Technology Regenerative Endodontics
Endodontic therapy is required to treat teeth with partial or complete necrosis of the pulpal tissues, typically resulting from dental trauma or infection of the pulp by cariogenic microorganisms that have penetrated through the enamel and dentin. For permanent teeth with mature roots, endodontic treatment is routinely provided, with high survival rates.1Alley BS, Kitchens GG, Alley LW, Eleazer PD. A comparison of survival of teeth following endodontic treatment performed by general dentists or specialists. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 2004;98(1):115-8. However, dental caries and trauma are estimated to result in pulpal necrosis and tooth loss in more than 5 million children and adolescents annually in the United States alone.2He L, Zhong J, Gong Q, Kim SG, Zeichner SJ, Xiang L, Ye L, Zhou X, Zheng J, Liu Y, Guan C, Cheng B, Ling J, Mao JJ. Treatment of necrotic teeth by apical revascularization: Meta-analysis. Sci Reports 2017;7:13941. Dens invaginatus can also result in pulpal necrosis.3Plascencia H, Díaz M, Moldauer BI, Uribe M, Skidmor E. Non-surgical endodontic management of Type II dens invaginatus with closed and open apex. Iran Endod J 2017;12(4):534-9. Endodontic treatment for immature permanent teeth is challenging. Options include apexification and, more recently, regenerative endodontics.
Apexification of immature permanent teeth with pulpal necrosis
Traditional approaches for treating immature permanent teeth with necrotic pulpal tissue have included multi-visit apexification using calcium hydroxide (CH) to induce a calcified apical barrier, and single-visit apexification using mineral trioxide aggregate (MTA) to form an apical barrier prior to root canal filling.4Garcia-Godoy F, Murray PE. Recommendations for using regenerative endodontic procedures in permanent immature traumatized teeth. Dent Traumatol 2012;28:33-41. While apexification is usually successful, further root development does not occur, and complications can include a poor crown-to-root ratio and cervical root fracture associated with the thin dentinal walls.5Silveira CMM, Sebrão CCN, Vilanova LSR, Sanchez-Ayala A. Apexification of an immature permanent incisor with the use of calcium hydroxide: 16-year follow-up of a case. Case Rep Dent 2015:984590. Dentin is also weakened by long-term use of CH, increasing the risk of fracture, which is estimated to occur in approximately 46% of treated of teeth within 9 years.4Garcia-Godoy F, Murray PE. Recommendations for using regenerative endodontic procedures in permanent immature traumatized teeth. Dent Traumatol 2012;28:33-41.,6Lin J, Zeng Q, Wei X, Zhao W, Cui M, Gu J, Lu J, Yang M, Ling J. Regenerative endodontics versus apexification in immature permanent teeth with apical periodontitis: A prospective randomized controlled study. J Endod 2017;43(11):1821-7.,7Singh RK, Shakya VK, Khanna R, Singh BP, Jindal G, Kirubakaran R, Sequeira-Byron P. Interventions for managing immature permanent teeth with necrotic pulps. Cochrane Database Syst Rev 2017;CD012709.,8Cvek M. Prognosis of luxated non-vital maxillary incisors treated with calcium hydroxide and filled with gutta-percha: a retrospective clinical study. Endod Dent Traumatol 1992;8:45-55.,9Thibodeau B, Trope M. Pulp revascularization of a necrotic infected immature permanent tooth: case report and review of the literature. Pediatr Dent 2007;29(1):47-50.
Regenerative endodontic therapy
The emergence of regenerative endodontic therapy (RET) represents a shift to a focus on revascularization, tissue regeneration and continued root development.10Lin LM, Kahler B. A review of regenerative endodontics: current protocols and future directions. J Istanb Univ Fac Dent 2017;51(3 Suppl 1):S41-S51. The primary, secondary and tertiary goals for RET are resolution of clinical signs and symptoms, continued root maturation and a positive response to vitality testing, respectively.11American Academy of Endodontists. Clinical Considerations for a Regenerative Procedure, Revised 6-8-16. Available at: https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/currentregenerativeendodonticconsiderations.pdf,12Kahler B, Rossi-Fedele G, Chugal N, Lin LM. An evidence-based review of the efficacy of treatment approaches for immature permanent teeth with pulp necrosis. J Endod 2017;43(7):1052-7.
