Background
Dental caries (tooth decay) is the most chronic disease among children1US Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Rockville, MD; 2000.. Children suffering from oral health problems experience serious social and health issues such as chronic pain, problems with eating and speaking, inability to concentrate in school, reduced social and family interaction, and diminished self-image and self-esteem1US Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Rockville, MD; 2000.. Dental disease is one of the leading causes of school absenteeism for children, and more than 51 million school hours are lost each year due to dental-related illness1US Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General. Rockville, MD; 2000..
About 80% of dental caries is concentrated in 20-25% of children, primarily those from low-income and/ or minority backgrounds2J. Liu, J.C Probst, A.B. Martin, J-Y. Wang, and C.F. Salinas, “Disparities in dental insurance coverage and dental care among US children: the national survey of children’s health” Pediatrics, vol. 119, no. 1, pp. S12-S21, 2007.. Nationally, Hispanic children have the lowest rates in dental care utilization3W. E. Mouradian, E. Wehr, J.J. Crall. “Disparities in children’s oral health and access to dental care” JAMA. 2000; 284:2625-2631. Ironically, those at highest risk are also those who face the greatest barriers to accessing early and ongoing dental care4B.L. Edelstein and C.H. Chinn, “ Update on disparities in oral health and access to dental care for America’s children”, Academic pediatrics, vol 9, no 6, pp.415-419, 2009..
Several studies have identified factors that hindered these children in obtaining dental care which include: socioeconomic level, ethnicity, primary language, education level of their parents or caregivers, lack of transportation, lack of work/school permission, lack of insurance coverage and social and cultural barriers.
The traditional private practice dental workforce model does not successfully reach every child that is in need of dental care5Y. Liu, R. Carpino, M. Walker, “Assessing the Effectiveness of a School-based dental clinic on the oral health of children who lack access to dental care: A program evaluation” Journal of School of Nursing, 2016. An important Oral Health Objective from the Healthy People 2020 report is to increase the percentage of school based health centers with an oral health component that includes dental care. The establishment of school-based dental health clinics has proven to be a unique and effective way to address the barriers to accessing oral health care for high-risk, low-income pediatric patient populations. Depending on the program, school-based dental clinics can provide everything from basic, preventive care to fully comprehensive, restorative treatment right inside the walls of the child’s school. Parents are able to sign a consent form prior to the appointment, and therefore are not required to be present during the time of the visit. School-based programs can have a tremendous impact on access to care because they overcome both monetary and social barriers5Y. Liu, R. Carpino, M. Walker, “Assessing the Effectiveness of a School-based dental clinic on the oral health of children who lack access to dental care: A program evaluation” Journal of School of Nursing, 2016.
P.S. 188, known as the Island School, spans pre-kindergarten through eighth grade. It is located on the Lower East Side of Manhattan. At P.S.188, 47 percent of their students are homeless. Nearly all of the 500 students at PS188 are poor. The school is surrounded on all sides by a fortress of public housing. Most of its students come from these housing projects, as well as from four homeless shelters in the area6E. Harris. “Where Nearly Half of Pupils are Homeless, School Aims to be Teacher, Therapist, Even Santa”. The New York Times June 6th 2016.. P.S 188 is one of the five NYC Public Schools that the “Bringing Smiles” School Based Dental Program provides pediatric dental services through the establishment and operation of portable dental clinics.
Purpose
The purpose of this report is to address oral health care issues and seek strategies for prevention and comprehensive dental care in children of hispanic descent.
Literature Review
Clinical Question
How do school-based dental programs eliminate the barriers to dental care for hispanic pediatric dental populations?
P: Hispanic Pediatric Patients
I: Hispanic Pediatric Patients in a School Based Setting
C: Hispanic Pediatric Patients not in a School Based setting
O: Lowering the ECC risk in Hispanic Pediatric Patient population
The article we selected is titled: Update on Disparities in Oral Health and Access to Dental Care for America’s Children by Edelstein et al. The goal of this contribution is to review and explore subsequent federal data on children’s oral health and dental care since release of Oral Health in America: A Report of the Surgeon General in 2000. The 2002 review found that children disadvantaged by poverty and minority status had greater likelihood of having cavities and, when affected, had more cavities than their peers4B.L. Edelstein and C.H. Chinn, “ Update on disparities in oral health and access to dental care for America’s children”, Academic pediatrics, vol 9, no 6, pp.415-419, 2009.. This subgroup of children had fewer overall and preventive dental visits than did their peers but used dental services more often for relief of pain4B.L. Edelstein and C.H. Chinn, “ Update on disparities in oral health and access to dental care for America’s children”, Academic pediatrics, vol 9, no 6, pp.415-419, 2009.. Since then, child poverty has remained high, especially among minority groups. In fact, there has been an increase in levels of poverty in young US children who are minorities and low income4B.L. Edelstein and C.H. Chinn, “ Update on disparities in oral health and access to dental care for America’s children”, Academic pediatrics, vol 9, no 6, pp.415-419, 2009.. This contribution examines the trends in dental caries among US children. By doing so they have analyzed that children who are affected earliest by childhood caries have the most intense disease experience and remain at substantial risk for ongoing disease progression. The Center for Disease Control and Prevention reported that more than half of two to eleven year old children in poor families experienced higher rates of cavities compared with a third of the children in families with incomes above 200% of the federal poverty level4B.L. Edelstein and C.H. Chinn, “ Update on disparities in oral health and access to dental care for America’s children”, Academic pediatrics, vol 9, no 6, pp.415-419, 2009.. The disparities in pediatric caries experience by race and ethnicity remain unchanged and among the US Hispanic population. Mexican American children experience higher rates of primary dentition caries (55%) compared to black children (43%) or white children (39%)4B.L. Edelstein and C.H. Chinn, “ Update on disparities in oral health and access to dental care for America’s children”, Academic pediatrics, vol 9, no 6, pp.415-419, 2009.. Similar rates are evident when discussing untreated tooth decay and permanent tooth decay in low-income hispanic children in the US. The authors of this update also mention the trends in dental service utilization among US children. One third of minority children obtain dental care in a year compared with half of white children4B.L. Edelstein and C.H. Chinn, “ Update on disparities in oral health and access to dental care for America’s children”, Academic pediatrics, vol 9, no 6, pp.415-419, 2009.. Children whose parents obtained less than high school education were less than half as likely to obtain a dental visit in 2004 in comparison to children whose parents are college graduates (25% vs 54%)4B.L. Edelstein and C.H. Chinn, “ Update on disparities in oral health and access to dental care for America’s children”, Academic pediatrics, vol 9, no 6, pp.415-419, 2009.. On another note, since the advent of the State Children’s Health Insurance Program (SCHIP), which served to expand coverage, access and utilization of dental services for the pediatric community, the percentage of children covered by public insurance who receive a dental visit has increased4B.L. Edelstein and C.H. Chinn, “ Update on disparities in oral health and access to dental care for America’s children”, Academic pediatrics, vol 9, no 6, pp.415-419, 2009.. However, there seems to be other factors that must be further studied due to the profound and ongoing disparities in dental access that are still affecting minority and low-income pediatric populations.
