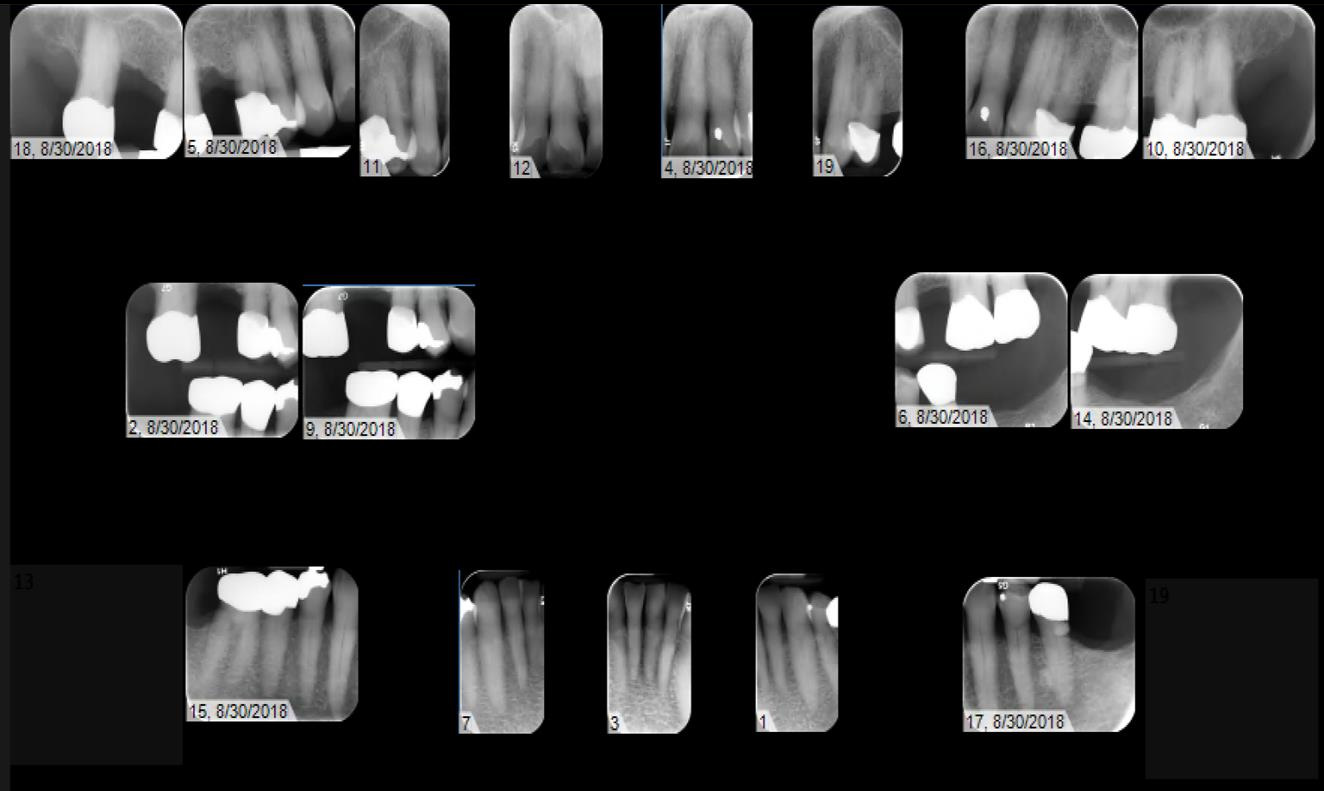
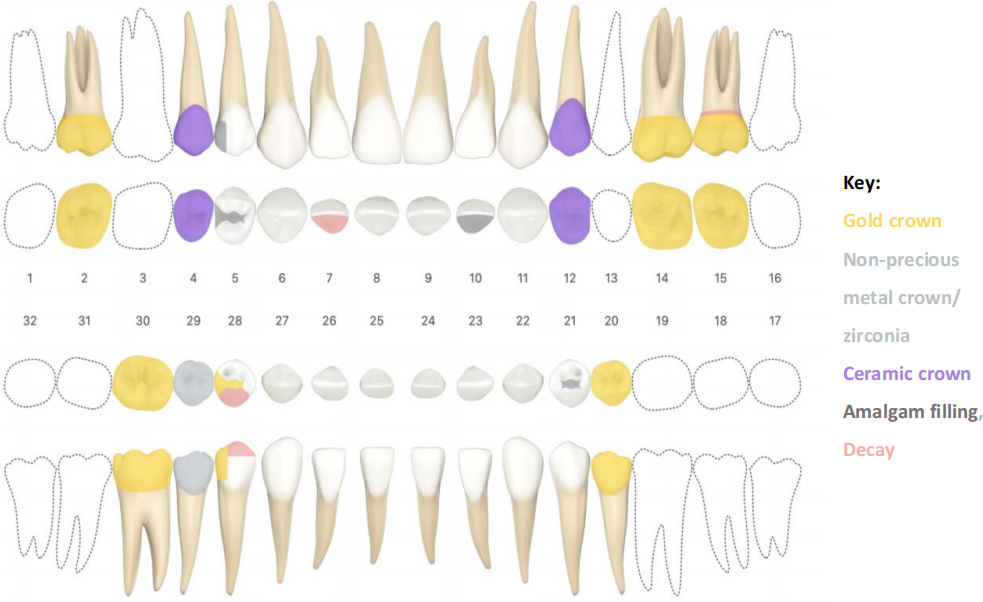
- History of Restorative work
- PFM crowns
- #s 4, 12
- Gold crowns
- #s 2, 14, 15, 20, 30
- Zirconia(?) crown
- #29
- Gold inlay
- #28
- Amalgam fillings
- #5 DO, #10 L, #21 O
- Exts
- Mentioned failed RCT leading to extraction
- PFM crowns
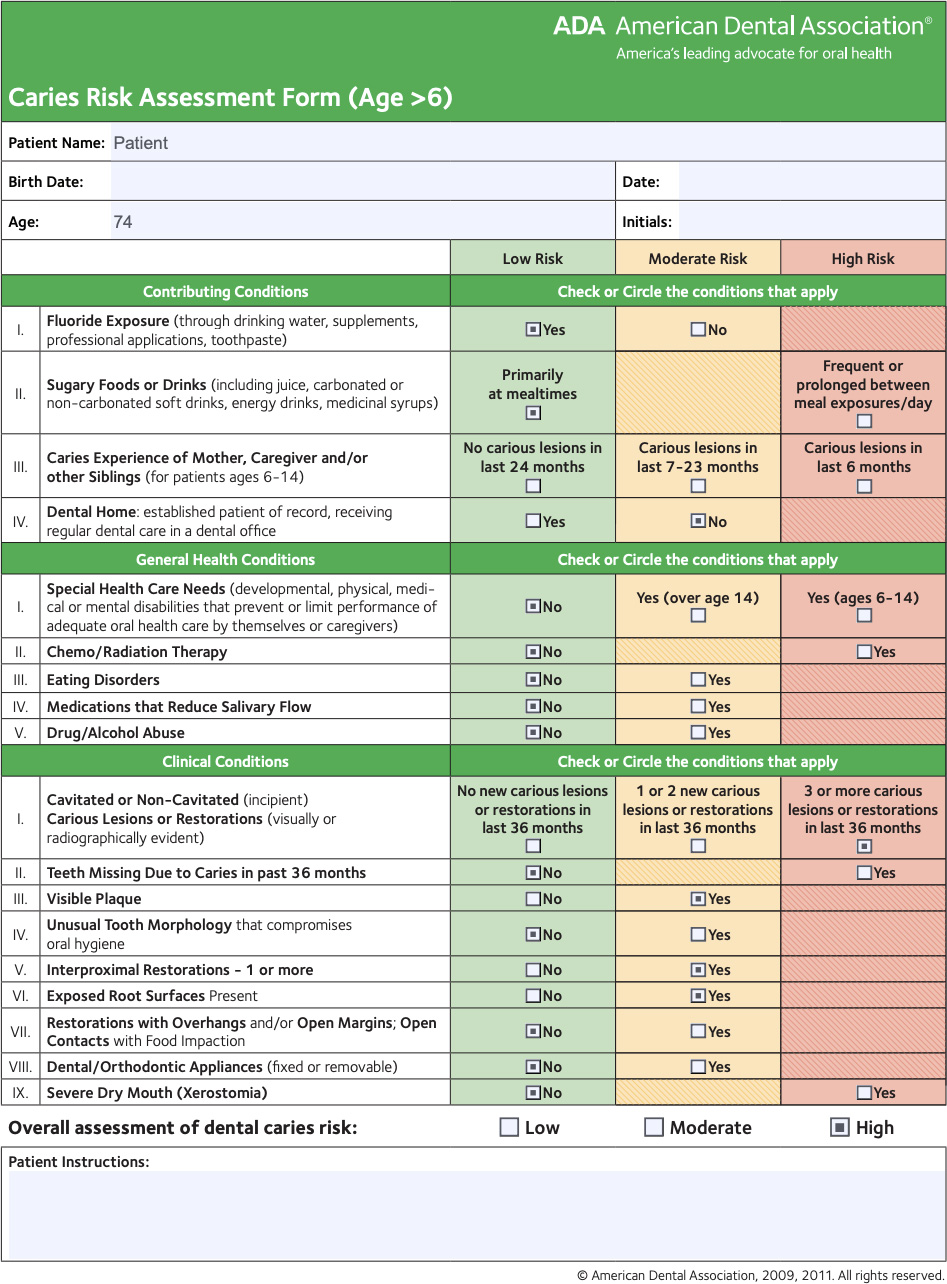
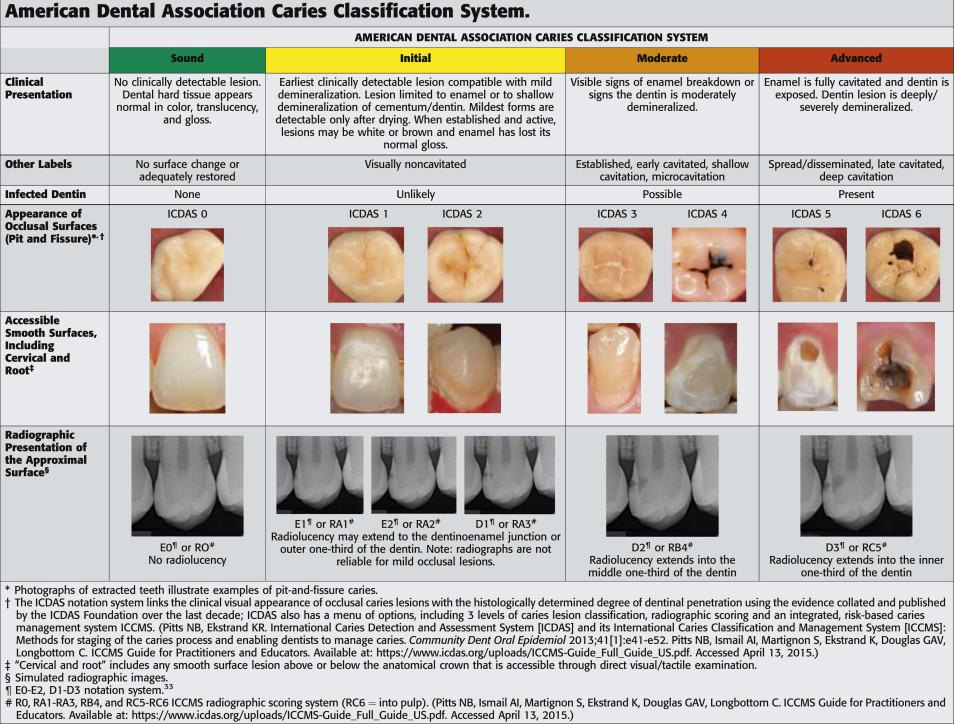
Caries Risk Assessment
Caries Risk:
- Caries Risk: High
- Oral Risk factors
- The patient has had 3 or more new carious lesions in the last 36 months
- Disease Indicators: based on caries – current and past experience (patient has had previous carious lesions, current secondary decay and a new lesion), high decay missing and filled (DMFT) index
- Home care and fluoride exposure
- Generalized moderate plaque
- The patient is motivated to improve oral health and techniques
- Brushes 2x/day and floss 1x/day but his technique is not effective in removing plaque
- Uses toothpaste with fluoride and sometimes drinks fluoridated water
- Diet: Healthy low cariogenic diet but patient consumes cariogenic beverages between meals
- Salivary Factors and Social history: The patient has good salivary flow and at intial appointment is taking no medication. The patient does not have dental home and is apprehensive about some dental treatments.