The protocol suggested by the American Academy of Endodontists involves two treatment visits.11American Academy of Endodontists. Clinical Considerations for a Regenerative Procedure, Revised 6-8-16. Available at: https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/currentregenerativeendodonticconsiderations.pdf Instrumentation of the dentinal walls is generally not recommended, unless minimal instrumentation is needed to help disrupt biofilm.10Lin LM, Kahler B. A review of regenerative endodontics: current protocols and future directions. J Istanb Univ Fac Dent 2017;51(3 Suppl 1):S41-S51. At the first visit, after rubber dam placement, the root canals are each gently irrigated for 5 minutes using 20 ml of 1.5% sodium hypochlorite (NaOCl) then irrigated for 5 minutes with 20 ml of ethylenediaminetetraacetic acid (EDTA) or saline, using a safe irrigation system (e.g., an irrigation needle with side vents and a closed end) and keeping the irrigation needle 1 mm away from the open apex to prevent periapical extrusion of the irrigant.11American Academy of Endodontists. Clinical Considerations for a Regenerative Procedure, Revised 6-8-16. Available at: https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/currentregenerativeendodonticconsiderations.pdf The root canals are then dried before placing CH or double/triple antibiotic paste into the canals and sealing the canals coronally with a temporary restoration.
At the second visit 1 to 4 weeks later, provided there are no signs/symptoms of infection, local anesthetic without vasoconstrictor is administered and the canals gently irrigated with 20 ml of 17% EDTA before being dried. The periapical tissue is briefly over-instrumented 2 mm beyond the open apex to cause bleeding and to produce a blood clot extending in the canals up to the CEJ. A resorbable matrix may be placed over the clot before placing MTA/tricalcium silicate cement/bioceramic over it, and then a restorative material. (Figure 1) Reassessment is recommended every 6 months for 2 years to evaluate bony healing, ideally with no symptoms, and continued root development.10Lin LM, Kahler B. A review of regenerative endodontics: current protocols and future directions. J Istanb Univ Fac Dent 2017;51(3 Suppl 1):S41-S51.,11American Academy of Endodontists. Clinical Considerations for a Regenerative Procedure, Revised 6-8-16. Available at: https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/currentregenerativeendodonticconsiderations.pdf
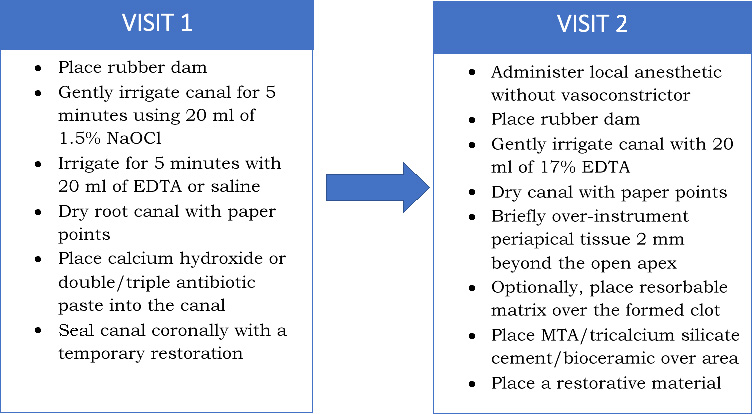
Figure 1
Recommended steps in RET11American Academy of Endodontists. Clinical Considerations for a Regenerative Procedure, Revised 6-8-16. Available at: https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/currentregenerativeendodonticconsiderations.pdf
Biologic Mechanism to Explain RET
The blood clot formed during RET acts as a scaffold and as a matrix containing undifferentiated mesenchymal (stem) cells.7Singh RK, Shakya VK, Khanna R, Singh BP, Jindal G, Kirubakaran R, Sequeira-Byron P. Interventions for managing immature permanent teeth with necrotic pulps. Cochrane Database Syst Rev 2017;CD012709.,13Nazzal H, Duggal MS. Regenerative endodontics: a true paradigm shift or a bandwagon about to be derailed? Eur Arch Paediatr Dent 2017;18(1):3-15. The stem cells are believed to be largely derived from the apical papilla and, together with Hertwig’s epithelial root sheath (HERS) cells, to be responsible for continued root development.7Singh RK, Shakya VK, Khanna R, Singh BP, Jindal G, Kirubakaran R, Sequeira-Byron P. Interventions for managing immature permanent teeth with necrotic pulps. Cochrane Database Syst Rev 2017;CD012709. During RET, a low concentration of NaOCl is recommended to minimize cytotoxic effects on stem cells.7Singh