Our patient C.D. is a hispanic pediatric patient who has experienced racial and income-based disparities. She presented with untreated tooth decay to the NYU College of Dentistry and due to the large amounts of visits that her oral health conditions required, she was unable to continue receiving care at the college. Her mother was unable to bring her to the scheduled appointments due to the fact that she was unable to take time off from work. The family recently moved from a shelter home to permanent housing. Patient C.D.’s mother is a single mother who is supporting patient C.D. and her two brothers. Taking time off from work significantly affects her income and her ability to provide for the entire household. The Bringing Smiles School-Based Dental Program has been particularly helpful for patients of low socioeconomic backgrounds who lack access and resources to help them receive the proper dental care. School-based dental programs are establishing equity for minority and low-income populations and tackling the increasing rates of oral disease in these communities by facilitating preventative and efficient dental services.
In the program evaluation by Carpino et al. titled: Assessing the Effectiveness of a School-Based Dental Clinic on the Oral Health of Children Who Lack Access to Dental Care: A Program Evaluation, we learn about how literature has revealed that poor oral health in children can be associated with low self-esteem, inability to concentrate, and the loss of over 51 million school hours5Y. Liu, R. Carpino, M. Walker, “Assessing the Effectiveness of a School-based dental clinic on the oral health of children who lack access to dental care: A program evaluation” Journal of School of Nursing, 2016. Furthermore, the article states that good dental health is a vital part of a child’s development. Recognizing the need for changes in the way that oral health services are accessed, Healthy People 2020 includes an objective to increase the proportion of school-based health centers with an oral health component5Y. Liu, R. Carpino, M. Walker, “Assessing the Effectiveness of a School-based dental clinic on the oral health of children who lack access to dental care: A program evaluation” Journal of School of Nursing, 2016. Poor and underserved children experience cultural, social, economic, structural, and geographic barriers at a much higher rate than their peers with more financial stability when trying to access oral health in a traditional practice setting. Our patient, C.D. is affected by some of these barriers5Y. Liu, R. Carpino, M. Walker, “Assessing the Effectiveness of a School-based dental clinic on the oral health of children who lack access to dental care: A program evaluation” Journal of School of Nursing, 2016. Thanks to the School-Based Dental Program, she has been able to receive the appropriate care. Encounter intensity with a dental or dental hygiene student appears to influence the oral health status of children. This program evaluation used complementary methods of testing effects (MANOVA and Kruskal–Wallis test) and examining associations (Pearson’s correlation) to evaluate the data5Y. Liu, R. Carpino, M. Walker, “Assessing the Effectiveness of a School-based dental clinic on the oral health of children who lack access to dental care: A program evaluation” Journal of School of Nursing, 2016.
This study concluded that the traditional dental workforce model is unable to reach every child needing care. It is essential for dental health care to move forward with an improved system of care delivery5Y. Liu, R. Carpino, M. Walker, “Assessing the Effectiveness of a School-based dental clinic on the oral health of children who lack access to dental care: A program evaluation” Journal of School of Nursing, 2016. By assessing the outcomes of a school-based dental center, this program evaluation was able to assess the quality and provide feedback on whether this is a plausible delivery model that could be implemented in other school-based settings5Y. Liu, R. Carpino, M. Walker, “Assessing the Effectiveness of a School-based dental clinic on the oral health of children who lack access to dental care: A program evaluation” Journal of School of Nursing, 2016. The outcomes from this program evaluation further supports the body of literature that asserts school-based dental clinics show great promise for providing access to high-quality, cost-effective oral health care5Y. Liu, R. Carpino, M. Walker, “Assessing the Effectiveness of a School-based dental clinic on the oral health of children who lack access to dental care: A program evaluation” Journal of School of Nursing, 2016.
Patient Presentation
The subject of this report is an eight year old hispanic female pediatric patient, C.D. She was born in the Dominican Republic. Her family decided to immigrate to the US in 2017. She lives at home with her mother (single mother) and two siblings ( older and younger brother). She recently moved from a shelter home to permanent housing in Brooklyn, NY.
Our patient is currently attending 4th grade at PS188- The Island School.
Chief Complaint:
“My brothers and my friends make fun of my front tooth and my back teeth hurt when I eat”
- The patient specifically stated that she had sensitivity to cold and sometimes pain in her posterior teeth ( both right and left posterior teeth).
Medical History:
Our patient “C.D” has no significant medical history ( as per review of systems “ROS”) *
- No previous surgeries or recent hospitalizations.
- Immunizations are up to date
- Patient is not taking any medications
- No known drug allergies
| System | Review |
|---|---|
| Eyes | WNL – No significant findings |
| Ears, Nose, Mouth and Throat ( ENT) | WNL – No significant findings |
| Cardiovascular | WNL – No significant findings |
| Respiratory | WNL – No significant findings |
| Gastrointestinal | WNL – No significant findings |
| Musculoskeletal | WNL – No significant findings |
| Integumentary | WNL – No significant findings |
| Neurologic/ Psychiatric | WNL – No significant findings |
| Endocrine | WNL – No significant findings |
| Hematology/ Lymphatic | WNL – No significant findings |
| Allergic/ Immunologic | WNL – No significant findings |
| Constitutional Symptoms | None |
Pregnancy and Birth History:
- Full Term( Vaginal Birth)- No complications
Patient Medical Status:
- ASA 1
Family History:
- Negative for Cleft Lip or Palate or any craniofacial anomalies
Social History:
Our patient “C.D” was born in the Dominican Republic and moved to the US when she was five years old.
- Spanish is her primary language.
- She attends the 4th grade at PS-188 The Island School.
- She has two other siblings ( one older brother and one younger brother)
- Patient lives with mother and siblings only.
- Patient doesn’t have previous unpleasant medical/dental experiences.
