Systemic Health and Implant Failure
Implant therapy has become a fundamental component of dental care. Treatment with dental implants has eliminated the need to include contiguous teeth in the treatment plan when only a single tooth requires replacement, and has provided clinicians with a series of options that allow replacement of teeth where before only a removable prosthesis was possible.1Busenlechner D, Fürhauser R, Haas R, Watzek G, Mailath G, Pommer B. Long-term implant success at the Academy for Oral Implantology: 8-year follow-up and risk factor analysis. J Periodontal Implant Sci 2014;44:102-8. http://dx.doi.org/10.5051/jpis.2014.44.3.102
Dental implant therapy has proven to be a remarkably successful clinical procedure, with a recent systematic review with a follow-up of more than 10 years finding a mean survival rate of 94.6% and a mean success rate of 89.7%.2Moraschini V, Poubel LA, Ferreira VF, Barboza Edos S. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: a systematic review. Int J Oral Maxillofac Surg 2015;44(3):377-88.
Complications
The large number of implants placed has meant that implant complications have become more common. Complications include mucosal inflammation (peri-implant mucositis), which untreated can progress to loss of bone support (peri-implantitis) and thereby implant failure.3American Academy of Periodontology. Peri-implant mucositis and peri-implantitis: A current understanding of their diagnoses and clinical implications. J Periodontol 2013;84(4):436-43. In addition, in older patients receiving implants, there is a higher probability of being diagnosed with a systemic/chronic disease or condition. An important concern is the potential impact of these conditions on implant complications and failure.
Systemic diseases and conditions
A recent report examined the association of dental implant failure and systemic diseases/conditions in 6,358 patients, with a follow-up of up to 31 years.4Carr AB, Revuru VS, Lohse CM. Association of systemic conditions with dental implant failures in 6,384 patients during a 31-year follow-up period. Int J Oral Maxillofac Implants 2017;32(5):1153-61. More than twenty systemic diseases/conditions were considered. Epidemiologic, medical and dental data were available for analysis. Implant failure was experienced by 713 patients, with a median time to first failure of 0.6 years. After adjusting for age, gender and follow-up period, none of the systemic conditions were found to increase risk for implant failure.
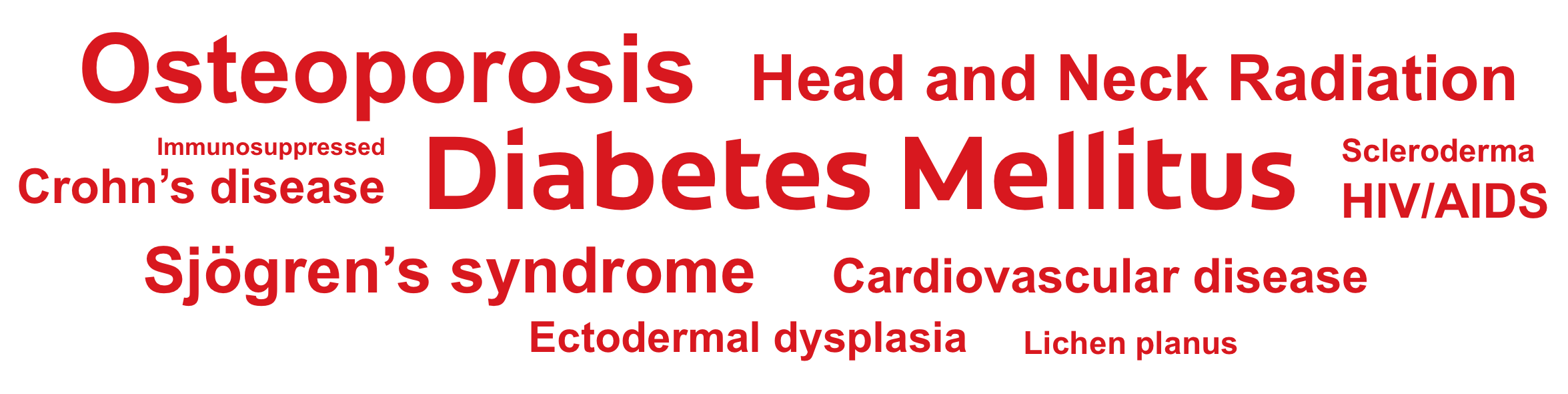
Figure 1
Systemic conditions/diseases considered in studies.