RK, Shakya VK, Khanna R, Singh BP, Jindal G, Kirubakaran R, Sequeira-Byron P. Interventions for managing immature permanent teeth with necrotic pulps. Cochrane Database Syst Rev 2017;CD012709.,11American Academy of Endodontists. Clinical Considerations for a Regenerative Procedure, Revised 6-8-16. Available at: https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/currentregenerativeendodonticconsiderations.pdf,14Kahler B, Chugal N, Lin LM. Alkaline materials and regenerative endodontics: A review. Materials 2017;10:1389. In addition, growth factors are released from dentin during irrigation with 17% EDTA which may also increase the viability of stem cells derived from the apical papilla and their attachment to dentin.10Lin LM, Kahler B. A review of regenerative endodontics: current protocols and future directions. J Istanb Univ Fac Dent 2017;51(3 Suppl 1):S41-S51.,15Trevino EG, Patwardhan AN, Henry MA, Perry G, Dybdal-Hargreaves N, Hargreaves KM, Diogenes A. Effect of irrigants on the survival of human stem cells of the apical papilla in a platelet-rich plasma scaffold in human root tips. J Endod 2011;37(8):1109-15. However, while HERS cells are able to promote differentiation of pulp stem cells and thereby dentin repair, they have not been shown to differentiate mesenchymal stem cells contained in blood clots.10Lin LM, Kahler B. A review of regenerative endodontics: current protocols and future directions. J Istanb Univ Fac Dent 2017;51(3 Suppl 1):S41-S51. Intraorally, stem cells can also be sourced from the dental pulp, periodontal ligament and as inflamed periapical progenitor cells.13Nazzal H, Duggal MS. Regenerative endodontics: a true paradigm shift or a bandwagon about to be derailed? Eur Arch Paediatr Dent 2017;18(1):3-15. In addition, it is suggested that bioactive peptides and immune cells in the blood forming the blood clot may possess antimicrobial activity and aid the removal of microorganisms within the canals.16Saoud TMA, Ricucci D, Lin LM, Gaengler P. Regeneration and repair in endodontics. A special issue of the regenerative endodontics - a new era in clinical endodontics. Dent J (Basel) 2016;4(1).
Clinical outcomes
In a review of 6 cohort studies, similar outcomes were found for RET and apexification using CH or an MTA barrier technique.12Kahler B, Rossi-Fedele G, Chugal N, Lin LM. An evidence-based review of the efficacy of treatment approaches for immature permanent teeth with pulp necrosis. J Endod 2017;43(7):1052-7. Four of the 6 studies reported survival rates, with survival rates for RET and apexification of 98.6% and 88.6%, respectively. No significant differences were found for healing or increases in bone density, and continued root development following RET varied.12Kahler B, Rossi-Fedele G, Chugal N, Lin LM. An evidence-based review of the efficacy of treatment approaches for immature permanent teeth with pulp necrosis. J Endod 2017;43(7):1052-7. In one of the 4 studies, increases in root length were 14.9%, 0.4% and 6.1%, respectively, for RET, CH apexification and the MTA barrier technique.17Jeeruphan T, Jantarat J, Yanpiset K, Suwannapan L, Khewsawai P, Hargreaves KM. Mahidol study 1: comparison of radiographic and survival outcomes of immature teeth treated with either regenerative endodontic or apexification methods: a retrospective study. J Endod 2012 Oct;38(10):1330-6. (Figure 2) Increases in root width, and survival rates, were also greatest for RET. However, as noted in the review, there was heterogeneity regarding mean follow-up periods, the teeth that were treated, and the etiology of pulpal necrosis.12Kahler B, Rossi-Fedele G, Chugal N, Lin LM. An evidence-based review of the efficacy of treatment approaches for immature permanent teeth with pulp necrosis. J Endod 2017;43(7):1052-7.
