Dental Stain
Dental stain is commonly encountered worldwide. Civilizations throughout history have tried to prevent and remove dental stain, including the ancient Egyptians approximately 4,000 years ago who used a mixture of ground pumice and vinegar to whiten their teeth.1A history of toothwhitening. Available at: https://www.seattletimes.com/seattle-news/health/a-history-of-tooth-whitening/. Dental stain is defined as extrinsic stain (ES) when present at the tooth surface and in the pellicle, and as intrinsic stain (IS) when present within the dental hard tissue. In addition, ES can enter teeth through surface defects, becoming internalized and resulting in IS.2Addy M, Moran J. Mechanisms of stain formation on teeth, in particular associated with metal ions and antiseptics. Adv Dent Res 1995;9:450-6.,3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16. In order to prevent avoidable stain and to treat existing stain, the etiology needs to be identified.
Etiology of ES
ES occurs when chromogens become incorporated into the pellicle, or may develop indirectly through chemical interactions at the tooth surface with metal salts or cationic oral chemotherapeutics.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.,4Proctor GB, Pramanik R, Carpenter GH. Salivary proteins interact with dietary constituents to modulate tooth staining. J Dent Res 2005;84(1):73-8.,5Eriksen HM, Nordbø H, Kantanen H, Ellingsen JE. Chemical plaque control and extrinsic tooth discoloration. A review of possible mechanisms. J Clin Periodontol 1985;12:345-50. Alternative hypotheses suggest that hydrogen forces, van der Waals forces and hydrophobic interactions enable the close proximity and adhesion of chromogens to the tooth surface.6Nathoo SA. The chemistry and mechanisms of extrinsic and intrinsic discoloration. J Am Dent Assoc 1997;128:6S-10S.,7Hattab FN, Qudeimat MA, Al-Rimawi HS. Dental discoloration: An overview. J Esthet Dent 1999;11:291-310.,8Azer SS, Hague AL, Johnston WM. Effect of pH on tooth discoloration from food colorant in vitro. J Dent 2010;38(2):e106-e9. Poor oral hygiene is associated with increased levels of ES.9Ellingsen JE, Erkisen HM, Rolla G. Extrinsic dental stain caused by stannous fluoride. Scand J Dent Res 1982;90(1):9-13. Further, surface roughness and cracks encourages its accumulation.6Nathoo SA. The chemistry and mechanisms of extrinsic and intrinsic discoloration. J Am Dent Assoc 1997;128:6S-10S.
Tobacco and dietary factors
Smoking tobacco is a well-known source of direct ES, resulting in discoloration ranging from yellowish-light brown to dark brown/black.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.,6Nathoo SA. The chemistry and mechanisms of extrinsic and intrinsic discoloration. J Am Dent Assoc 1997;128:6S-10S.,10Sruthy Prathap H, Vinitha R, Boloor A, Rao AS. Extrinsic stains and management: A new insight. J Acad Indus Res 2013;1(8):435. Using smokeless tobacco also causes ES, and when betel leaves/areca nut is combined with smokeless tobacco, or chewed, the resulting stain is red-black.7Hattab FN, Qudeimat MA, Al-Rimawi HS. Dental discoloration: An overview. J Esthet Dent 1999;11:291-310.,11Savitz DA, Meyer RE, Tanzer JM, Mirvish SS, Lewin F. Public health implications of smokeless tobacco use as a harm reduction strategy. Am J Public Health 2006;96(11):1934-9. Dietary sources of chromogens include coffee, tea, red wine, spicy foods and dark sauces.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.,6Nathoo SA. The chemistry and mechanisms of extrinsic and intrinsic discoloration. J Am Dent Assoc 1997;128:6S-10S. Further, certain vegetables and fruits have a propensity to cause ES, e.g., beetroot, blueberries and blackberries.12Evans V. Living well. Top 10 teeth-staining foods. Available at: https://www.bupa.co.uk/newsroom/ourviews/teeth-staining-foods. It is believed that polyphenolic compounds, responsible for the color of highly-pigmented foods, interact with the salivary pellicle thereby forming ES.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.,8Azer SS, Hague AL, Johnston WM. Effect of pH on tooth discoloration from food colorant in vitro. J Dent 2010;38(2):e106-e9. Acidic compounds (food dyes) also have a greater propensity to cause ES than those with a higher pH.8Azer SS, Hague AL, Johnston WM. Effect of pH on tooth discoloration from food colorant in vitro. J Dent 2010;38(2):e106-e9. In addition, acidic foods and beverages can erode enamel, compounding the problem by rendering it more susceptible to staining.7Hattab FN, Qudeimat MA, Al-Rimawi HS. Dental discoloration: An overview. J Esthet Dent 1999;11:291-310.