- Patient used to complain of pain in her mouth – but now, she states that her missing her front tooth is bothering her.
- She doesn’t use any mouthguards- she doesn’t play any sports.
- Patient C.D. does not smoke, drink alcohol, or engage in recreational drug use.
Dental History:
Our patient “C.D” was first seen by a dentist at the age of six at the NYU College of Dentistry – Pediatric Dental Clinic accompanied by her mother (8/10/17).
- A dental treatment plan was created, however, the patient did not return with her mother due to the amount of dental visits needed.
- Mother stated she can not take off work to take her to the dentist and that appointment and that the patient could get penalized for missing school.
- Only a few dentists take her insurance around where she lives, but appointments are not available for the next 5 months – especially on the weekends.
On September 2018, the patient signed up for the School Based Dental Program, “Bringing Smiles”, at her own elementary school.
- Her last dental visit was September 18th, 2019 – for a recall visit.
Family Dental Care History:
Primary caregiver (Mother) and siblings have cavities. Unfortunately, they don’t receive routine dental care.
- Brushing Practice:
Our patient “C.D” states she only brushes her teeth 1x day ( unsupervised) - Flossing Practice:
Our patient states she never flosses her teeth – “ I don’t have floss” - Fluoride History:
Lives in an area with fluoridated tap water, drinks fluoridated tap water and uses fluoride toothpaste - Nutritive Habits/ Non-Nutritive Habits:
None – no trouble swallowing.
Diet:
- Patient drinks apple juice – for breakfast and lunch (food and drinks provided by the PS school).
- Patient has 2 snacks per day – crackers and occasionally, gummy bears.
- Patient drinks water – from time to time.
Clinical Examination
Examination involved evaluation of the head and neck. Palpation to identify enlarged and fixed lymph nodes and other swellings and also the form and function.

Figures 1, 2, & 3: Facial and lateral profiles of Patient C.D.
Extra -Oral Examination:
- Head and Neck Exam: no significant findings – within normal limits (WNL)
- Brodsky Grade: 1
- Temporomandibular joint: symmetry in function, smooth movement, absence of pain, max. Range of motion- WNL
- Lymph nodes: normal size, mobility – NSF (No significant findings)
- Frontal Profile: Symmetrical
- Antero-Posterior Profile: Convex
Intra-oral Examination:
- Palate: normal function,integrity, absence of lesion
- Tongue: normal color, range of motion, absence of lesions
- Floor of the mouth: salivary function, absence of swelling or lesions.
- Buccal mucosa: Absence of lesions or swelling
- Gingival tissues:
Findings:
- Soft Tissues:
- No significant findings, except for lower left posterior side around tooth L and K
- Hard Tissues:
- Non-erupted tooth #8 and missing tooth #T
- Partially Erupted Teeth #6 and #11.
Cavitated lesions on teeth:#3-O #A-OBL,#14-O #19-O,#L-O, #S-O,and #30-OB

Figures 4,5 & 6: Posterior right, anteriors, and posterior left
Occlusal Analysis:
- Midline: N/A due to unerupted #8
- Overjet: 2mm
- Overbite: 70%
- Open Bite: N/A
- Crossbite: none
- Spacing: Slight spacing in both Maxillary and Mandibular arches
- Right Side: Class|Molar Class|Canine
- Left Side: Class|Molar Class|Canine
Pre Tx Diagnostic Models
Figures 7 & 8 diagnostic models from first visit
Radiographs:
Patient presented to NYUCD to visit the dentist for the first time in 2017. These BWs and PAN were taken then.
The dental treatment recommended for this patient in 2017 included:
Comprehensive dental exam, prophylaxis, fluoride, 2 BWs, PAN- performed on 8/10/17
|
|
Date of service: 08/10/17
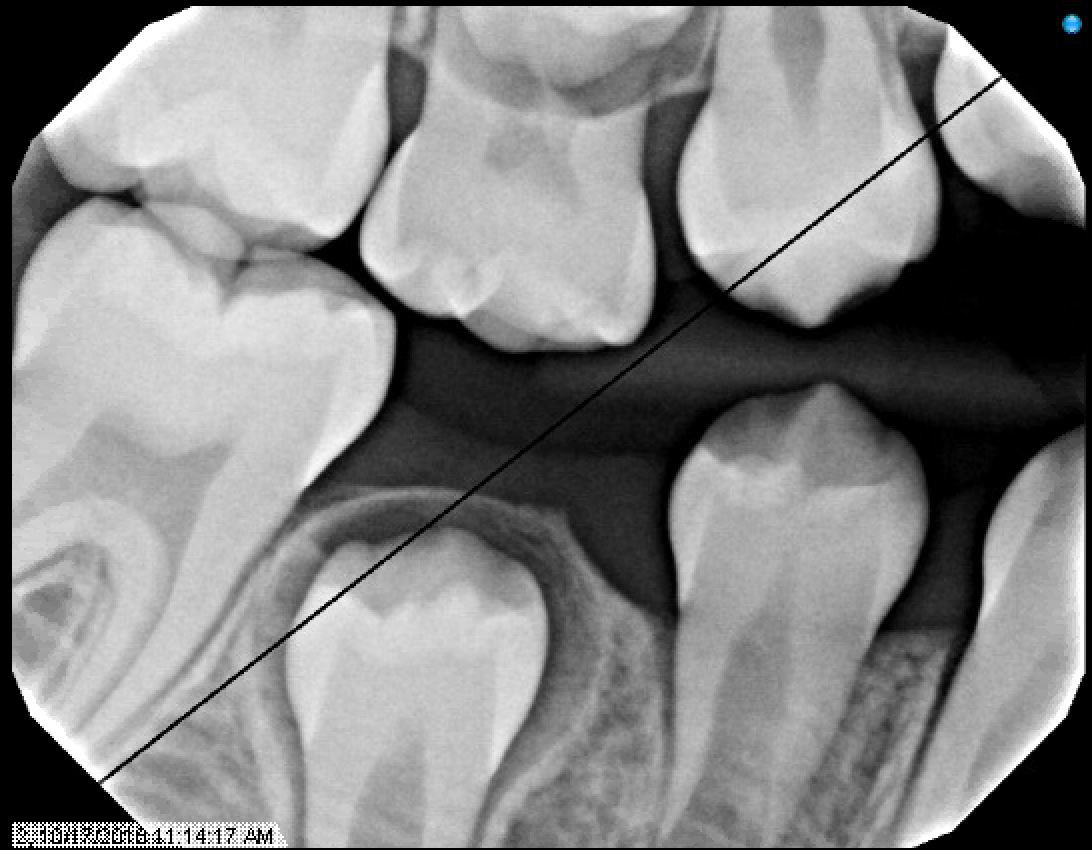
Figures 9 & 10: Preoperative bitewings of Right and Left
Figure 11: Preoperative Panoramic image
Unfortunately, due to the amount of dental treatment needed and number of dental visit needed, patient and mother never returned back to NYU dental clinic.
 |
 |
| UG Clinic – NYUCD 8/10/17 |
School Based Dental Program @PS188 10/17/18 |
- Our Patient “C.D” signed up for the School Based Dental Program @PS188. The Bringing Smiles School Based Program @PS188 started on September 2018.