Other systematic reviews have also failed to find a clear association between systemic disorders and implant failure.5Bornstein MM, Cionca N, Mombelli A. Systemic conditions and treatments as risks for implant therapy. Int J Oral Maxillofac Implants 2009;24(Suppl):12-27.,6Guobis Z, Pacauskiene I, Astramskaite I. General diseases influence on peri-implantitis development: a systematic review. J Oral Maxillofac Res 2016;7(3):e5.,7Clementini M, Rossetti PH, Penarrocha D, Micarelli C, Bonachela WC, Canullo L. Systemic risk factors for peri-implant bone loss: a systematic review and meta-analysis. Int J Oral Maxillofac Surg 2014;43(3):323-34. Additionally, in a retrospective study including more than 200 patients and 1,000 implants, and with a minimum follow-up of at least 20 years and a maximum of 36 years, no differences in survival rates were observed for patients with and without type 2 diabetes, high blood pressure, immunosuppression, hypothyroidism or those taking bisphosphonates.8Chrcanovic BR, Kisch J, Albrektsson T, Wennerberg A. A retrospective study on clinical and radiological outcomes of oral implants in patients followed up for a minimum of 20 years. Clin Implant Dent Relat Res 2017 Dec 6. While the reviews and studies discussed found no associations for systemic diseases overall, this may mask the potential for complications as a result of a single disorder, conflicting findings and potential confounders. It is illustrative to examine specific disorders in greater detail.
Diabetes mellitus
However, further examination of these reviews and studies reveals several issues. Some reviews reported significant study heterogeneity, a lack of high-quality studies, and failure rates across individual studies varied considerably for control and test groups.13Naujokat H, Kunzendorf B, Wiltfang J. Dental implants and diabetes mellitus—a systematic review. Int J Implant Dent 2016;2:5. doi: 10.1186/s40729-016-0038-2.
| Table 1. Summary data for studies of patients with and without DM | |
|---|---|
| Study | Findings |
| Chen et al, 2013 | No statistically significant association found for implant failure and DM. |
| Oates et al, 2014 | Healing and osseointegration were delayed for patients with poor glycemic control. Similar success rates observed 1-year after implant loading, including for patients with poorly-controlled DM. |
| Moraschini et al, 2016 | Types 1 and 2 DM were not risk factors for implant failure. |
| Naujokat et al, 2016 | Similar implant survival rates for patients with well-controlled DM and without DM |
| Shi et al, 2016 | No direct association for implant failure and glycemic level. |
Irradiated bone
Conflicting outcomes and conclusions have been reported for implants placed in irradiated bone. In a pooled analysis of 16 studies, a more than two-fold increased risk of implant failure was found for implants placed in irradiated bone.10Chen H, Liu N, Xu X, Qu X, Lu E. Smoking, radiotherapy, diabetes and osteoporosis as risk factors for dental implant failure: a meta-analysis. PLoS One 2013;8:e71955. In addition, an almost three-fold increased risk for implant failure for implants placed in irradiated bone was found in a meta-analysis of 7 studies in a second systematic review, as well as and an almost six-fold risk for implants placed in irradiated bone in the maxilla compared to in the mandible.14Chambrone L, Mandia J Jr, Shibli JA, Romito GA, Abrahao M. Dental implants installed in irradiated jaws: a systematic review. J Dent Res 2013;92(12 Suppl):119S-30S.Other studies have compared survival rates for implants placed at different periods of time post-irradiation, or compared pre- or post-irradiation implant placement. In a review of 10 studies, it was concluded that implant placement less than 12 months after radiotherapy may result in a higher risk of failure.15Claudy MP, Miguens SA Jr, Celeste RK, Camara Parente R, Hernandez PA, da Silva AN Jr. Time interval after radiotherapy and dental implant failure: systematic review of observational studies and meta-analysis. Clin Implant Dent Relat Res 2015;17(2):402-11. doi: 10.1111/cid.12096. Similar implant survival rates were found for dental implants placed pre- and post-irradiation in a systematic review of 19 studies reported between 1990 and 2006,16Colella G, Cannavale R, Pentenero M, Gandolfo S. Oral implants in radiated patients: A systematic review. Int J Oral Maxillofac Impl 2007;22:616-22. as well as in a separate review of articles published between 1990 and 2012.17Nooh N. Dental implant survival in irradiated oral cancer patients: a systematic review of the literature. Int J Oral Maxillofac Implants 2013;28(5):1233-42.