Bacterial chromogens
Yellow, orange, green and black ES are associated with bacterial chromogens and occur primarily in children.13Eriksen HM, Nordbø H. Extrinsic discoloration of teeth. J Clin Periodontol 1978;5(4):229-36.,14Żyła T, Kawala B, Antoszewska-Smith J, Kawala M. Black stain and dental caries: A review of the literature. Biomed Res Int 2015:469392.,15Koch MJ, Bove M, Schroff J, Perlea P, Garcia-Godoy F, Staehle HJ. Black stain and dental caries in schoolchildren in Potenza, Italy. ASDC J Dent Child. 2001;68(5-6):353-5,02. Black ES presents as a black line or a series of dark dots along the gingival margin, with an estimated prevalence in children of 2.4% to 18% and occurring more frequently in children with lower caries rates.14Żyła T, Kawala B, Antoszewska-Smith J, Kawala M. Black stain and dental caries: A review of the literature. Biomed Res Int 2015:469392.,15Koch MJ, Bove M, Schroff J, Perlea P, Garcia-Godoy F, Staehle HJ. Black stain and dental caries in schoolchildren in Potenza, Italy. ASDC J Dent Child. 2001;68(5-6):353-5,02. A predominance of Gram-positive rods, in particular Actinomycetes, has been found in children with black ES, and a recent study also found increased levels of Cardiobacterium, Haemophilus, Corynebacterium, Tannerella and Treponema species.14Żyła T, Kawala B, Antoszewska-Smith J, Kawala M. Black stain and dental caries: A review of the literature. Biomed Res Int 2015:469392.,16Li Y, Zhang Q, Zhang F, Liu R, Liu H, Chen F. Analysis of the microbiota of black stain in the primary dentition. PLoS One 2015;10(9):e0137030. Available at: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0137030 Diet and/or iron supplementation may play a role, and iron compounds or high concentrations of sulfur in metal complexes may be involved.14Żyła T, Kawala B, Antoszewska-Smith J, Kawala M. Black stain and dental caries: A review of the literature. Biomed Res Int 2015:469392. (Table 1)
| Table 1. Sources and manifestations of direct ES | |
|---|---|
| Tobacco smoking | Yellowish-brown to brown/black stain |
| Smokeless tobacco | Yellowish-brown stain |
| Betel leaves/areca nut in smokeless tobacco/chewed | Red-black stain |
| Foods and drinks | Yellowish-brown stain |
| Bacterial chromogens | Yellow, orange, green or black stain |
Indirect ES
Indirect ES can be experienced with use of stannous fluoride (SF), cationic mouth rinses and aqueous iron salts.3,4Proctor GB, Pramanik R, Carpenter GH. Salivary proteins interact with dietary constituents to modulate tooth staining. J Dent Res 2005;84(1):73-8.,6Nathoo SA. The chemistry and mechanisms of extrinsic and intrinsic discoloration. J Am Dent Assoc 1997;128:6S-10S.,9Ellingsen JE, Erkisen HM, Rolla G. Extrinsic dental stain caused by stannous fluoride. Scand J Dent Res 1982;90(1):9-13.,17de Baat C, Zweers PGMA, van Loveren C, Vissink A. Medicaments and oral healthcare 5. Adverse effects of medications and over-the-counter drugs on teeth. [In Dutch]. Ned Tijdschr Tandheelkd 2017;124(10):485-91. doi:10.5177/ntvt.2017.10.17142. ES associated with chlorhexidine gluconate (CHX) rinse ranges from yellowish-brown to brown or blackish stain in color. This discoloration is believed to occur when dietary anionic chromogens react with cationic CHX adsorbed at the tooth surface.2Addy M, Moran J. Mechanisms of stain formation on teeth, in particular associated with metal ions and antiseptics. Adv Dent Res 1995;9:450-6.,3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16. Other theories suggest that CHX alters the speed of pellicle formation or denaturation, thereby changing surface reactions, or through exposure of sulfur radicals that can interact with metal ions.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16. Further, other cationic agents may result in indirect ES, including quaternary ammonium, essential oils and cetylpyridinium chloride mouth rinses.