Comprehensive Pediatric Dental Treatment is provided every week at PS 188 ( Wednesdays). Patients that sign up for the program receive all the pediatric dental services at their school (exam, x-rays, prophy, fluoride, restorations, sealants, extractions, pulpotomies, SSCs, space-maintainer). - Patients have EHR since they are NYU Patients
- Patients are referred back to NYU if advanced behavioral techniques ( nitrous, sedation, GA) or specialized dental treatment is needed ( OS, Endo, Prostho, Ortho, Perio)
Radiographs from 10/17/18 – School Based Dental Program @ PS188
Since this patient was already seen a year ago in NYUCD. This visit was considered a recall visit.
Due to the clinical carious lesions present – 2 BW radiographs were recommended to observe any interproximal carious lesions (also to update the treatment plan that was never fulfilled) and PA#8 to observe the location of mesiodens and any update in eruption of #8 or the mesiodens.
Radiographic Interpretation revealed: Carious lesions in #3-O, #A-O, #14-O, #19-OB, #K-MOD, root tip present in tooth #L, #30-O, Mesiodens present ( disrupting the proper eruption of tooth #8) ***
Watch – #3-M, #13-M, #21-D
Figures 12, 13, & 14: Recall bitewing radiographs 10/17/18 @PS188 School Based Dental Program
Restorative Charting:
- Occlusion: mixed dentition
- Teeth clinically present: #3, #A, #5, #6 partially erupted, #7, #9, #10, #11partially erupted, #12, #13, #14,#19, #K, #21, #L root tip, #22, #23, #24, #25, #26, #27, #S, #30
- Teeth missing: #8 due to mesiodens, #T
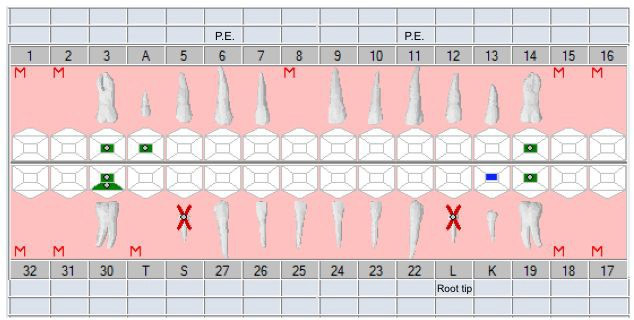
Figure 15: Odontogram with planned Tx
Patient did not receive dental treatment since her first time appointment at the NYU College of Dentistry. Patient did not return to the dental clinic at the NYU College of Dentistry due to the large amount of dental visits needed. Unfortunately, her mother could not take time off from work to bring the patient to her appointments. At the same time, the patient could not take time from school.
Some of the teeth that had carious lesions had already exfoliated and tooth #L broke down on it’s own-leaving behind one root tip (clinically present).
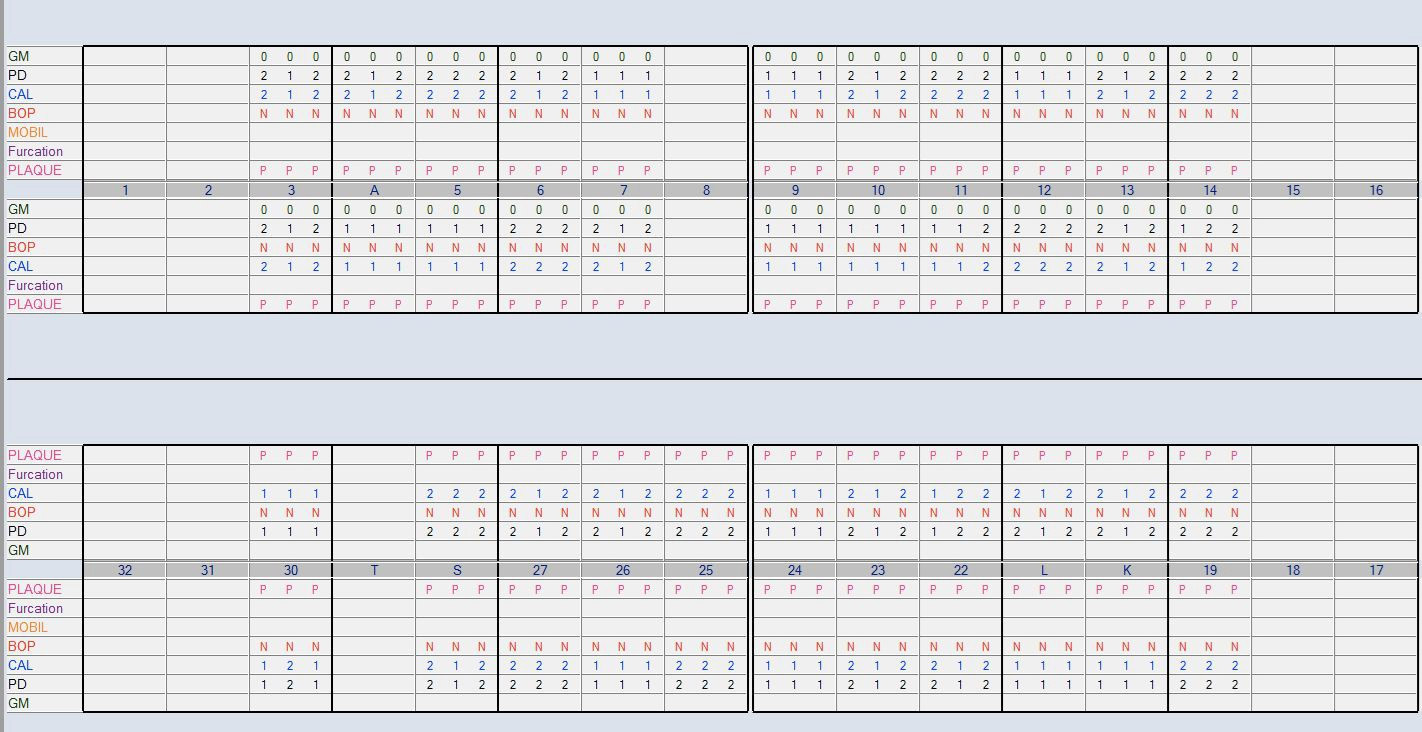
Periodontal Charting:
Periodontal Examination was performed to characterize the periodontal status as part of the overall treatment plan.