It is difficult to draw conclusions due to the heterogeneity and variable quality of existing studies, and the lack of robust controlled studies. For example, excluding one study from the meta-analysis in one review reduced the increased risk of implant failure attributed to timing of implant placement from 34% to 8%, two studies involved placement before the stated inclusion period, and selection bias was evident.15Claudy MP, Miguens SA Jr, Celeste RK, Camara Parente R, Hernandez PA, da Silva AN Jr. Time interval after radiotherapy and dental implant failure: systematic review of observational studies and meta-analysis. Clin Implant Dent Relat Res 2015;17(2):402-11. doi: 10.1111/cid.12096. In another review, radiation exposures ranged from 36 to 72 Gy, failure rates for individual studies varied greatly, and it was not reported whether implant placement occurred before or after radiation therapy.10Chen H, Liu N, Xu X, Qu X, Lu E. Smoking, radiotherapy, diabetes and osteoporosis as risk factors for dental implant failure: a meta-analysis. PLoS One 2013;8:e71955. In addition, while higher implant failure rates have been found for patients who received high-dose radiation therapy, high-dose was defined in different studies as >55 Gy, >50 Gy and >45 Gy.17Nooh N. Dental implant survival in irradiated oral cancer patients: a systematic review of the literature. Int J Oral Maxillofac Implants 2013;28(5):1233-42.,18Granström G. Osseointegration in irradiated cancer patients: An analysis with respect to implant failures. J Oral Maxillofac Surg 2005;63:579-85.,19Curi MM, Condezo AFB, Ribeiro KDCB, Cardoso CL. Long-term success of dental implants in patients with head and neck cancer after radiation therapy. Int J Oral Maxillofac Surg 2018 Feb 6. pii: S0901-5027(18)30028-6. doi: 10.1016/j.ijom.2018.01.012. [Epub ahead of print] Considered in total, these studies do, however, suggest that the radiation dose and the method of radiation delivery impacts implant outcomes.
Other Conditions
Systematic reviews have also been conducted in patients with and without osteoporosis.8Chrcanovic BR, Kisch J, Albrektsson T, Wennerberg A. A retrospective study on clinical and radiological outcomes of oral implants in patients followed up for a minimum of 20 years. Clin Implant Dent Relat Res 2017 Dec 6.,20de Medeiros FCFL, Kudo GAH, Leme BG, Saraiva PP, Verri FR, Honório HM, Pellizzer EP, Santiago Junior JF. Dental implants in patients with osteoporosis: a systematic review with meta-analysis. Int J Oral Maxillofac Surg 2018;47(4):480-91.,21Temmerman A, Rasmusson L, Kubler A, Thor A, Quirynen M. An open, prospective, non-randomized, controlled, multicentre study to evaluate the clinical outcome of implant treatment in women over 60 years of age with osteoporosis/osteopenia: 1-year results. Clin Oral Implants Res 2017;28:95-102.,22Giro G, Chambrone L, Goldstein A, Rodrigues JA, Zenóbio E, Feres M, Figueiredo LC, Cassoni A, Shibli JA. Impact of osteoporosis in dental implants: A systematic review. World J Orthop 2015;6(2):311-5. In one recent meta-analysis of 15 studies with a total of almost 9,000 patients and 30,000 implants, no statistically significant differences were found for implant survival at the individual or patient level.20de Medeiros FCFL, Kudo GAH, Leme BG, Saraiva PP, Verri FR, Honório HM, Pellizzer EP, Santiago Junior JF. Dental implants in patients with osteoporosis: a systematic review with meta-analysis. Int J Oral Maxillofac Surg 2018;47(4):480-91. However, nuances are also apparent across studies. Peri-implantitis was evaluated in only one study, and studies did not consistently report whether the onset of osteoporosis preceded or followed dental implant therapy and/if bisphosphonate therapy was initiated before or after implant placement.20de Medeiros FCFL, Kudo GAH, Leme BG, Saraiva PP, Verri FR, Honório HM, Pellizzer EP, Santiago Junior JF. Dental implants in patients with osteoporosis: a systematic review with meta-analysis. Int J Oral Maxillofac Surg 2018;47(4):480-91.,21Temmerman