- Risk Factors
- Exposed roots
- Retentive pits and fissures
- Subgingival restorations
- Abfraction lesions
- Cariogenic beverages – high frequency of cariogenic beverages between meals
- Fair Oral Hygeine – brushes 2x/day and floss 1x/day but the technique is not effective
- No dental home
- Protective Factors
- Fluoride exposure from toothpaste, fluoridated water
- Good salivary flow
Disease Risk Assessment
| Disease Risk | Assessment |
| Caries Risk (based on caries risk assessment and CAMBRA) | High |
| Periodontal disease Risk (based on Probing depth, Bleeding on probing, Tooth loss, Extent of radiographic bone loss, Patient age relative to extent of disease, Diabetes mellitus, Genetic factors (interleukin [IL]-1 genotype status), Cigarette smoking, Tooth factors (furcations, bone loss and calculus) and periodontal disease history. | Low |
| Xerostomia risk (based on medications and patient evaluation) | Low |
| Oral Cancer Risk (based on smoking, alcohol outdoor, HPV, immunocompromised patients, activities, radiation treatment, previous history of oral cancer and present lesions in mouth) | Low |
| Traumatic Occlusion Risk ( based on teeth present, current occlusion, bruxing and clenching, tooth fracture, occlusal related temporomandibular disorders and assessment of PDL) | Moderate |
Clinical Findings:
Extraoral clinical exam
- Leptoprosopic
- Mesocephalic
- Straight profile
- Jaw is symmetrical on opening and closing
- No abnormal findings and no sign of pain or tenderness in the head and neck area
- No clicking or popping in TMJ or tenderness in muscles of mastication
- Submandibular and posterior cervical Lymph nodes were non-palpable
Intraoral clinical exam
- Palate: Normal
- Tongue: slightly coated with normal range of motion and no lesions
- Floor of mouth and mucosa appears normal with no lesions
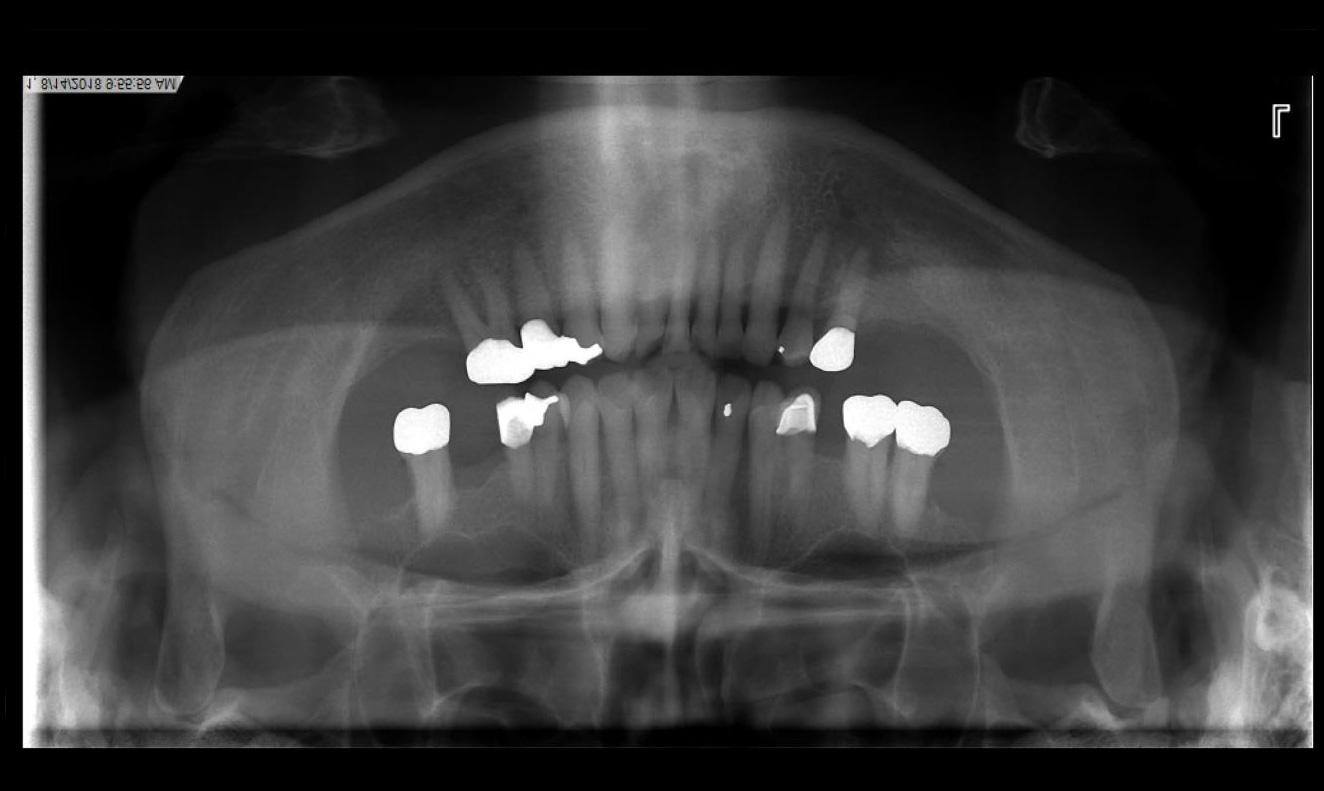
- Teeth with exposed root surfaces from gingival recession
- Discoloration of teeth
- Supraerupted teeth
- Missing teeth – #1,3, 13, 16, 17 18, 19, 31, 32
- Clenching/grinding/ parafunctional habits
- Abfractions
- Wear facets on posterior teeth and restorations
- Craze lines – prominent on #8 and 9