A basic periodontal examination was performed and recorded in the EHR.
- Frenums (maxillary labial, mandibular labial and lingual frenum) were evaluated – Within normal limits ( WNL)
- Disclosing tablet was used to evaluate plaque.
- Mobility Type 2 was observed in tooth #K.
Diagnostic Tools used:
- Dental Mirror, Explorer, Perio Probe
- Dental Loupes
- To provide proper illumination for provider
- Digital Radiographs using Nomad
- To provide a detailed and diagnostic dental evaluation
- To provide low radiation, instant and consistent image
- Easy access and portability
- Impressions and Dental Models
- To evaluate proper occlusion and determine future treatment
Treatment Plan:
- Comprehensive Treatment Plan
Phase 1: Examination- Detailed Examination
- Extraoral and Intraoral examination were conducted
- Prophylaxis
- Prophy cup and slow handpieces were used to conduct the dental cleaning
- Prophylaxis was performed after the use of a disclosing tablet to evaluate dental hygiene and location of plaque
- Diagnostic radiographs
- 2 BWs and 1 PA of tooth #8 were recommended to evaluate the extent of carious lesions ( previously indicated as carious lesions)
- PAN was previously taken in 2017 at NYUCD
- Fluoride Varnish
- ○ Using gauze to dry the surfaces of teeth prior to applying varnish over teeth
- Explaining the importance of fluoride
- Oral hygiene instructions
- Disclosing tablet and mirror – to show the areas where food/plaque accumulates
- Toothbrush/ Mirror: to show proper way to brush their teeth
- Floss/ Mirror: to show the importance and the proper way of flossing
Since we provided this treatment at the school based dental program, mother was contacted in writing and by phone in order to explain the dental findings and the treatment plan that was created. Mother understood and agreed to treatment.
*** Patient’s chief complaint was about her appearance – a mesiodens is impacting the proper eruption of tooth #8. Mother was explained that patient would need a consultation with the oral surgery team for proper removal of the mesiodens (due to impaction).
Phase 2: Restorative Treatment
Mother was called before every dental appointment at the school based program to let her know about the treatment that would be performed for the day. A follow up phone call was made at the end of the day to ask how the patient was feeling after each procedure.
- Restorations:
- Resin 1 surface posterior composite in #3-O, #14-O, #19-O,
- Resin 2 surfaces posterior composite in #A-OL, #30-OB
Patient’s behavior was ++ under the Frankel Scale. We used tell-show-do at each visit. A patient mirror was used at each visit – so that patient will feel more comfortable with the procedure and the dental team.
For the restorative treatment, topical anesthesia and 1 carpule of 2% lidocaine was used for the restoration in tooth #30-OB and #19-O. Isovac systems were used for isolation. Carious lesions were removed with slow and high speed handpieces. Carious lesions removal were checked by a pediatric dental faculty prior to restoring them with resin.
Occlusion was checked with articulating paper.- Extractions
- Extraction on tooth #S and extraction of root tip #L
- Mesiodens removal which was impeding the proper eruption of tooth #8 ( chief complaint for patient)
Patient’s behavior was ++ under the Frankel Scale. We would use tell show do at each visit. A patient mirror was used at each visit – so that patient will feel more comfortable with the procedure and the dental team.
For extraction procedures, topical anesthesia and 1 carpule of 2 % lidocaine was used for both teeth #S and L. Periosteal elevator was used, as well as mandibular forces. A protective gauze was used to prevent any aspiration. Post-op instructions were given to the patient, teachers and mother. One and two week follow up appointments were scheduled to evaluate proper healing.
Phase 3: Referral to Oral Surgery Clinic
Patient was referred to Oral Surgery Clinic for consultation and removal of mesiodens. The appointment was scheduled on patient’s mother day off from work. A car service was booked for the mother, patient and siblings to come to the oral surgery clinic for a consultation and removal.
Patient’s behavior was rated ++ in the Frankel Scale. Therefore, we recommended to have the surgery procedure under nitrous and local anesthesia. A pediatric dental faculty was present during the procedure, as well as oral surgery resident and faculty.