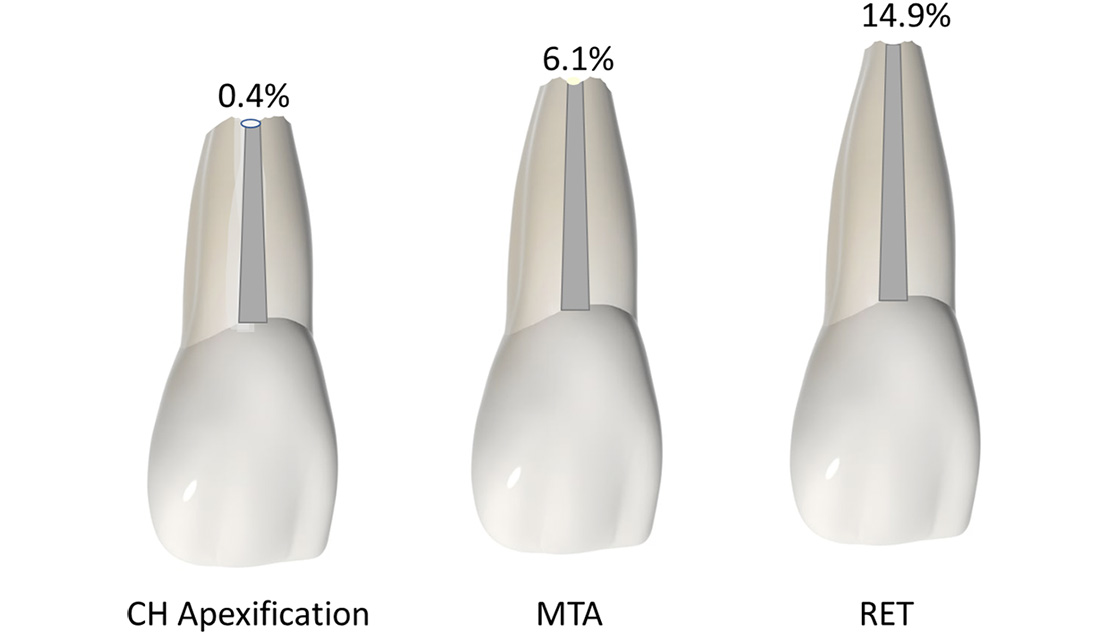
Figure 2
Increases in root length following RET, CH apexification and the MTA barrier technique17Jeeruphan T, Jantarat J, Yanpiset K, Suwannapan L, Khewsawai P, Hargreaves KM. Mahidol study 1: comparison of radiographic and survival outcomes of immature teeth treated with either regenerative endodontic or apexification methods: a retrospective study. J Endod 2012 Oct;38(10):1330-6.
In a meta-analysis of 22 studies with a follow-up period ranging from 6 to 66 months, RET was found to result in apical closure in approximately 39% of clinical cases.2He L, Zhong J, Gong Q, Kim SG, Zeichner SJ, Xiang L, Ye L, Zhou X, Zheng J, Liu Y, Guan C, Cheng B, Ling J, Mao JJ. Treatment of necrotic teeth by apical revascularization: Meta-analysis. Sci Reports 2017;7:13941. An apical bridge formed in 47% of cases (in the remaining cases the apices were found to be open). No significant increases in root length were found at the subject level and increases in the area of root dentin were only found for roots with closed apices.2He L, Zhong J, Gong Q, Kim SG, Zeichner SJ, Xiang L, Ye L, Zhou X, Zheng J, Liu Y, Guan C, Cheng B, Ling J, Mao JJ. Treatment of necrotic teeth by apical revascularization: Meta-analysis. Sci Reports 2017;7:13941. In comparing clinical outcomes, survival rates for RET and apexification using MTA were 97.8% and 97.1%, respectively, and success rates were 91.3% and 94.6%, respectively. (Figure 3) No statistically significant differences were found for the two interventions.18Torabinejad M, Nosrat A, Verma P, Udochukwu O. Regenerative endodontic treatment or mineral trioxide aggregate apical plug in teeth with necrotic pulps and open apices: a systematic review and meta-analysis. J Endod 2017;43(11):1806-20.
Figure 3.