Radiographic evaluation: Full Mouth Series and Panoramic X-ray
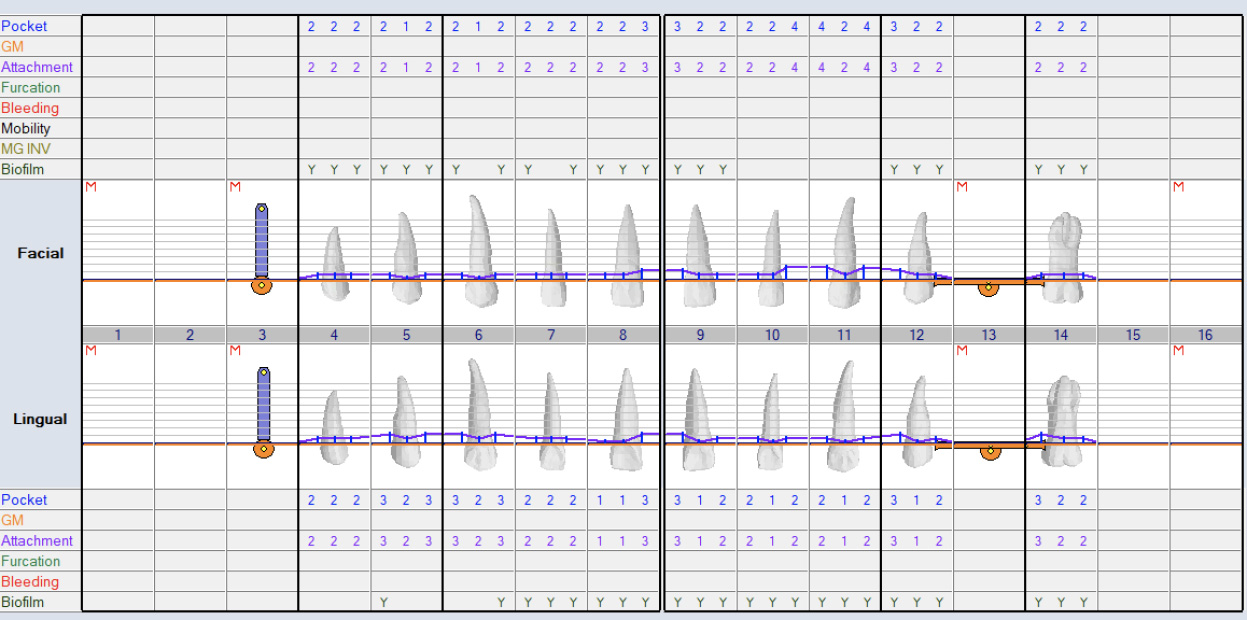
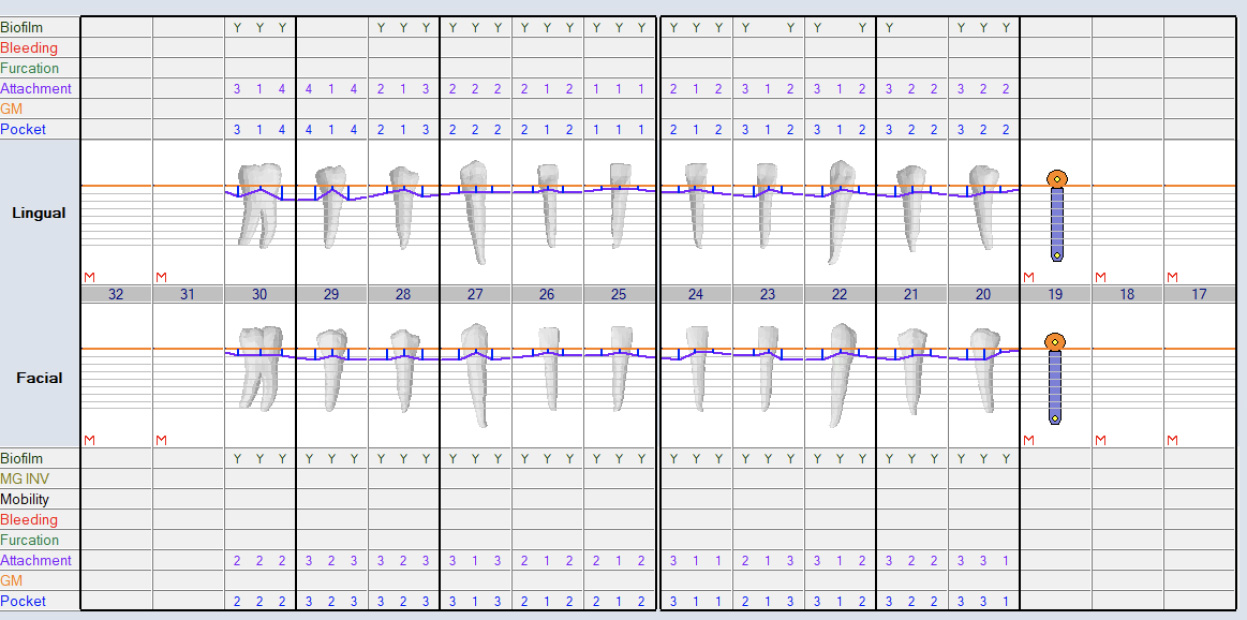
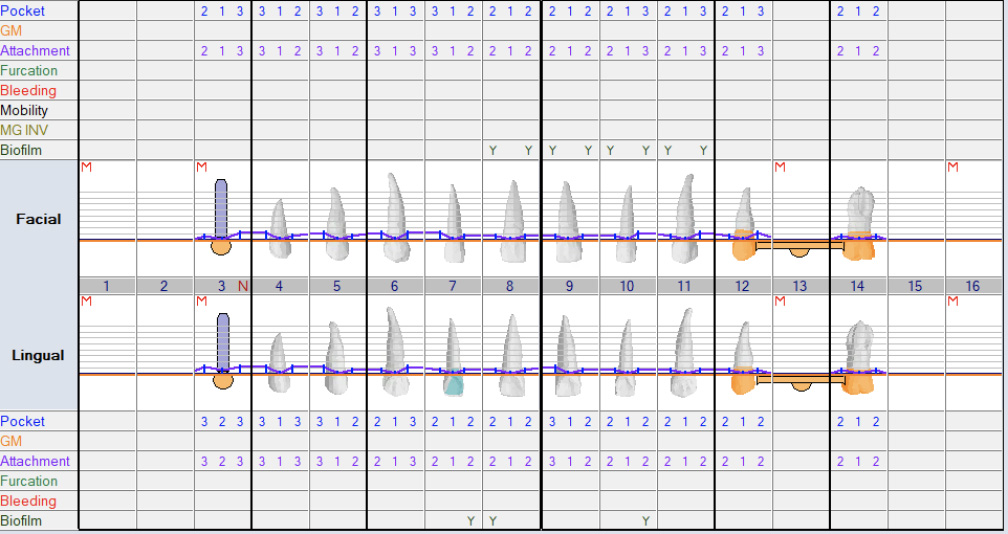
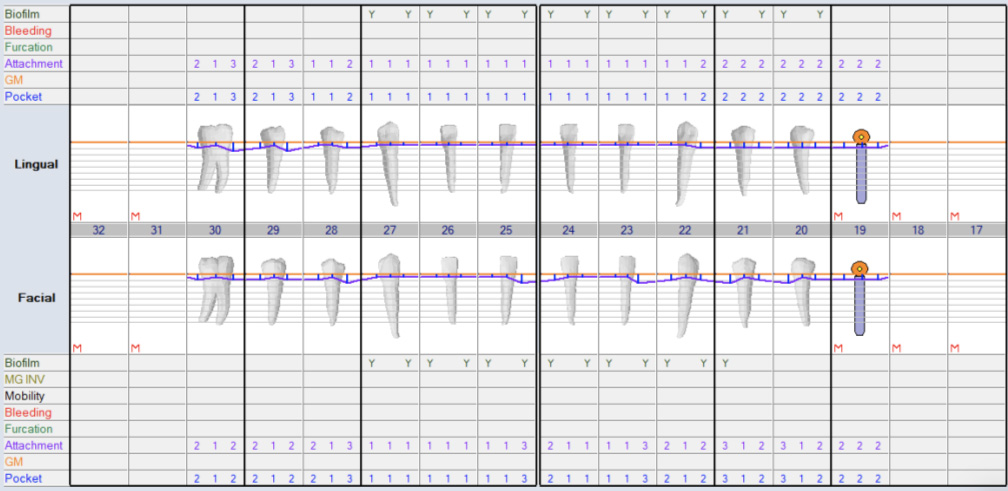
Periodontal Evaluation
- Oral hygiene: fair
- Pock depths within normal range 1-3mm. Few spots with 4mm and no bleeding
- Generalized mild – moderate gingival recession
- No bleeding on probing
- Probing depths measured after extraction of supraerupted #2 and #15
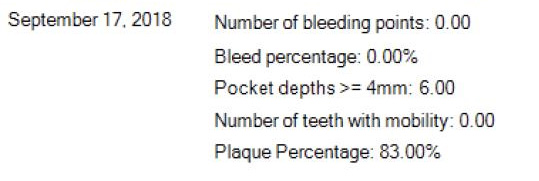
- Bleeding Index: 0.00%
- Plaque Index: 83% (presence of plaque indicated by Y = Yes using plaque disclosing solution)
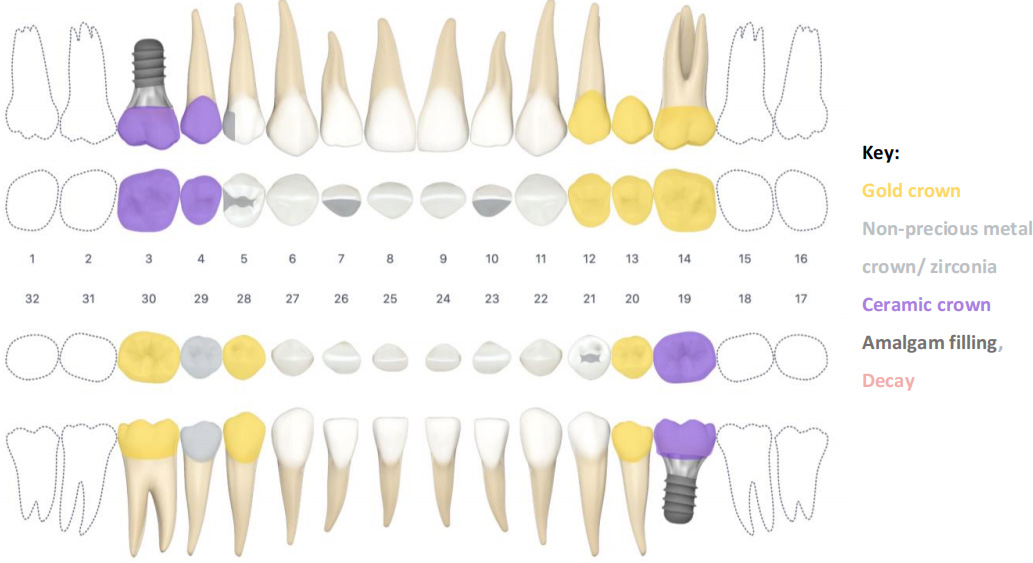
Restorative Chart – Pre- Treatment
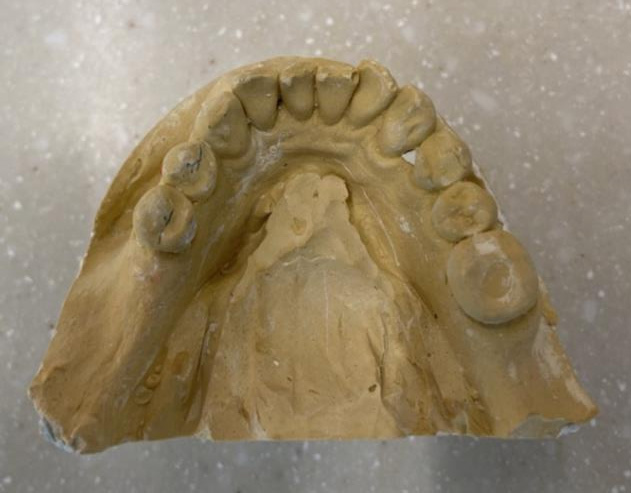
Diagnostic casts
Diagnostic Tools
- Visual examination
- Dental loupes with illumination
- Dental mirror
- Tactile examination with a dental explorer and dental periodontal probe
- X-rays – full mouth series and panormainc x-ray
- Diagnostic Casts, mounted for occlusal analysis
- Plaque disclosing solution
- ADA Caries Risk assessmet form and Caries Risk assessment
- ADA caries classification system ICDAS
Dental exam, Problem list and goals
| Problem list | Treatment Goals | Considerations |
| Preventive | ||
| Moderate generalized plaque, high Plaque score, cariogenic drinks in diet, presence of new lesions, ineffective oral hygiene techniques. |
|
Patient’s current knowledge of oral hygiene and the patient’s willingness to adapt to new and improved techniques. |
| Disease Control and Restorative | ||
| Unopposed upper molars leading to supraeruption (#2 and 15), difficulty chewing | Align teeth with occlusal plane and prevent further supraeruption or extract supraerupted teeth to improve the overall prognosis of oral health and prevent further supraeruption | Patient opts to go with extraction of supraerupted teeth. Patient is willing to pay for implants and is comfortable with the amount of time required to reach treatment goals. Alternative treatment includes intentional endo on supraerupted teeth and enameloplasty. Patient has had multiple failed endo treatments and is unwilling to go that route. |
