Tooth Retention vs. Tooth Extraction and Implant Placement: Clinical Dilemma or Expanding Clinical Options?
Options for replacement of lost teeth dramatically expanded with the introduction and continuing clinical refinement of dental implantology. Osseointegrated dental implants have increased the options available to dental providers to restore the dentition and offer improved clinical solutions for the most complex dental problems. The popularity of these treatments has grown steadily in the past few decades. Nevertheless, when the treatment plan for a compromised tooth or a compromised dentition is under development, the question of retention of one or more teeth with appropriate dental care, that is with necessary periodontal, restorative and endodontic treatment, versus extraction and implant placement, has become and remains a matter of considerable debate. This essay will examine this question from the perspective of that binary choice. Specific periodontal, implant and endodontic procedures, and variations in the range of clinical options for each discipline, will not be addressed as that topic is beyond the scope of this essay.
The introduction of dental implants has changed the landscape of dental care. The modern era of dental implantology began in 1965, with the use of titanium implants to replace lost teeth1Addy LD. An introduction to dental implants. Br Dent J. 2024;236(10):753-7.. The discovery of the unusual property of a biological compatibility of titanium with bone was a serendipitous finding from experiments conducted by P.I. Branemark, who was examining blood flow in the femur of rabbits. He observed that the titanium chambers inserted into rabbit bones could not be removed. An early longitudinal clinical study of the outcome of implant placement revealed 81% (maxilla) to 91% (mandible) success over 15 years2Adell R, Lekholm U, Rockler B, Branemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10(6):387-416.. Therefore, even at this early stage of the dental implant era, one could anticipate the dilemma that faced clinicians.
What does the data say?
Many studies have examined the success rate of dental implants compared to treatment with the goal of tooth retention. The best way to attempt to answer this question is by examining reviews that summarize published studies. There are inherent challenges when attempting this analysis or comparing success rates of two approaches. Are equivalent clinical situations being compared?
A review published in an implant journal in 2007 included 55 studies of single tooth implant survival and 13 studies of teeth that were endodontically treated and restored. They found no significant differences in survival. The conclusion was that “…the decision to treat a tooth endodontically or replace it with an implant must be based on factors other than the treatment outcomes of the procedures themselves.” This is an important statement and indicates the need for an approach to treatment planning that individualizes each situation3Iqbal MK, Kim S. For teeth requiring endodontic treatment, what are the differences in outcomes of restored endodontically treated teeth compared to implant-supported restorations? Int J Oral Maxillofac Implants. 2007;22 Suppl:96-116..
A review of this same issue was published in 20144Setzer FC, Kim S. Comparison of long-term survival of implants and endodontically treated teeth. J Dent Res. 2014;93(1):19-26.. The authors noted the challenges of this comparison, including what is meant by a successful outcome. In endodontics, success has long been defined as the resolution of apical periodontics and an absence of any symptoms. The issue is more complicated for implants. “Success” is not well defined. A definition put forth in 2010 by the Academy of Osteointegration focuses on achieving the desired clinical goal, with the implant in function, stable and esthetically acceptable. Other definitions have been proposed, but these authors noted that criteria for success vary widely. They state that “…it is difficult, if not prohibitive, to compare endodontic outcome studies with strictly defined success criteria with implant outcomes data based on survival. If a positive outcome for teeth was defined as retention without symptoms, regardless of the periapical status, the survival of endodontically treated teeth is as high as that of implants.” They suggest that survival is the best basis for comparison.
A systemic review and meta-analysis published in 2021 included 5 studies. Conclusions were that both therapies were considered to be effective treatment approaches. There were no significant differences when considering survival as the outcome. However, when other criteria were used, endodontic therapy had somewhat better results5Sayed ME, Jurado CA, Tsujimoto A, Garcia-Cortes JO. Clinical decision-making regarding endodontic therapy vs extraction and implant-assisted replacement: a systematic review and meta-analysis. Gen Dent. 2021;69(1):52-7..