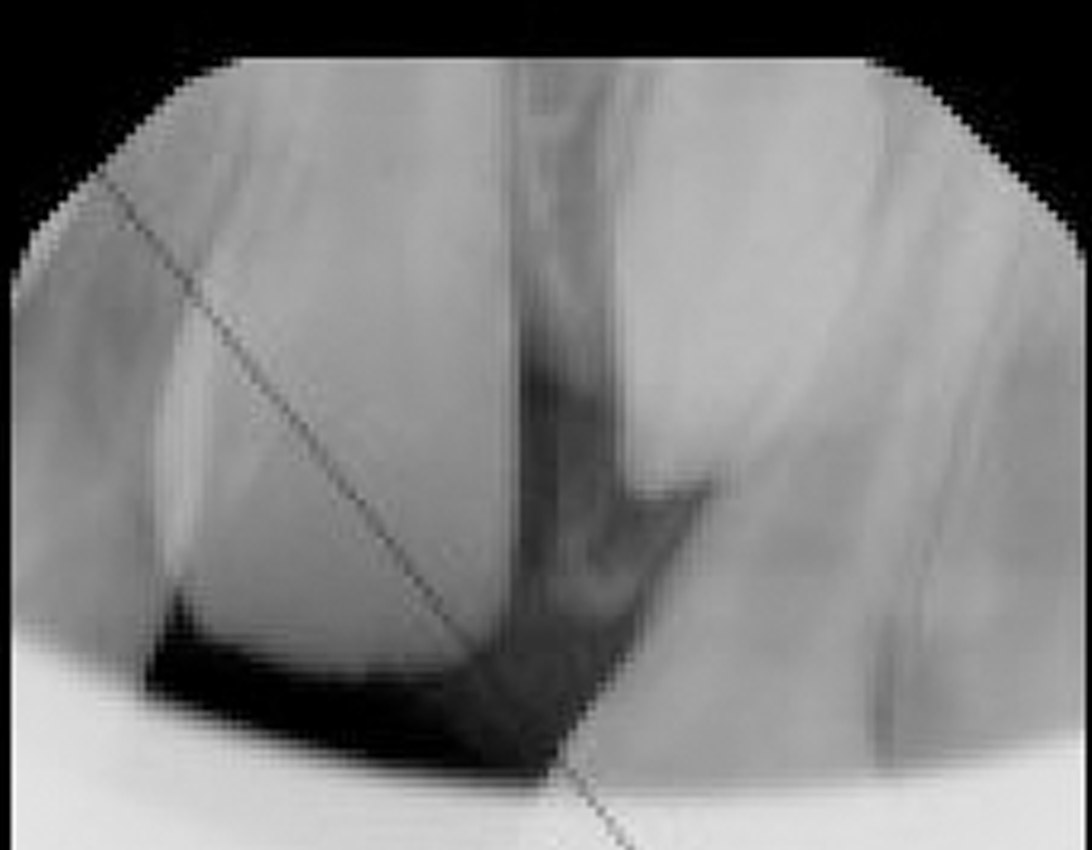
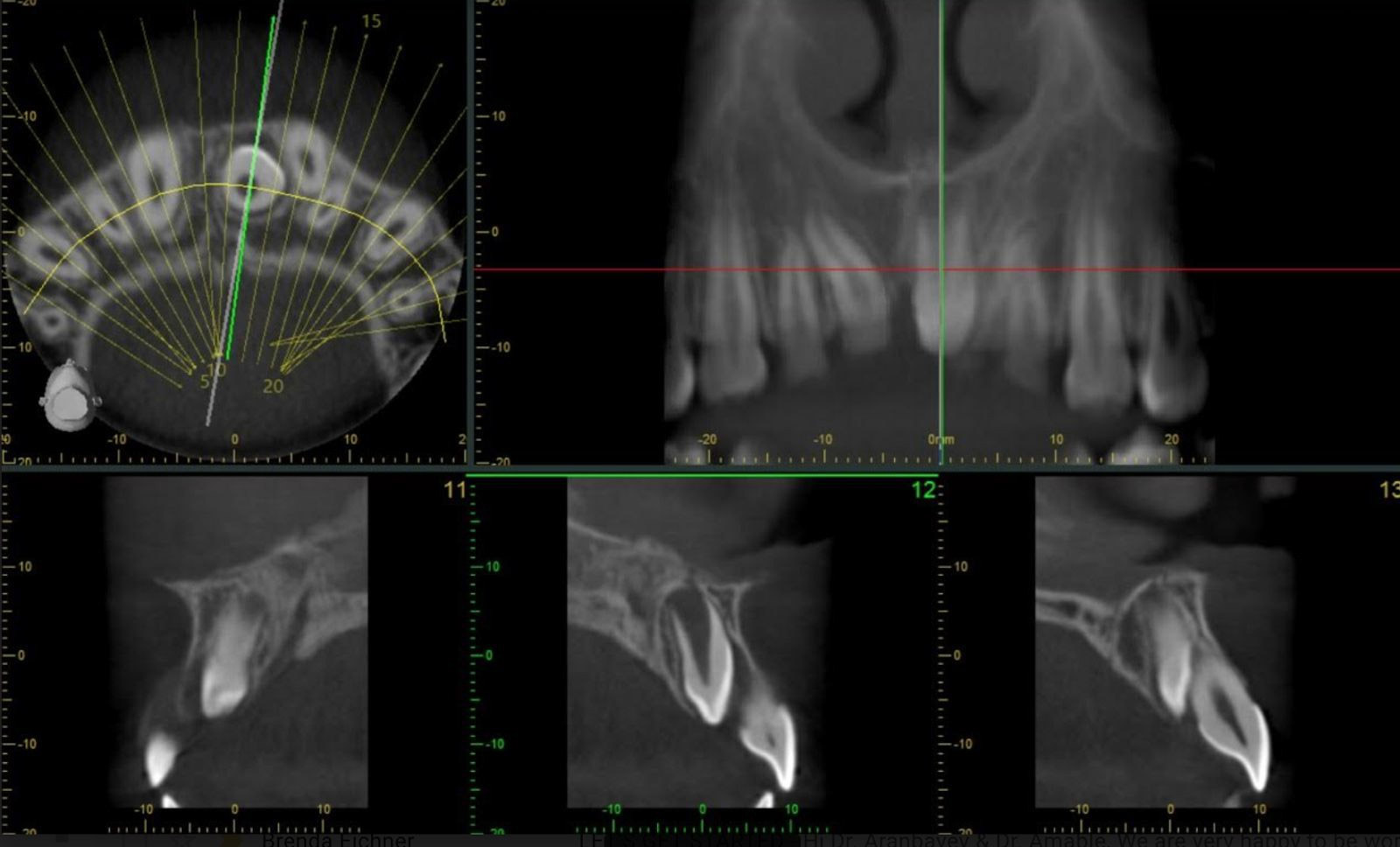
- CT-Scan was ordered and taken for evaluation of exact position/location of mesiodens.
- Extraction of Mesiodens under nitrous oxide and local anesthesia. Oral surgeon resident performed the mesiodens removal without any complications.
Figures 22-24: CT scan of Mesiodens, and post operative diagnostic casts
Phase 4: Orthodontic Consult
Patient was scheduled for a consultation with the orthodontic team at NYUCD in Nov 2019.
- Detailed Examination
- Preventive Treatment:
- Periodic Exams every 3 months – patient is considered high risk
- Prophylaxis
- Fluoride varnish
- Important to be placed every 3 months
- X-rays – Bws radiographs every 6 months.
- Oral hygiene instructions
- Use of disclosing tablet to evaluate proper oral hygiene.
- Periodic Exams every 3 months – patient is considered high risk
Oral Hygiene Recommendations:
- Brushing twice a day ( morning and night) with a fluoridated toothpaste for 2 minutes.
- Place your toothbrush at a 45-degree angle to the gums.
- Gently move the brush back and forth in short (tooth-wide) strokes.
- Brush the outer surfaces, the inner surfaces, and the chewing surfaces of the teeth.
- To clean the inside surfaces of the front teeth, tilt the brush vertically and make several up-and-down strokes.