| Missing teeth #3, 13, 18, 19, 31 | Replace some missing teeth with implants or indirect restorations to improve patients chewing ability | The patient is willing to pay for multiple implants and crowns. |
| Decay #7 L | Restore function and esthetics and prevent further decay | |
| Esthetic issues #8 and 9 | Remove craze lines and staining and restore esthetics | The patient was not concerned with craze lines and staining and will reconsider treatment at a later time |
| Decay #15 B | Restore function and esthetics and prevent further decay | Will be extracted due to supraeruption |
| #28 inlay with secondary decay | Restore function and esthetics and prevent further decay | |
| Generalized recession, exposed roots, wear facets, craze lines and abfractions | Exposed dentin assessed for sensitivity. Option to restore with dental material to prevent sensitivity and further wear of abfractions. In the older population, exposed root surfaces have an increased risk of becoming carious. The goal is to prevent root caries from occurring on exposed cementum. Provide occlusal guard to protect restorations and prevent wear of teeth. | When the patient is assessed for sensitivity, the patient reports that he does not experience sensitivity in exposed regions. The patient is informed of the possibility of sensitivity occurring and risk of caries. Patient is unwilling to address abfractions with restorations and will inform the dentist if the abfractions become sensitive to cold or hot temperatures or when brushing teeth. The patient will be placed on a 3-month fluoride recall regimen to help prevent sensitivity and root caries from occurring. |
Treatment Plan
Goal is to create 1st molar – 1st molar occlusion and stable occlusion
- Disease Control Phase
- ext #s 2, 15
- Prophylaxis, fluoride varnish
- #7 direct amalgam filling
- Restorative Phase
- #s 12×14 indirect bridge restoration
- #28 indirect crown restoration
- Refer for implant #s 3, 19
- Occlusal guard
- Recall and Maintenance Phase
- 3 – 6-month recall
Treatment modifications:
- Med consult re: HTN
Sequenced treatment plan:
- Appointment 1: ext #s 2, 15