Examining studies of patients who had a history of periodontitis, outcomes of endodontic therapy and implant placement were compared in a systematic review6Sarafidou K, Lazaridi I, Gotsis S, Kirmanidou Y, Vasilaki D, Hirayama H, et al. Tooth preservation vs. extraction and implant placement in periodontally compromised patients: A systematic review and analysis of studies. J Prosthodont. 2022;31(8):e87-e99.. Twenty-four studies were included. The implant treated group included extraction of periodontally-involved teeth and implant placement. Patients in the tooth retention group received periodontal treatment, both with and without regenerative procedures. Percent survival was high in both groups (81-100% tooth retention, 95-100% implants). Frequency of complications was 13% in the tooth retention group and 24% in the implant group. The authors considered the two groups comparable in terms of the outcome. Both the use of regenerative procedures and adherence to a strict maintenance schedule improved the prognosis of the teeth affected by periodontitis. Their suggestion was that periodontal treatment should first be attempted before tooth removal and implant placement6Sarafidou K, Lazaridi I, Gotsis S, Kirmanidou Y, Vasilaki D, Hirayama H, et al. Tooth preservation vs. extraction and implant placement in periodontally compromised patients: A systematic review and analysis of studies. J Prosthodont. 2022;31(8):e87-e99..
A critical review of the choice between endodontic therapy and tooth retention vs. extraction and implant placement concluded that when making a choice, key concerns were:
- The condition of the tooth in question, considering variables such as the remaining tooth structure, percent loss of attachment, and tooth mobility.
- The potential influence of the patient’s health, specifically medical diagnoses.
- The patient’s preference.
As above, they also concluded that tooth retention should be the first choice7Sartoretto SC, Shibli JA, Javid K, Cotrim K, Canabarro A, Louro RS, et al. Comparing the Long-Term Success Rates of Tooth Preservation and Dental Implants: A Critical Review. J Funct Biomater. 2023;14(3)..
Decision Analysis:
Decision analysis is the process by which a decision is reached considered all the variables that can influence the outcome. Formal and informal attempts at developing an approach to decision-making have been published and emphasize the many variables that need to be considered when deciding on the best clinical approach.
Avila and colleagues8Avila G, Galindo-Moreno P, Soehren S, Misch CE, Morelli T, Wang HL. A novel decision-making process for tooth retention or extraction. J Periodontol. 2009;80(3):476-91. developed a complex decision chart to help guide the clinician. There are 6 levels, with sub-categories within each:
- Initial assessment: patient expectations, treatment expectations, esthetics, finances, patient compliance.
- Severity of periodontal disease: probing depths, mobility, recurrent abscesses, bone loss, osseous defect morphology.
- Furcation involvement: class, interproximal bone level, root anomalies, root resection.
- Etiologic factors: presence of calculous, surgical compromise, periodontal retreatment, root proximity, endodontic therapy.
- Restorative factors: faulty restorations/fractures, extensive caries, crown to root ratio, the need for a post and core.
- Other determinants: smoking, systemic diseases, use of bisphosphonates, skill of the clinician.
To guide the clinician, a color-coded grading (green = favorable progress, yellow = cautious, red = unfavorable) was suggested. Such a comprehensive approach is intensive but emphasizes the potential complexity of the treatment planning process.
The decision analysis proposed by Avila et. al.8Avila G, Galindo-Moreno P, Soehren S, Misch CE, Morelli T, Wang HL. A novel decision-making process for tooth retention or extraction. J Periodontol. 2009;80(3):476-91. has been considered by other authors. Nunn et. al.9Nunn ME, Fan J, Su X, Levine RA, Lee HJ, McGuire MK. Development of prognostic indicators using classification and regression trees for survival. Periodontol 2000. 2012;58(1):134-42. suggested the use of new statistical approaches to identify the interrelationship of different variables deemed to be important in determining tooth prognosis. Carcano-Espana et. al.10Carcamo-Espana V, Cuesta Reyes N, Flores Saldivar P, Chimenos-Kustner E, Estrugo Devesa A, Lopez-Lopez J. Compromised Teeth Preserve or Extract: A Review of the Literature. J Clin Med. 2022;11(18). made some modifications to be the scheme presented by Avila et. al.8Avila G, Galindo-Moreno P, Soehren S, Misch CE, Morelli T, Wang HL. A novel decision-making process for tooth retention or extraction. J Periodontol. 2009;80(3):476-91., with a focus on the severity of periodontal destruction and whether the tooth or teeth in question can be restored. They highlighted the importance of maintaining natural teeth, as the presence of a periodontal ligament provides proprioception, and allows adaptation to the stress associated with function. The basic concept introduced by Avila et. al.8Avila G, Galindo-Moreno P, Soehren S, Misch CE, Morelli T, Wang HL. A novel decision-making process for tooth retention or extraction. J Periodontol. 2009;80(3):476-91. can be re-considered with the variables classified into 4 domains: clinical patient variables, restorative considerations, systemic variables and personal/socioeconomic variables (see Figure 1).