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.,17de Baat C, Zweers PGMA, van Loveren C, Vissink A. Medicaments and oral healthcare 5. Adverse effects of medications and over-the-counter drugs on teeth. [In Dutch]. Ned Tijdschr Tandheelkd 2017;124(10):485-91. doi:10.5177/ntvt.2017.10.17142. Essential oils (e.g., tea tree oils, clove oil, sandalwood and lemon oil) have been found to cause ES in combination with tea drinking.17de Baat C, Zweers PGMA, van Loveren C, Vissink A. Medicaments and oral healthcare 5. Adverse effects of medications and over-the-counter drugs on teeth. [In Dutch]. Ned Tijdschr Tandheelkd 2017;124(10):485-91. doi:10.5177/ntvt.2017.10.17142.
The capacity of unstabilized/poorly stabilized formulations of SF to promote a yellowish-brown stain is well-recognized.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.,9Ellingsen JE, Erkisen HM, Rolla G. Extrinsic dental stain caused by stannous fluoride. Scand J Dent Res 1982;90(1):9-13. ES occurs due to hydrolysis/oxidation of poorly stabilized SF in dentifrices, gels and rinses.9Ellingsen JE, Erkisen HM, Rolla G. Extrinsic dental stain caused by stannous fluoride. Scand J Dent Res 1982;90(1):9-13.,17de Baat C, Zweers PGMA, van Loveren C, Vissink A. Medicaments and oral healthcare 5. Adverse effects of medications and over-the-counter drugs on teeth. [In Dutch]. Ned Tijdschr Tandheelkd 2017;124(10):485-91. doi:10.5177/ntvt.2017.10.17142. Higher levels of stannic ions (Sn4+) result in ES. In addition, iron supplements cause black ES, and medications or occupational exposure can cause black, green and purplish discoloration with use of iron, copper and potassium permanganate salts, respectively.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.
Green and yellowish-brown discoloration has been reported in competitive swimmers spending long periods of time in chlorinated swimming pools.18Escartin JL, Arnedo A, Pinto V, Vela MJ. A study of dental staining among competitive swimmers. Community Dent Oral Epidemiol 2000;28(1):10-7. (Table 2) Pool water with a pH >6.5 is believed to cause break down of proteins at the tooth surface, resulting in stain formation.19Scheper WA, van Nieuw Amerongen A, Eijkman MA. Oral conditions in swimmers. [Article in Dutch] Ned Tijdschr Tandheelkd 2005;112(4):147-8. In one study, 60.2% of competitive swimmers experienced ES compared to 12.9% of individuals in other sports.18Escartin JL, Arnedo A, Pinto V, Vela MJ. A study of dental staining among competitive swimmers. Community Dent Oral Epidemiol 2000;28(1):10-7. (Figure 1)
| Table 2. Sources and manifestations of indirect ES | |
|---|---|
| Stannous fluoride products | Yellowish-brown stain |
| Chlorhexidine gluconate rinse | Yellowish-brown to dark brown stain |
| Essential oils rinse | Yellowish stain |
| CPC mouth rinse | Yellowish stain |
| Iron, copper and potassium permanganate medications, or occupational exposure | Black, green and purplish stain, respectively |
| Long-duration use of chlorinated swimming pools | Green stain |
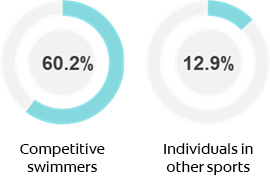
Figure 1. Prevalence of green stain among competitive swimmers
Preventing, inhibiting and treating ES
Oral hygiene and dietary advice, as well as advice on abstaining from the use of tobacco products (and betel leaves/areca nut if indicated), should be provided routinely to patients. Appropriate oral hygiene and healthy dietary choices help to maintain and improve oral health, and to prevent stain build-up.18Escartin JL, Arnedo A, Pinto V, Vela MJ. A study of dental staining among competitive swimmers. Community Dent Oral Epidemiol 2000;28(1):10-7. In addition to stain removal, routine prophylaxis polishes the surface, which helps to maintain a smooth surface and discourages stain formation. Competitive swimmers should be advised on the role of oral hygiene and routine prophylaxis in reducing the risk of green ES.