- Appointment 2: Prophylaxis, fluoride varnish, Oral hygiene instructions, dietary counselling
- Appointment 3: #7 direct amalgam restoration
- Appointment 4&5: #s 12×14 indirect bridge restoration
- Appointment #6&7: 28 indirect gold crown
- Refer to prosthodontist for implant #s 3, 19
- 3-6-month recalls and maintenance (3 month fluoride and 6 month prophy)
Implementation and Treatment outcomes
Preventive
- Brushing and flossing: Daily removal of plaque is essential to reduce the risk of caries. Patient is made aware to the caries process and the link between plaque, bacteria, sugar and the development of caries. Asked the patient to demonstrate brushing technique at initial appointment. Patient had learned the modified bass brushing technique from his previous dentist and had implemented it in his daily oral hygiene routine. Patient demonstrated technique adequately but admits he does not brush all teeth surfaces sufficiently for up to 2 minutes. Patient also has a good grasp of flossing. Brushing and flossing techniques were reviewed and reinforced to improve and make techniques more effective in removing and disrupting plaque. Techniques will be reinforced at recall appointments. He is reminded to brush for at least 2 minutes and to use the C-shaped circle flossing technique in order to effectively clean gums and teeth. Tongue cleaning is also encouraged to reduce coating of the tongue. Patient is informed of wide range of products that can be incorporated into oral hygiene such as tongue scrapers, floss holders, interproximal brushes, plastic and wooden toothpicks and water flossing instruments. Patient is advised to purchase an electric toothbrush in order to help monitor brushing time and pressure. This will help increase brushing efficacy and reduce the risk of cervical wear. Patient is told to note any bleeding that occurs during oral hygiene as that could be a sign of inflamed gums. Patient now has a bridge and is required to use floss threaders to floss underneath bridge. Patient struggled initially to repeat floss threading techniques demonstrated. He is instructed to go home and practice after bridge is delivered.