- Use of dental floss once a day ( at night) using the C shape technique against each tooth.
- Use of fluoridated mouthwash every night
- Eat a balanced diet that limits sugary beverages and snacks.
- Regular visits to your dentist- every 3 or 6 months ( depending on the dentist’s recommendation) for a check-up and cleanings.
Figures 17-21: Post operative photos after completed tx plan
Recall visit x-rays:
Figures 25-27: Recall visit 9/18/19 radiographs
Discussion and Answer to the Clinical Question:
Our clinical question: “How do school-based dental programs eliminate the barriers to dental care for hispanic pediatric dental populations?”
Our patient C.D., seeked dental care at NYUCD in 2017, however due to the amount of dental treatment and dental visits needed, the patient was not able to return to commence with the recommended treatment plan. When her mother was later asked about why the patient did not return to NYUCD for dental treatment, she explained that it was due to the geographic and socio-economic barriers that most patients like patient C.D. encounter. More specifically, the barriers that were difficult to overcome were: lack of transportation, lack of dental appointments after 4:00pm (after work and school), lack of school permission (after two missed days of school – student gets penalized), lack of work permission (due to paycut and limited number of sick days to be used) and lack of babysitter help to take care of her other two children.
The school based dental program at PS188 was created after reading the New York Times article published on June 2016. This article describes the crude reality that children at PS188 go through everyday – around 47% of those students are homeless. Our patient was part of that percentage at some point. Our patient used to live in the shelter across from PS188 and used to receive breakfast, lunch and dinner at the school. PS 188 is open from 7:00am – 7:00pm.
The school based dental program at PS 188 was created exactly a year after our patient had her first dental visit at NYUCD.
Our patient signed up for this program on September 2018. Her first dental examination at the school based dental program occured in October 2018, where she received a detailed examination, x-rays, prophylaxis and fluoride treatment. After finding clinical and radiographic cavities, as well as a mesiodens – mom was contacted to inform her of the treatment plan that was recommended. Patient C.D. returned every week until her treatment was completed.
Our patient not only received all the treatment listed in her treatment plan, but also was provided with oral hygiene instructions at every visit.
Our dental program eliminated all the barriers that our patient and her mother encountered while trying to obtain dental care. Transportation was not needed since our school based program is established at the patient’s elementary school. Days of work or school were not missed – since mom did not have to be present unless she decided to and patient didn’t need to miss school since treatment was provided at her school. There was no language barrier since the pediatric dental faculty and dental students are bilingual. The number of visits for dental treatment was not an impediment to treatment since patient would only miss a max of 1 hour of class during dental treatment.
This is the case not only for our patient, but for 85% of the students at this school that signed up to our program.
Patient Outcome:
All of patient C.D.’s caries were treated after the establishment of a dental home through the Bringing Smiles Dental Program. Additionally, patient C.D. went through the extraction of tooth #S and the extraction of the root tip of tooth #L. After the mesiodens was diagnosed and a referral was sent to Oral Surgery, patient C.D. was successfully treated for the extraction of the mesiodens between tooth #8 and #9. Patient is awaiting her consult with the orthodontics department to continue receiving timely dental treatment. Even tough patient C.D. received full dental care through a complete treatment plan, it is imperative that she understands the importance of preventative dentistry. She must comprehend the importance of maintaining proper oral care at home as well as presenting for recall appointments and prophylaxis. Some of the complications that arose while treating patient C.D. dealt with making traveling arrangements. Many times, transportation was made available to the patient.
Conclusion
One of the goals of this case report is to explain how school-based dental programs positively impact hispanic pediatric dental patients by reducing the barriers to dental care. Many of the barriers that low-income, minority populations face deal with cultural, economic, geographic and structural barriers, to name a few. By delivering dental services to public school systems, we are able to halt the increasing numbers of untreated tooth decay, provide early diagnosis of oral pathology and reduce the lack of dental education in the pediatric population made up of minorities and low-income communities.
References
- 1.U.S. Department of Health and Human Services. Oral health in America: A report of the Surgeon General, Executive summary. Rockville, MD: National Institutes of Health, National Institute of Dental and Craniofacial Research. 2000.
- 2.Chen KJ, Gao SS, Duangthip D, Lo ECM, Chu CH. Prevalence of early childhood caries among 5-year-old children: A systematic review. J Investig Clin Dent 2019;10(1):e12376. doi:10.1111/jicd.12376
- 3.Fleming E, Afful J. Prevalence of Total and Untreated Dental Caries Among Youth: United States, 2015–2016. NCHS Data Brief 2018;307. Available at: https://www.cdc.gov/nchs/data/databriefs/db307.pdf.
- 4.Dye B, Thornton-Evans G, Li X, Iafolla T. Dental caries and tooth loss in adults in the United States, 2011-2012. NCHS Data Brief. 2015;197.
- 5.Pitts NB, Zero DT, Marsh PD, Ekstrand K, Weintraub JA, Ramos-Gomez F, et al. Dental caries. Nat Rev Dis Primers 2017;25(3):17030.
- 6.World Health Organization. Risk factors. Available at: https://www.who.int/topics/risk_factors/en/
- 7.Tagliaferro E, Pardi E, Ambrosano V, Meneghim G, Pereira, MAC. An overview of caries risk assessment in 0-18 year-olds over the last ten years (1997-2007). Braz J Oral Sci 2008;7(27):7.
- 8.Bibby BG, Krobicka A. An in vitro method for making repeated pH measurements on human dental plaque. J Dent Res 1984;63:906-9.
- 9.American Dental Association. Caries Risk Assessment Form (Age 0-6). Available at: https://www.ada.org/~/media/ADA/Member%20Center/FIles/topics_caries_under6.pdf.
- 10.American Dental Association. Caries Risk Assessment Form (Age >6). Available at: http://www.ada.org/~/media/ADA/Science%20and%20Research/Files/topic_caries_over6.ashx.
- 11.AAPD. Caries-risk Assessment and Management for Infants, Children, and Adolescents. Latest revision, 2019. Available at: https://www.aapd.org/media/Policies_Guidelines/BP_CariesRiskAssessment.pdf
- 12.AAPD. Best Practices. Perinatal and Infant Oral Health Care. 2016.. Available at: https://www.aapd.org/globalassets/media/policies_guidelines/bp_perinataloralhealthcare.pdf.
- 13.Dasanayake AP, Warnakulasuriya S, Harris CK, Cooper DJ, Peters TJ, Gelbier S. Tooth decay in alcohol abusers compared to alcohol and drug abusers. Int J Dent 2010;2010:786503.