A similar approach, that being creation of a decision tree, has been published by others11Ovaydi-Mandel A, Petrov SD, Drew HJ. Novel decision tree algorithms for the treatment planning of compromised teeth. Quintessence Int. 2013;44(1):75-84.. The authors emphasize the need for such algorithms to be based on the published, peer-reviewed literature, and should be updated as new information becomes available.
Clarke and Levin12Clark D, Levin L. In the Dental Implant Era, Why Do We Still Bother Saving Teeth? J Endod. 2019;45(12S):S57-S65. asked a provocative question: “In the Dental Implant Era, Why Do We Still Bother Saving Teeth?” They argue that implant success rate is not 100%, and that complications do occur (peri-implant mucositis, peri-implantitis). The full range of treatment options must be considered. They emphasize that regardless of the selected approach, a maintenance recall schedule must be maintained. They also remind us that treatment must be ethical and based on the best available evidence.
Economic Considerations:
A person’s financial status is often a primary determinant of the selection of an approach to treatment. This includes both insurance support (private or public) as well as the individual’s willingness to pay out-of-pocket for dental services, specifically what is not covered by insurance. Of note, access to dental care has been closely linked to having dental insurance13Manski RJ, Goodman HS, Reid BC, Macek MD. Dental insurance visits and expenditures among older adults. Am J Public Health. 2004;94(5):759-64.14Gnanamanickam ES, Teusner DN, Arrow PG, Brennan DS. Dental insurance, service use and health outcomes in Australia: a systematic review. Aust Dent J. 2018;63(1):4-13.. Nevertheless, dental insurance generally limits coverage to a set amount that is renewed each year. The cost of comprehensive dental care can easily exceed the coverage provided by employer-provided dental insurance.
Willingness-to-pay studies provide a measure of a patient’s interest in proceeding with dental treatment if out-of-pocket payment is required. In one study, individuals responded to different scenarios that assessed their preference for retaining teeth with a questionable prognosis, versus extraction and replacement with an implant. Two-thirds of respondents preferred to retain their teeth, and the amount they were willing to pay was 4 times greater as compared to the cost of extraction without tooth replacement. Not surprisingly, the willingness to pay was greater for anterior vs. posterior teeth. Patient variables associated with a willingness to pay a greater amount included greater education, employment, older age, preferring care in a private office setting and being female15Ghahramani S, Ziar N, Moradi N, Bagheri Lankarani K, Sayari M. Preserving natural teeth versus extracting them: a willingness to pay analysis. BMC Oral Health. 2022;22(1):375..
In a larger study of 762 individuals, questions were asked about crown restorations, representing a costly treatment choice. The most important variables were esthetics and expected durability of the restoration. In this cohort, respondents were from a developed country (Germany) and were willing to pay more for what was considered improved treatment16Felgner S, Henschke C. Patients' preferences in dental care: A discrete-choice experiment and an analysis of willingness-to-pay. PLoS One. 2023;18(2):e0280441.. The authors suggested that their findings can help when attempting to determine an appropriate treatment approach for different patients.