Techniques are practiced and reinforced at subsequent appointments and patient is now proficient at using floss threader and has improved oral hygiene. - Dietary counselling: Patient has healthy diet but also has various cariogenic foods and drinks in his diet. Patient is made aware of cariogenic foods containing fermentable carbohydrates that can reduce pH of saliva to less than 5.5. pH of less than 5.5 will lead to demineralization of the teeth surface and this can lead to caries development. Cariostatic foods such as such as cheese, nuts, popcorn or vegetables cannot be broken down by caries causing bacteria. These cariostatic foods are not metabolized by microorganisms in plaque, and so do not cause a drop in salivary pH to less than 5.5. He is advised to minimize the frequency of tooth contact with acids and sugars between meals. It is also advisable to substitute nonacidic high pH foods such as cheeses, nuts for between-meal snacks and limit cariogenic drinks to mealtimes only.
- Water Source: Patient lives in a fluoridated water community but also frequently drinks bottled water. During appointment, he is informed that community water supply plays a role in the prevention of caries. It has been shown that patients that reside in a community with water fluoridation have experienced reduced incidents of root caries and tooth loss compared to those who have lived in communities with non-fluoridated water supplies. Patient is advised to increase tap water consumption or ensure bottled water has an appropriate amount of fluoride. To help prevent tooth decay, water should contain 0.7 to 1ppm of fluoride, 1ppm = 1mg/L.
- Adjuvant Therapies: Patient is advised to chew sugar free xylitol gum or lozenges after meals to increase saliva flow and to aid in reducing caries. Xylitol is anticariogenic and helps to reduce the activity of caries causing bacteria as the bacteria cannot break down xylitol and produce acid. Patient is told from 6-15g of Xylitol gum should be chewed 10-20 minutes after meals 3-5x/day as an adjuvant therapy. Patient has introduced waterpik flosser into regimen and uses it after every meal to ensure mouth is clean.
- Fluoride: Daily use of a prescription dentifrice with fluoride concentrations of 5000 ppm is recommended for the patient with high caries risk and risk of root caries. Patient is provided with prescription. Patient is placed on 3 months recall high exposure fluoride regimen at the dental office. Fluoride 2.26% (NaF) topical varnish every 3 months or 1.23% fluoride (APF) for four minutes every 3 months is used. This is administered at 6 months recall after prophy and in between prophy recalls.
- Recall and Maintenance: Patient is to return to recall clinic every 6 months for a cleaning, fluoride varnish application and maintenance of restorations and implants. Patient is placed on 3 month fluoride recall. At the recall appointment, it is expected that posterior bitewings will be taken every 6 to 12 months.
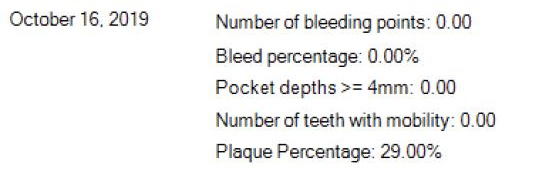
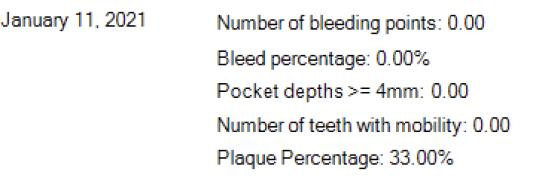
- Overall Outcome: Patients plaque score has improved over subsequent hygiene appointments. Periodontium is currently stable and healthy. Restorations are intact. No new carious lesions have developed, and patient’s overall oral hygiene technique and understanding has improved. All techniques implemented at recall appointments are repeatable and effective. Patient has limited consumption of cariogenic beverages in between meals.
Fig: Final Appointment Perio Chart
Yearly Plaque percentages: Shows improvement in Oral hygiene from initial appointment in 2018
Disease Control and Definitive Treatment
- No new lesions found at update oral diagnosis appointments. Previous restorations and current restorations are intact, and margins are sound. Goal of eliminating disease and maintaining disease free oral environment was met.
- Goals of restoring function and stable occlusion are met. Missing teeth restored and patient is satisfied and impressed with improved chewing capability and absence of sensitivity.
- Patient’s needs were met, and patient left satisfied about overall dental treatment.
- Patient currently has no esthetic concerns and is unwilling to address staining of teeth or craze lines on anterior teeth. Patient’s goal is to restore functionality and not esthetics.
- Occlusal guard provided for patient to wear at night to help protect restorations and teeth from wear and parafunctional forces.