A, Rasmusson L, Kubler A, Thor A, Quirynen M. An open, prospective, non-randomized, controlled, multicentre study to evaluate the clinical outcome of implant treatment in women over 60 years of age with osteoporosis/osteopenia: 1-year results. Clin Oral Implants Res 2017;28:95-102.,22Giro G, Chambrone L, Goldstein A, Rodrigues JA, Zenóbio E, Feres M, Figueiredo LC, Cassoni A, Shibli JA. Impact of osteoporosis in dental implants: A systematic review. World J Orthop 2015;6(2):311-5.,23Dvorak G, Arnhart C, Heuberer S, Huber CD, Watzek G, Gruber R. Peri-implantitis and late implant failures in postmenopausal women: a cross-sectional study. J Clin Periodontol 2011;38:950-5.,24Walter C, Al-Nawas B, Wolff T, Schiegnitz E, Grötz KA. Dental implants in patients treated with antiresorptive medication – a systematic literature review. Int J Impl Dent 2016;2:9.,25Hellstein JW, Adler RA, Edwards B, Jacobsen PL, Kalmar JR, Koka S, Migliorati CA, Ristic H; American Dental Association Council on Scientific Affairs Expert Panel on Antiresorptive Agents. Managing the care of patients receiving antiresorptive therapy for prevention and treatment of osteoporosis: executive summary of recommendations from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc 2011;142(11):1243-51. There is limited data available for other systemic/chronic diseases. A 93.7% survival rate was found for implants placed in patients with Sjögren’s syndrome with a mean follow-up of 4 years in a recent systematic review, which was limited to one case study, one prospective and four retrospective studies.26Almeida D, Vianna K, Arriaga P, Moraschini V. Dental implants in SjoÈgren’s syndrome patients: A systematic review. PLoS One 2017;12(12): e0189507. https://doi.org/10.1371/journal.pone.0189507 Further, limited data on implant outcomes is available for patients with cardiovascular disease, and even less for patients with HIV/AIDS, Crohn’s disease, ectodermal dysplasia, lichen planus, scleroderma, or for patients taking immunosuppressants.5Bornstein MM, Cionca N, Mombelli A. Systemic conditions and treatments as risks for implant therapy. Int J Oral Maxillofac Implants 2009;24(Suppl):12-27.,27Paredes V, López-Pintor RM, Torres J, de Vicente JC, Sanz M, Hernández G. Implant treatment in pharmacologically immunosuppressed liver transplant patients: A prospective-controlled study. Clin Oral Implants Res 2018;29(1):28-35.
Conclusions
The results of systematic reviews indicate that “systemic disease” in the broadest sense is not a contraindication to implant therapy, and disorders such as diabetes, irradiated bone and osteoporosis do not disqualify patients from receiving dental implants.
However, as noted, studies in the reviews were heterogeneous, at varying levels of risk of bias, and there is a paucity of truly robust studies. In addition, far fewer studies have evaluated implant success, i.e., an absence of complications, including peri-implantitis. Further, for other conditions there is a lack of, or limited, available data. This issue will become increasingly important as the population ages and more individuals with systemic/chronic diseases could benefit from implant therapy.
Implant maintenance protocols were recently introduced that could improve long-term implant outcomes28Bidra AS, Daubert DM, Garcia LT, Kosinski TF, Nenn CA, Olsen JA, Platt JA, Wingrove SS, Chandler ND, Curtis DA. Clinical practice guidelines for recall and maintenance of patients with tooth-borne and implant-borne dental restorations. J Am Dent Assoc 2016;147(1):67-74. and medical management of chronic diseases/conditions continues to evolve. Though not thoroughly examined in the reviews, the relative success of medical management of specific disorders should be a critical factor in determining the best course of treatment for patients. Each patient must be evaluated separately when deciding upon a course of treatment, other health professionals should be consulted, and potential concerns should be discussed with patients.