It is challenging to compare the cost of tooth retention and treatment and tooth removal and placement of an implant and the required restoration. Fees differ in different parts of the country, and there are differences between urban, suburban and rural locales. In an attempt to compare the cost of these two approaches to care, the Delta Dental Cost Estimator was used to gauge the cost of treatment for a single tooth17Dental Dental Plans Association. Delta Dental Cost Estimator. https://deltadental.com/us/en/member/cost-estimator.html.. For tooth retention, specific procedures included:
- Periodontal treatment (root planning and sealing, periodontal surgery)
- Restoration (crown)
- Endodontic treatment (with and without treatment of an anterior tooth, or molar tooth)
What was not considered is the need for a bone graft during periodontal surgery, as well as the need for a post and core if endodontic treatment was performed. The fee assigned to periodontal surgery was the fee for a gingival graft, which is the only periodontal surgical procedure in the Estimator.
For tooth removal, specific procedures included:
- Extraction (surgical)
- Implant (includes surgical implant placement, the abutment and crown)
The need for a bone graft during implant placement was not considered. Further, the fee for an evaluation and any imaging was not factored in the calculations, as most patients would require imaging. Lastly, as the Estimator provides a cost range for each procedure at each location, and the midpoint was considered the cost for all procedures. The cost for follow-up maintenance visits was also not included, as this would apply in both clinical scenarios. Three locations in the United States were included.
This data is provided in Table 1. In the absence of the need for endodontic treatment the trend was for the cost of tooth retention being lower than for implant placement. The reverse was true when endodontic treatment was required for a molar tooth. Nevertheless, these differences were not great, generally less than 25%.
Other Considerations:
Tooth retention has been linked to successful aging. As an example, Musacchio and colleagues18Musacchio E, Binotto P, Perissinotto E, Sergi G, Zambon S, Corti MC, et al. Tooth retention predicts good physical performance in older adults. PLoS One. 2021;16(9):e0255741. observed a strong correlation between having at least 20 teeth and less disability. Conversely, having fewer teeth is associated with greater health challenges as people age. Cause and effect cannot be evaluated, as aging is a natural but complex process that involves many intrinsic and extrinsic variables. Nevertheless, the authors emphasize the “good oral status is a crucial component of successful aging.”
Further, studies have linked fewer teeth to a risk for developing dementia19Yoo JJ, Yoon JH, Kang MJ, Kim M, Oh N. The effect of missing teeth on dementia in older people: a nationwide population-based cohort study in South Korea. BMC Oral Health. 2019;19(1):61.. There are many studies that have observed this relationship 20Galindo-Moreno P, Lopez-Chaichio L, Padial-Molina M, Avila-Ortiz G, O'Valle F, Ravida A, et al. The impact of tooth loss on cognitive function. Clin Oral Investig. 2022;26(4):3493-500.,21Li L, Zhang Q, Yang D, Yang S, Zhao Y, Jiang M, et al. Tooth loss and the risk of cognitive decline and dementia: A meta-analysis of cohort studies. Front Neurol. 2023;14:1103052.. What is noteworthy about the Yoo et. al. study19Yoo JJ, Yoon JH, Kang MJ, Kim M, Oh N. The effect of missing teeth on dementia in older people: a nationwide population-based cohort study in South Korea. BMC Oral Health. 2019;19(1):61. was that the data analyzed was from a longitudinal study of older adults in South Korea and included more than 200,000 individuals. They concluded that “…it is important to delay tooth loss and preserve the stable remaining teeth to help prevent dementia.” These studies do not consider the effect of replacement of lost teeth by implants or fixed prostheses.
Conclusions:
This review has stressed the need to consider a large number of variables when deciding on a treatment plan for a tooth with a questionable prognosis. These variables must be analyzed before any advice is given and a treatment plan is developed. The studies reviewed here suggest that comparison between outcomes of traditional dental treatment of a compromised tooth and extraction and implant placement is not valid. Rather, these approaches should be viewed as different options, with the selection of the best approach for long term success. In addition to the many clinical variables, it is important to emphasize that patient variables must be considered. These include patient desire (i.e., attitude about retaining the natural dentition, dental health literacy). There is relatively little difference in the cost of these approaches when a single tooth is being treated (see Table 1). Though not considered here, the financial variable assumes greater importance when multiple teeth are considered, or in the case of near total or total edentulism. The cost of a traditional complete denture versus a tooth supported overdenture, or placement of multiple implants in one or both jaws varies dramatically, but the basic decision-making principles outlined here still apply.