Survival and success rates for RET and apexification18Torabinejad M, Nosrat A, Verma P, Udochukwu O. Regenerative endodontic treatment or mineral trioxide aggregate apical plug in teeth with necrotic pulps and open apices: a systematic review and meta-analysis. J Endod 2017;43(11):1806-20.
Adverse events associated with RET
Root resorption, apical periodontitis, tooth discoloration and treatment failure due to infection and pain may occur following RET.19López C, Mendoza A, Solano B, Yáñez-Vico R. Revascularization in immature permanent teeth with necrotic pulp and apical pathology: case series. Case Reports Dent 2017; Article ID 3540159.,20Kahler B, Rossi-Fedele G. A review of tooth discoloration after regenerative endodontic therapy. J Endod 2016;42(4):563-9. In a systematic review of 80 studies with almost 400 teeth, tooth discoloration was more likely for teeth treated with a triple antibiotic paste containing minocycline, ciprofloxacin and metronidazole than with CH paste or a double antibiotic paste containing no mincocycline.20Kahler B, Rossi-Fedele G. A review of tooth discoloration after regenerative endodontic therapy. J Endod 2016;42(4):563-9. To help prevent or reduce tooth discoloration, cefaclor or amoxicillin can be substituted for minocycline in triple antibiotic paste, or a double antibiotic paste can be used.11American Academy of Endodontists. Clinical Considerations for a Regenerative Procedure, Revised 6-8-16. Available at: https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/currentregenerativeendodonticconsiderations.pdf,21Santos LG, Felippe WT, Souza BD, Konrath AC, Cordeiro MM, Felippe MC. Crown discoloration promoted by materials used in regenerative endodontic procedures and effect of dental bleaching: spectrophotometric analysis. J Appl Oral Sci 2017;25(2):234-42.,22Moodley DS, Peck C, Moodley T, Patel N. Management of necrotic pulp of immature permanent incisor tooth: A regenerative endodontic treatment protocol: case report. S Afr Dent J 2017;72(3):122-5. If triple antibiotic paste containing minocycline is used, it should be placed only below the cementoenamel junction.11American Academy of Endodontists. Clinical Considerations for a Regenerative Procedure, Revised 6-8-16. Available at: https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/currentregenerativeendodonticconsiderations.pdf Sealing the coronal aspect of the root canals with glass ionomer cement or MTA has been found to be ineffective in preventing staining.21Santos LG, Felippe WT, Souza BD, Konrath AC, Cordeiro MM, Felippe MC. Crown discoloration promoted by materials used in regenerative endodontic procedures and effect of dental bleaching: spectrophotometric analysis. J Appl Oral Sci 2017;25(2):234-42. MTA, which contains bismuth oxide or another agent for radiopacity, is also known to cause discoloration.13Nazzal H, Duggal MS. Regenerative endodontics: a true paradigm shift or a bandwagon about to be derailed? Eur Arch Paediatr Dent 2017;18(1):3-15.,20Kahler B, Rossi-Fedele G. A review of tooth discoloration after regenerative endodontic therapy. J Endod 2016;42(4):563-9. (Table 1)
| Table 1. Methods for reducing potential tooth discoloration |
|---|
| Use a double antibiotic paste instead of triple antibiotic paste |
| Use a triple antibiotic paste replacing minocycline with cefaclor |
| Use a triple antibiotic paste replacing minocycline with amoxicillin |
| Use a material other than MTA to seal the area |
Potential factors in inconsistent root development
Several factors have been proposed for inconsistent root development following RET, including variations in protocols. Blood clots may be incapable of attracting regeneration-inducing cells, and apical bridges may be areas of mineralization rather than resulting in a closed apex.2He L, Zhong J, Gong Q, Kim SG, Zeichner SJ, Xiang L, Ye L, Zhou X, Zheng J, Liu Y, Guan C, Cheng B, Ling J, Mao JJ. Treatment of necrotic teeth by apical revascularization: Meta-analysis. Sci Reports 2017;7:13941. Stem cell differentiation requires HERS cells and they can produce cementum. The amount of damage to HERS cells due to trauma or during RET has also been proposed to explain inconsistent outcomes.13Nazzal H, Duggal MS. Regenerative endodontics: a true paradigm shift or a bandwagon about to be derailed? Eur Arch Paediatr Dent 2017;18(1):3-15.