References
- 1.Marui VC, Souto MLS, Rovai ES, Romito GA, Chambrone L, Pannuti CM. Efficacy of preprocedural mouthrinses in the reduction of microorganisms in aerosol: A systematic review. J Am Dent Assoc 2019;150(12):1015-26.e1. doi: 10.1016/j.adaj.2019.06.024.
- 2.Sreenivasan PK, Gittins E. The effects of a chlorhexidine mouthrinse on culturable micro-organisms of the tongue and saliva. Microbiol Res 2004;159(4):365-70.
- 3.Larsen PE. The effect of a chlorhexidine rinse on the incidence of alveolar osteitis following the surgical removal of impacted mandibular third molars. J Oral Maxillofac Surg 1991;49(9):932-37.
- 4.Hennessy B, Joyce A. A survey of preprocedural antiseptic mouth rinse use in Army dental clinics. Mil Med 2004;169(8):600-3.
- 5.American Dental Association. Interim Guidance for Minimizing Risk of COVID-19 Transmission. Available at: https://www.ada.org/~/media/CPS/Files/COVID/ADA_COVID_Int_Guidance_Treat_Pts.pdf.
- 6.Meng L, Fang H, Bian Z.. Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine. J Dent Res 2020;99. 002203452091424. 10.1177/0022034520914246.
- 7.Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci 2020;12:9.
- 8.Kobza J, Pastuszka JS, Brągoszewska E. Do exposures to aerosols pose a risk to dental professionals? Occupat Med 2018;68(7):454-8.
- 9.Tellier, Li Y, Cowling BJ, Tang JW. Recognition of aerosol transmission of infectious agents: a commentary. BMC Infect Dis 2019;19:101. Available at: https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-019-3707-y.
- 10.Grenier D. Quantitative analysis of bacterial aerosols in two different dental clinic environments. Appl Environ Microbiol 1995;61(8):3165-8.
- 11.Al Maghlouth A, Al Yousef Y, Al Bagieh N. Qualitative and quantitative analysis of bacterial aerosols. J Contemp Dent Pract. 2004 Nov 15;5(4):91-100.
- 12.Feres M, Figueiredo LC, Faveri M, Stewart B, de Vizio W. The effectiveness of a preprocedural mouthrinse containing cetylpyridinium chloride in reducing bacteria in the dental office. J Am Dent Assoc 2010;141:415-22.
- 13.Domingo MA, Farrales MS, Loya RM, Pura MA, Uy H. The effect of 1% povidone-iodine as a pre-procedural mouthrinse in 20 patients with varying degrees of oral hygiene. J Philipp Dent Assoc 1996;48(2):31-8.
- 14.DePaola LG, Eshenaur Spolarich A. Safety and Efficacy of Antimicrobial Mouthrinses in Clinical Practice. J Dent Hyg 2007;81(suppl 1) 117. Available at: https://jdh.adha.org/content/jdenthyg/81/suppl_1/117.full.pdf.
- 15.Scheie AA. Modes of action of currently known chemical antiplaque agents other than chlorhexidine. J Dent Res 1989;68 (Spec Iss):1609-16.
- 16.Nazzaro F, Fratianni F, De Martino L, Coppola R, De Feo V. Effect of essential oils on pathogenic bacteria. Pharmaceuticals (Basel) 2013;6(12):1451‐74. doi:10.3390/ph6121451.
- 17.Prescribers Digital Reference. povidone iodine – Drug Summary. Available at: https://www.pdr.net/drug-summary/Betadine-5–povidone-iodine-2152.
- 18.Litsky BY, Mascis JD, Litsky W. Use of an antimicrobial mouthwash to minimize the bacterial aerosol contamination generated by the high-speed drill. PlumX Metrics. Available at: https://doi.org/10.1016/0030-4220(70)90407-X.
- 19.Wyler D, Miller RL, Micik RE. Efficacy of self-administered preoperative oral hygiene procedures in reducing the concentration of bacteria in aerosols generated during dental procedures. J Dent Res 1971;50(2):509.
- 20.Logothetis DD, Martinez-Welles JM. Reducing bacterial aerosol contamination with a chlorhexidine gluconate pre-rinse. J Am Dent Assoc 1995;126(12):1634-9.
- 21.Klyn SL, Cummings DE, Richardson BW, Davis RD. Reduction of bacteria-containing spray produced during ultrasonic scaling. Gen Dent 2001;49(6):648-52.