It is the provider’s responsibility to do what is in the patient’s best interest. Stories in the lay press have suggested some inappropriate approaches to dental care that favor the extraction of teeth that can be treated and retained, followed by implant placement22Kelman B. and Werner A. Dentists are pulling healthy and treatable teeth to profit from implants, experts warn. CBS News Health Watch, October 31, 2024.. The practitioner should present the patient with options, educate them when necessary and answer all questions. This can help ensure a satisfactory clinical and personal result.
| New York City area | Dubuque, Iowa area | San Antonio, Texas area | |
|---|---|---|---|
| Tooth Retention | |||
| Periodontal | 3235 | 2123 | 2426 |
| Restorations | 1893 | 1367 | 1942 |
| Endodontic tx | |||
| Anterior | 1425 | 1024 | 942 |
| Molar | 1835 | 1350 | 2009 |
| No endodontic tx | 5128 | 3490 | 4368 |
| With endodontic tx | |||
| Anterior | 6553 | 4514 | 5310 |
| Posterior | 6963 | 4840 | 6377 |
| Implant Placement | |||
| Extraction | 563 | 383 | 488 |
| Implant | 4368 | 4213 | 5221 |
| Total | 4931 | 4596 | 5709 |
| % Differences | |||
| Retention vs. implant | -4% | +24% | +24% |
| Anterior endodontic tx | +28% | -2% | +7% |
| Molar endodontic tx | +36% | +5% | +12% |
Table 1. Comparison of the cost of tooth retention vs. extraction and implant placement for a single tooth. Three locations are considered, and cost is provided for anterior and posterior teeth. The data was based on fees in the Delta Dental Cost Estimator (17).
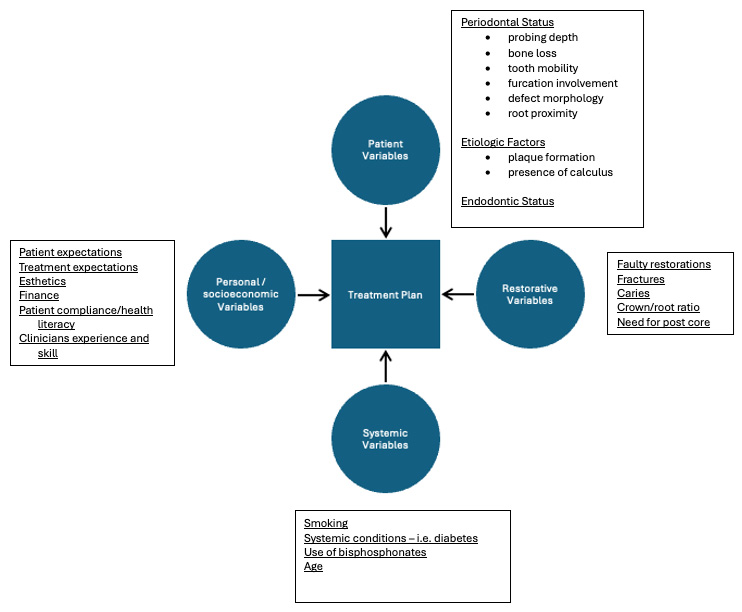
Figure 1. Variables to be considered when deciding upon tooth retention and treatment vs. tooth extraction and implant placement. The variables are grouped into 4 domains. Adapted from Avila et.al. (8).
References
- 1.Addy LD. An introduction to dental implants. Br Dent J. 2024;236(10):753-7.
- 2.Adell R, Lekholm U, Rockler B, Branemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10(6):387-416.
- 3.Iqbal MK, Kim S. For teeth requiring endodontic treatment, what are the differences in outcomes of restored endodontically treated teeth compared to implant-supported restorations? Int J Oral Maxillofac Implants. 2007;22 Suppl:96-116.