Other considerations
There is significant heterogeneity in the approach to regenerative endodontics.14Kahler B, Chugal N, Lin LM. Alkaline materials and regenerative endodontics: A review. Materials 2017;10:1389. In one review, 97% of clinical studies used a protocol that included irrigation with NaOCl.14Kahler B, Chugal N, Lin LM. Alkaline materials and regenerative endodontics: A review. Materials 2017;10:1389. However, in a web-based survey of endodontists, 60% of respondents reported using a variety of protocols, irrigants and medicaments.23Lee JY, Kersten DD, Mines P, Beltran TA. Regenerative endodontic procedures among endodontists: A web-based survey. J Endod 2018;44(2):250-5. For example, during irrigation at the first visit, NaOCl at concentrations of <1.5%, 1.5%, 1.6% to 3% and >3% was used by 9.6%, 23.7%, 22.7% and 36.7% of endodontists, respectively. Other irrigants in addition to NaOCl and EDTA were reported. For intracanal medicaments, approximately 52% used calcium hydroxide, 23.5% used a triple and 17.5% a double antibiotic paste, and the remainder used another or no medicament.
Figure 4. Reported use of sodium hypochlorite concentrations23Lee JY, Kersten DD, Mines P, Beltran TA. Regenerative endodontic procedures among endodontists: A web-based survey. J Endod 2018;44(2):250-5.
Such heterogeneity is highlighted by reports examining approaches to RET. Platelet-rich plasma (PRP), platelet-rich fibrin and autologous fibrin matrix have been used as alternative scaffolds.11American Academy of Endodontists. Clinical Considerations for a Regenerative Procedure, Revised 6-8-16. Available at: https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/currentregenerativeendodonticconsiderations.pdf,24Yang H, Shi L, Chen H, Yin Z, Li P. Clinical efficacy of platelet rich fibrin in tooth pulp revascularization in treating periapical periodontitis of immature permanent teeth. J Biosci Med 2016;6. In one study comparing PRP and blood clots, 93% of teeth in the PRP group showed continued root development, and 73% of teeth overall (22 of 30).25Alagl A, Bedi S, Hassan K, AlHumaid J. Use of platelet-rich plasma for regeneration in non-vital immature permanent teeth: Clinical and cone-beam computed tomography evaluation. J Int Med Res 2017;45(2):583-93. The mean root length increase was 1.06 mm and 0.5 mm, respectively, for PRP and blood clots (p=0.004).25Alagl A, Bedi S, Hassan K, AlHumaid J. Use of platelet-rich plasma for regeneration in non-vital immature permanent teeth: Clinical and cone-beam computed tomography evaluation. J Int Med Res 2017;45(2):583-93. In a second study, apical closure, continued root development and periapical healing were similar for PRP- and blood clot-induced revascularization.26Jadhav G, Shah N, Logani A. Revascularization with and without platelet-rich plasma in nonvital, immature, anterior teeth: a pilot clinical study. J Endod 2012;38(12):1581-7. A decellularized human dental pulp preparation has been studied as a biological scaffold and was able to support dental pulp stem cell viability and attachment.27Matoug-Elwerfelli M, Duggal MS, Nazzal H, Esteves F, Raif E. A biocompatible decellularized pulp scaffold for regenerative endodontics. Int Endod J 2017. Enamel matrix derivative, a protein extract derived from porcine tissue and having been shown to induce formation of cementum in periodontal defects, is also being investigated.28Wang HH, Sarmast ND, Shadmehr E, Angelov N, Shabahang S, Torabinejad M. Application of enamel matrix derivative (Emdogain) in endodontic therapy: A comprehensive literature review. J Endod 2018.
Conclusions
New approaches to regenerative endodontics continue to be evaluated. Future research into specific signalling molecules that could promote pulpal regeneration has been recommended, as well as the development of improved scaffolds.13Nazzal H, Duggal MS. Regenerative endodontics: a true paradigm shift or a bandwagon about to be derailed? Eur Arch Paediatr Dent 2017;18(1):3-15. Further, the application of regenerative endodontics to non-vital mature adult teeth represents a future goal of regenerative endodontics.29He L, Kim SG, Gong Q, Zhong J, Wang S, Zhou X, Ye L, Ling J, Mao JJ. Regenerative endodontics for adult patients. J Endod 2017;43(9S):S57-64.