- 14.Boersma JG, van der Veen MH, Lagerweij MD, Bokhout B, Prahl-Andersen B. Caries prevalence measured with QLF after treatment with fixed orthodontic appliances: influencing factors. Caries Res 2005;39(1):41-7.
- 15.Opal S, Garg S, Jain J, Walia I. Genetic factors affecting dental caries risk. Aust Dent J 2015;60:2-11.
- 16.Gomez A, Espinoza JL, Harkins DM, Leong P, Saffery R, Bockmann M et al. Host genetic control of the oral microbiome in health and disease. Cell Host Microbe 2017;22:269-78 e263.
- 17.Featherstone JDB, Alston P, Chaffee BW, Rechmann P. Caries Management by Risk Assessment (CAMBRA)*: An Update for Use in Clinical Practice for Patients Aged Through Adult. In: CAMBRA® Caries Management by Risk Assessment A Comprehensive Caries Management Guide for Dental Professionals. (2019) Available at: https://www.cdafoundation.org/Portals/0/pdfs/cambra_handbook.pdf.
- 18.Cagetti MG, Bontà G, Cocco F, Lingstrom P, Strohmenger L, Campus G. Are standardized caries risk assessment models effective in assessing actual caries status and future caries increment? A systematic review. BMC Oral Health 2018;18(1):123. doi: 10.1186/s12903-018-0585-4.
- 19.Malmö University. Cariogram – Download. Available at: https://www.mah.se/fakulteter-och-omraden/Odontologiska-fakulteten/Avdelning-och-kansli/Cariologi/Cariogram/.
- 20.Petsi G , Gizani S, Twetman S, Kavvadia K. Cariogram caries risk profiles in adolescent orthodontic patients with and without some salivary variables. Angle Orthod 2014;84(5):891-5. doi:10.2319/080113-573.1.
- 21.Martin J, Mills S, Foley ME. Innovative models of dental care delivery and coverage. Patient-centric dental benefits based on digital oral health risk assessment. Dent Clin N Am 2018;62:319-25.
- 22.Chapple L, Yonel Z. Oral Health Risk Assessment. Dent Update 2018;45:841-7.
- 23.American Dental Association. Electronic oral health risk assessment tools. SCDI White Paper No. 1074, 2013. Available at: http://www.ada.org/~/media/ADA/Science%20and%20Research/Files/ADAWhitePaperNo1074.pdf?la=en.
- 24.Twetman S, Banerjee A. (2020) Caries Risk Assessment. In: Chapple I, Papapanou P. (eds) Risk Assessment in Oral Health. Springer, Cham.
- 25.Rechmann P, Chaffee BW, Rechmann BMT, Featherstone JDB. Caries Management by Risk Assessment: Results From a Practice-Based Research Network Study. J Calif Dent Assoc 2019;47(1):15-24.
- 26.Mertz E, Wides C, White J. Clinician attitudes, skills, motivations and experience following the implementation of clinical decision support tools in a large dental practice. J Evid Based Dent Pract 2017;17(1):1-12.
- 27.Dou L, Luo J, Fu X, Tang Y, Gao J, Yang D. The validity of caries risk assessment in young adults with past caries experience using a screening Cariogram model without saliva tests. Int Dent J 2018;68(4):221-6. doi: 10.1111/idj.12378
- 28.Thyvalikakath T, Song M, Schleyer T. Perceptions and attitudes toward performing risk assessment for periodontal disease: a focus group exploration. BMC Oral Health 2018;18(1):90.
- 29.Riley JL 3rd, Gordan VV, Ajmo CT, Bockman H, Jackson MB, Gilbert GH. Dentists’ use of caries risk assessment and individualized caries prevention for their adult patients: findings from The Dental Practice-Based Research Network. Community Dent Oral Epidemiol 2011;39(6):564-73.
- 30.Weyant RJ, Tracy SL, Anselmo T, Frantsve-Hawley J, Meyer DM, Beltrán-Aguilar ED et al. Topical fluoride for caries prevention. J Am Dent Assoc 2013;144(11):1279-91. doi.org/10.14219/jada.archive.2013.0057
- 31.American Dental Association Council on Scientific Affairs. Fluoride toothpaste use for young children. J Am Dent Assoc 2013;145(2):190-1. doi.org/10.14219/jada.2013.47
- 32.Wright JT, Crall JJ, Fontana M, Gillette EJ, Nový BB, Dhar V et al. Evidence-based clinical practice guideline for the use of pit-and-fissure sealants. A report of the American Dental Association and the American Academy of Pediatric Dentistry. J Am Dent Assoc 2016;147(8):672-82.E12. doi.org/10.1016/j.adaj.2016.06.001
- 33.Slayton RL, Urquhart O, Araujo MWB, Fontana M, Guzmán-Armstrong S, Nascimento MM et al. Evidence-based clinical practice guideline on nonrestorative treatments for carious lesions. A report from the American Dental Association. J Am Dent Assoc 2018;149(10):P837-49.E10. doi.org/10.1016/j.adaj.2018.07.002
- 34.Baskaradoss JK. Relationship between oral health literacy and oral health status. BMC Oral Health 2018;18:172. Available at: https://doi.org/10.1186/s12903-018-0640-1.
- 35.Collins FM. Oral health literacy. Available at: https://www.colgateoralhealthnetwork.com/article/oral-health-literacy/
- 36.Alian AY, McNally ME, Fure S, Birkhed D. Assessment of Caries Risk in Elderly Patients Using the Cariogram Model. J Can Dent Assoc 2006;72(5):459–63.
- 37.Edwards AGK, Hood, K, Matthews EJ et al. The effectiveness of one to one risk communication interventions in health care: a systematic review. Med Decis Making 2000;20:290-7.
- 38.Eden E, Frencken J, Gao S, et al. Managing dental caries against the backdrop of COVID-19: approaches to reduce aerosol generation. Br Dent J. 2020;229:411-416. https://doi.org/10.1038/s41415-020-2153-y


:sharpen(level=0):output(format=jpeg)/up/2023/05/Vanessa-Mancuso-Cortinas-1-3.jpg)
:sharpen(level=0):output(format=jpeg)/up/2023/05/Stephanie-Aya-3.jpg)
:sharpen(level=0):output(format=jpeg)/up/2020/02/Childhood-Caries-and-Supernumerary-Tooth-Removalthumbnail-photo-2.jpg)