- 4.Setzer FC, Kim S. Comparison of long-term survival of implants and endodontically treated teeth. J Dent Res. 2014;93(1):19-26.
- 5.Sayed ME, Jurado CA, Tsujimoto A, Garcia-Cortes JO. Clinical decision-making regarding endodontic therapy vs extraction and implant-assisted replacement: a systematic review and meta-analysis. Gen Dent. 2021;69(1):52-7.
- 6.Sarafidou K, Lazaridi I, Gotsis S, Kirmanidou Y, Vasilaki D, Hirayama H, et al. Tooth preservation vs. extraction and implant placement in periodontally compromised patients: A systematic review and analysis of studies. J Prosthodont. 2022;31(8):e87-e99.
- 7.Sartoretto SC, Shibli JA, Javid K, Cotrim K, Canabarro A, Louro RS, et al. Comparing the Long-Term Success Rates of Tooth Preservation and Dental Implants: A Critical Review. J Funct Biomater. 2023;14(3).
- 8.Avila G, Galindo-Moreno P, Soehren S, Misch CE, Morelli T, Wang HL. A novel decision-making process for tooth retention or extraction. J Periodontol. 2009;80(3):476-91.
- 9.Nunn ME, Fan J, Su X, Levine RA, Lee HJ, McGuire MK. Development of prognostic indicators using classification and regression trees for survival. Periodontol 2000. 2012;58(1):134-42.
- 10.Carcamo-Espana V, Cuesta Reyes N, Flores Saldivar P, Chimenos-Kustner E, Estrugo Devesa A, Lopez-Lopez J. Compromised Teeth Preserve or Extract: A Review of the Literature. J Clin Med. 2022;11(18).
- 11.Ovaydi-Mandel A, Petrov SD, Drew HJ. Novel decision tree algorithms for the treatment planning of compromised teeth. Quintessence Int. 2013;44(1):75-84.
- 12.Clark D, Levin L. In the Dental Implant Era, Why Do We Still Bother Saving Teeth? J Endod. 2019;45(12S):S57-S65.
- 13.Manski RJ, Goodman HS, Reid BC, Macek MD. Dental insurance visits and expenditures among older adults. Am J Public Health. 2004;94(5):759-64.
- 14.Gnanamanickam ES, Teusner DN, Arrow PG, Brennan DS. Dental insurance, service use and health outcomes in Australia: a systematic review. Aust Dent J. 2018;63(1):4-13.
- 15.Ghahramani S, Ziar N, Moradi N, Bagheri Lankarani K, Sayari M. Preserving natural teeth versus extracting them: a willingness to pay analysis. BMC Oral Health. 2022;22(1):375.
- 16.Felgner S, Henschke C. Patients' preferences in dental care: A discrete-choice experiment and an analysis of willingness-to-pay. PLoS One. 2023;18(2):e0280441.
- 17.Dental Dental Plans Association. Delta Dental Cost Estimator. https://deltadental.com/us/en/member/cost-estimator.html.
- 18.Musacchio E, Binotto P, Perissinotto E, Sergi G, Zambon S, Corti MC, et al. Tooth retention predicts good physical performance in older adults. PLoS One. 2021;16(9):e0255741.
- 19.Yoo JJ, Yoon JH, Kang MJ, Kim M, Oh N. The effect of missing teeth on dementia in older people: a nationwide population-based cohort study in South Korea. BMC Oral Health. 2019;19(1):61.
- 20.Galindo-Moreno P, Lopez-Chaichio L, Padial-Molina M, Avila-Ortiz G, O'Valle F, Ravida A, et al. The impact of tooth loss on cognitive function. Clin Oral Investig. 2022;26(4):3493-500.
- 21.Li L, Zhang Q, Yang D, Yang S, Zhao Y, Jiang M, et al. Tooth loss and the risk of cognitive decline and dementia: A meta-analysis of cohort studies. Front Neurol. 2023;14:1103052.
- 22.Kelman B. and Werner A. Dentists are pulling healthy and treatable teeth to profit from implants, experts warn. CBS News Health Watch, October 31, 2024.