- 22.Fine DH, Mendieta C, Barnett ML, Furgang D, Meyers R. Efficacy of preprocedural rinsing with an antiseptic in reducing viable bacteria in dental aerosols. J Periodontol 1992;63(10):821-4.
- 23.Fine DH, Furgang D, Korik I, Olshan A, Barnett ML, Vincent JW. Reduction of viable bacteria in dental aerosols by preprocedural rinsing with an antiseptic mouthrinse. Am J Dent 1993;6(5):219-21.
- 24.Altonen M, Saxen L, Kosunen T, Ainamo J. Effect of two antimicrobial rinses and oral prophylaxis on preoperative degerming of saliva. Int J Oral Surg 1976;5(6):276-84.
- 25.Veksler AE, Kayrouz GA, Newman MG. Reduction of salivary bacteria by pre-procedural rinses with chlorhexidine 0.12%. J Periodontol 1991;62(11):649-51.
- 26.Balbuena L, Stambaugh KI, Ramirez SG, Yeager C. Effects of topical oral antiseptic rinses on bacterial counts of saliva in healthy human subjects. Otolaryngol Head Neck Surg 1998;118(5):625-9.
- 27.Kirk-Bailey J, Combes J, Sunkaraneni S, Challacombe S. The use of Povidone Iodine nasal spray and mouthwash during the current COVID-19 pandemic for the reduction of cross infection and protection of healthcare workers. Last revised 24 April 2020. Available at: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3563092.
- 28.To KK-W, Tsang OT-Y, Yip C-YC, Chan K-H, Wu T-C, Chan JM-C, et al. Consistent detection of 2019 novel coronavirus in saliva. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 2020;361:1319. doi:10.1093/cid/ciaa149.
- 29.Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, et al. SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients. N Engl J Med 2020;382:1177-9.
- 30.van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020. Available at: https://www.nejm.org/doi/full/10.1056/NEJMc2004973.
- 31.Guo Z-D, Wang Z-Y, Zhang S-F, Li X, Li L, Li C, et al. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerg Infect Dis 2020 Jul [date cited]. https://doi.org/10.3201/eid2607.200885.
- 32.Caruso AA, Del Prete A, Lazzarino AI, Capaldi R, Grumetto L. May hydrogen peroxide reduce the hospitalization rate and complications of SARS-CoV-2 infection? Letter to the Editor. Infection Control & Hospital Epidemiology as part of the Cambridge Coronavirus Collection. doi: 10.1017/ice.2020.170.
- 33.Centers for Disease Control and Prevention. Chemical Disinfectants
Guideline for Disinfection and Sterilization in Healthcare Facilities (2008). Available at:
https://www.cdc.gov/infectioncontrol/guidelines/disinfection/disinfection-methods/chemical.html#Hydrogen. - 34.Eggers, M. Infectious Disease Management and Control with Povidone Iodine. Infect Dis Ther 2019;8:581-93.
- 35.Kanagalingam J, Feliciano R, Hah JH, Labib H, Le TA, Lin JC. Practical use of povidone-iodine antiseptic in the maintenance of oral health and in the prevention and treatment of common oropharyngeal infections. Int J Clin Pract 2015;69(11):1247-56. doi: 10.1111/ijcp.12707.
- 36.Tiwari T, Jamieson L, Broughton J, Lawrence HP, Batliner TS, Arantes R, Albino J. Reducing indigenous oral health inequalities: A review from 5 nations. J Dent Res 2018;97(8):869-77.
- 37.Flynn P, Acharya A, Schwei K, VanWormer J, Skrzypcak K. Assessing dental hygienists’ communication techniques for use with low oral health literacy patients. J Dent Hyg 2016;90(3):162-9.
- 38.Aldoory L, Macek MD, Atchison KA, Chen H. Comparing well-tested health literacy measures for oral health: A pilot assessment. Health Commun 2016;21(11):1161-9.


:sharpen(level=0):output(format=jpeg)/up/2023/05/Fiona-Collins-thumbnail-1-3.jpg)
:sharpen(level=0):output(format=jpeg)/up/2023/05/Ira-Lamster-3.jpg)
:sharpen(level=0):output(format=jpeg)/up/2018/07/Systemic-Health-and-Implant-Failure-2.jpg)