Current guidelines provide considerations for successful clinical outcomes.23Lee JY, Kersten DD, Mines P, Beltran TA. Regenerative endodontic procedures among endodontists: A web-based survey. J Endod 2018;44(2):250-5. However, they are largely based on case reports and an evidence base to support a specific protocol is lacking.7Singh RK, Shakya VK, Khanna R, Singh BP, Jindal G, Kirubakaran R, Sequeira-Byron P. Interventions for managing immature permanent teeth with necrotic pulps. Cochrane Database Syst Rev 2017;CD012709.,11American Academy of Endodontists. Clinical Considerations for a Regenerative Procedure, Revised 6-8-16. Available at: https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/currentregenerativeendodonticconsiderations.pdf,12Kahler B, Rossi-Fedele G, Chugal N, Lin LM. An evidence-based review of the efficacy of treatment approaches for immature permanent teeth with pulp necrosis. J Endod 2017;43(7):1052-7.,23Lee JY, Kersten DD, Mines P, Beltran TA. Regenerative endodontic procedures among endodontists: A web-based survey. J Endod 2018;44(2):250-5. In addition, there is significant heterogeneity in the approach to regenerative endodontics, and 40% of endododontists in one survey indicated the need for better evidence for RET.12Kahler B, Rossi-Fedele G, Chugal N, Lin LM. An evidence-based review of the efficacy of treatment approaches for immature permanent teeth with pulp necrosis. J Endod 2017;43(7):1052-7.,23Lee JY, Kersten DD, Mines P, Beltran TA. Regenerative endodontic procedures among endodontists: A web-based survey. J Endod 2018;44(2):250-5. Robust randomized controlled clinical trials have been recommended and would provide data on outcomes for the development of an evidence-based protocol to optimize treatment outcomes.
References
- 1.Alley BS, Kitchens GG, Alley LW, Eleazer PD. A comparison of survival of teeth following endodontic treatment performed by general dentists or specialists. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 2004;98(1):115-8.
- 2.He L, Zhong J, Gong Q, Kim SG, Zeichner SJ, Xiang L, Ye L, Zhou X, Zheng J, Liu Y, Guan C, Cheng B, Ling J, Mao JJ. Treatment of necrotic teeth by apical revascularization: Meta-analysis. Sci Reports 2017;7:13941.
- 3.Plascencia H, Díaz M, Moldauer BI, Uribe M, Skidmor E. Non-surgical endodontic management of Type II dens invaginatus with closed and open apex. Iran Endod J 2017;12(4):534-9.
- 4.Garcia-Godoy F, Murray PE. Recommendations for using regenerative endodontic procedures in permanent immature traumatized teeth. Dent Traumatol 2012;28:33-41.
- 5.Silveira CMM, Sebrão CCN, Vilanova LSR, Sanchez-Ayala A. Apexification of an immature permanent incisor with the use of calcium hydroxide: 16-year follow-up of a case. Case Rep Dent 2015:984590.
- 6.Lin J, Zeng Q, Wei X, Zhao W, Cui M, Gu J, Lu J, Yang M, Ling J. Regenerative endodontics versus apexification in immature permanent teeth with apical periodontitis: A prospective randomized controlled study. J Endod 2017;43(11):1821-7.
- 7.Singh RK, Shakya VK, Khanna R, Singh BP, Jindal G, Kirubakaran R, Sequeira-Byron P. Interventions for managing immature permanent teeth with necrotic pulps. Cochrane Database Syst Rev 2017;CD012709.
- 8.Cvek M. Prognosis of luxated non-vital maxillary incisors treated with calcium hydroxide and filled with gutta-percha: a retrospective clinical study. Endod Dent Traumatol 1992;8:45-55.
- 9.Thibodeau B, Trope M. Pulp revascularization of a necrotic infected immature permanent tooth: case report and review of the literature. Pediatr Dent 2007;29(1):47-50.
- 10.Lin LM, Kahler B. A review of regenerative endodontics: current protocols and future directions. J Istanb Univ Fac Dent 2017;51(3 Suppl 1):S41-S51.