Restorative chart: Post Treatment
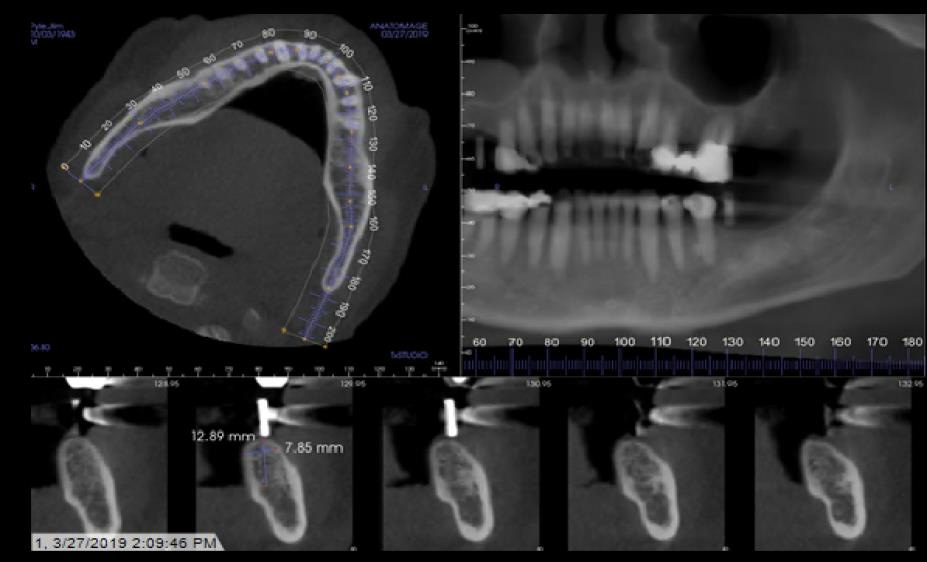
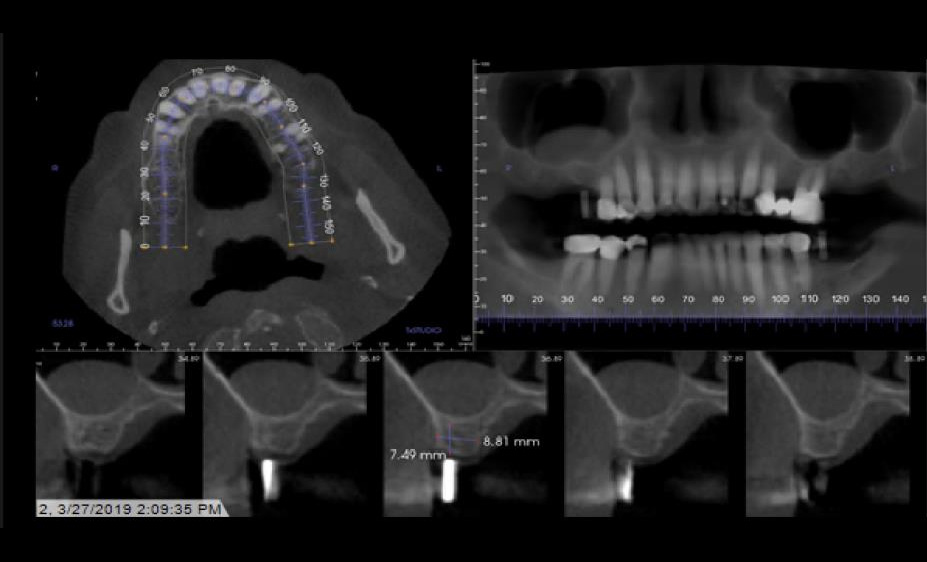
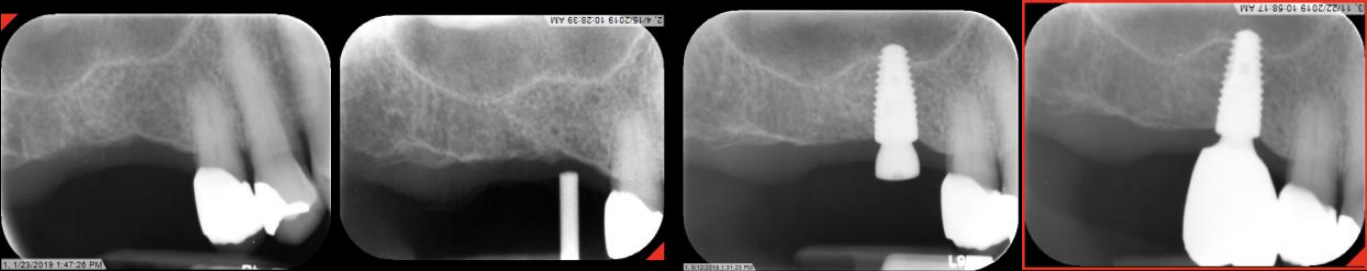
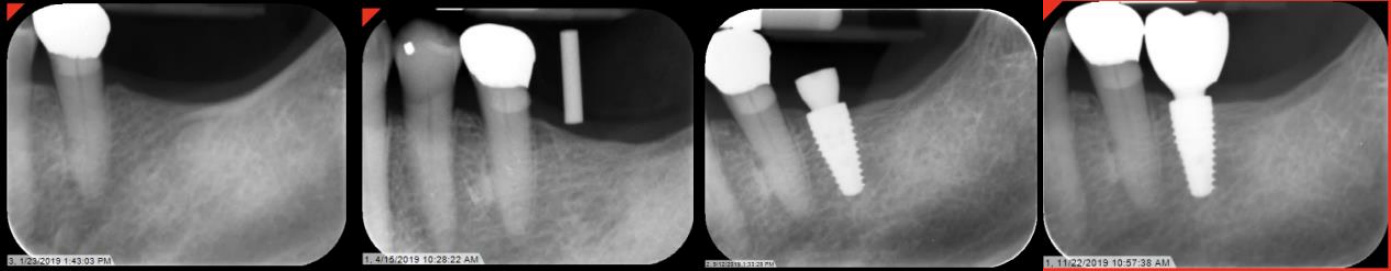
Implant Planning and Restoration #3 and #19
Site #3 Restoration Sequence
Site #19 Restoration Sequence
Final Intraoral Photographs
Models
Mounted Final casts
Sources
Caries Risk Assessment Form (Age 6). (2011). Retrieved January 17, 2021, from www.ada.org
The American Dental Association Caries Classification System for Clinical Practice. (2015, February). Retrieved January 17, 2021, from jada.ada.org
Login to access

:sharpen(level=0):output(format=jpeg)/up/2023/05/Cynthia-Udeh-3.jpg)
:sharpen(level=0):output(format=jpeg)/up/2022/01/Whole-Mouth-Health-and-Preventive-Dentistry-for-Older-Adults-2.jpg)