- 11.American Academy of Endodontists. Clinical Considerations for a Regenerative Procedure, Revised 6-8-16. Available at: https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/currentregenerativeendodonticconsiderations.pdf
- 12.Kahler B, Rossi-Fedele G, Chugal N, Lin LM. An evidence-based review of the efficacy of treatment approaches for immature permanent teeth with pulp necrosis. J Endod 2017;43(7):1052-7.
- 13.Nazzal H, Duggal MS. Regenerative endodontics: a true paradigm shift or a bandwagon about to be derailed? Eur Arch Paediatr Dent 2017;18(1):3-15.
- 14.Kahler B, Chugal N, Lin LM. Alkaline materials and regenerative endodontics: A review. Materials 2017;10:1389.
- 15.Trevino EG, Patwardhan AN, Henry MA, Perry G, Dybdal-Hargreaves N, Hargreaves KM, Diogenes A. Effect of irrigants on the survival of human stem cells of the apical papilla in a platelet-rich plasma scaffold in human root tips. J Endod 2011;37(8):1109-15.
- 16.Saoud TMA, Ricucci D, Lin LM, Gaengler P. Regeneration and repair in endodontics. A special issue of the regenerative endodontics - a new era in clinical endodontics. Dent J (Basel) 2016;4(1).
- 17.Jeeruphan T, Jantarat J, Yanpiset K, Suwannapan L, Khewsawai P, Hargreaves KM. Mahidol study 1: comparison of radiographic and survival outcomes of immature teeth treated with either regenerative endodontic or apexification methods: a retrospective study. J Endod 2012 Oct;38(10):1330-6.
- 18.Torabinejad M, Nosrat A, Verma P, Udochukwu O. Regenerative endodontic treatment or mineral trioxide aggregate apical plug in teeth with necrotic pulps and open apices: a systematic review and meta-analysis. J Endod 2017;43(11):1806-20.
- 19.López C, Mendoza A, Solano B, Yáñez-Vico R. Revascularization in immature permanent teeth with necrotic pulp and apical pathology: case series. Case Reports Dent 2017; Article ID 3540159.
- 20.Kahler B, Rossi-Fedele G. A review of tooth discoloration after regenerative endodontic therapy. J Endod 2016;42(4):563-9.
- 21.Santos LG, Felippe WT, Souza BD, Konrath AC, Cordeiro MM, Felippe MC. Crown discoloration promoted by materials used in regenerative endodontic procedures and effect of dental bleaching: spectrophotometric analysis. J Appl Oral Sci 2017;25(2):234-42.
- 22.Moodley DS, Peck C, Moodley T, Patel N. Management of necrotic pulp of immature permanent incisor tooth: A regenerative endodontic treatment protocol: case report. S Afr Dent J 2017;72(3):122-5.
- 23.Lee JY, Kersten DD, Mines P, Beltran TA. Regenerative endodontic procedures among endodontists: A web-based survey. J Endod 2018;44(2):250-5.
- 24.Yang H, Shi L, Chen H, Yin Z, Li P. Clinical efficacy of platelet rich fibrin in tooth pulp revascularization in treating periapical periodontitis of immature permanent teeth. J Biosci Med 2016;6.
- 25.Alagl A, Bedi S, Hassan K, AlHumaid J. Use of platelet-rich plasma for regeneration in non-vital immature permanent teeth: Clinical and cone-beam computed tomography evaluation. J Int Med Res 2017;45(2):583-93.
- 26.Jadhav G, Shah N, Logani A. Revascularization with and without platelet-rich plasma in nonvital, immature, anterior teeth: a pilot clinical study. J Endod 2012;38(12):1581-7.
- 27.Matoug-Elwerfelli M, Duggal MS, Nazzal H, Esteves F, Raif E. A biocompatible decellularized pulp scaffold for regenerative endodontics. Int Endod J 2017.
- 28.Wang HH, Sarmast ND, Shadmehr E, Angelov N, Shabahang S, Torabinejad M. Application of enamel matrix derivative (Emdogain) in endodontic therapy: A comprehensive literature review. J Endod 2018.
- 29.He L, Kim SG, Gong Q, Zhong J, Wang S, Zhou X, Ye L, Ling J, Mao JJ. Regenerative endodontics for adult patients. J Endod 2017;43(9S):S57-64.