Oral care recommendations should consider the ability of a product to prevent/inhibit and remove ES. Dentifrices contain abrasives for their cleaning and stain removal benefit during brushing and improve mouthfeel and compliance with oral hygiene20Lobene R, Hefferren J, and Dentifrice Function Committee. Clinical response of non-abrasive dentifrice use in dental hygienists. J Dent Res 1996;75:88.. These are safe and effective for everyday use at an RDA of up to 250.21American Dental Association. Oral Health Topics. Toothpaste. Center for Scientific Information, ADA Science Institute. Updated August 2018. Available at: https://www.ada.org/en/member-center/oral-health-topics/toothpastes. A recent systematic review found whitening dentifrices to be effective in reducing ES.22Soeteman GD, Valkenburg C, Van der Weijden GA, Van Loveren C, Bakker E, Slot DE. Whitening dentifrice and tooth surface discoloration-a systematic review and meta-analysis Int J Dent Hyg. 2018 Feb;16(1):24-35. Whitening dentifrices may variously contain a high-cleaning abrasive, baking soda, stain-inhibiting agents and/or hydrogen peroxide.23Kakar A, Rustogi K, Zhang YP, Petrone ME, DeVizio W, Proskin HM. A clinical investigation of the tooth whitening efficacy of a new hydrogen peroxide-containing dentifrice J Clin Dent. 2004;15(2):41-5.,24Ghassemi A, Hooper W, Vorwerk L, Domke T, DeSciscio P, Nathoo S. Effectiveness of a new dentifrice with baking soda and peroxide in removing extrinsic stain and whitening teeth J Clin Dent. 2012;23(3):86-91.,25Isaacs RL, Bartizek RD, Owens TS, Walters PA, Gerlach RW. Maintenance of tooth color after prophylaxis: comparison of three dentifrices. J Clin Dent 2001;12(2):51-5. Further, if medium- or long-duration use of an antimicrobial rinse is indicated, options are available that result in less stain and avoid side effects associated with CHX. In addition, oxygenating products, e.g., hydrogen peroxide, help to inhibit ES.26Maanen-Schakel NWD van, Slot DE, Bakker EWP, Weijden GA van der. The effect of an oxygenating agent on chlorhexidine-induced extrinsic tooth staining: a systematic review. Int J Dent Hyg 2012;10:198-208.
Stabilized or anhydrous SF dentifrice inhibits stain formation. Stabilization reduces the level of stannic ions and can be achieved through the addition of stannous chloride (to provide extra stannous ions), amine fluoride, gluconate, or zinc phosphate.17de Baat C, Zweers PGMA, van Loveren C, Vissink A. Medicaments and oral healthcare 5. Adverse effects of medications and over-the-counter drugs on teeth. [In Dutch]. Ned Tijdschr Tandheelkd 2017;124(10):485-91. doi:10.5177/ntvt.2017.10.17142.,27Milleman JL, He T, Anastasia MK. Anti-calculus efficacy of a SnF2 dentifrice in a three-month clinical. J Dent Res 2017;96(spec iss A):Abstract 2816.,28Myers CP, Pappas I, Makwana E, Begum-Gafur R, Utgikar N, Alsina MA, Fitzgerald M, Trivedi HM, Gaillard J-F, Masters JG, Sullivan RJ. Solving the problem with stannous fluoride: Formulation, stabilization, and antimicrobial action. J Am Dent Assoc 2019;150)4S):S5-S13. In addition, chelating agents contained in stabilized stannous fluoride formulations become incorporated into the pellicle and inhibit stain deposition. These include pyrophosphates, polyphosphates, sodium hexametaphosphate and sodium phytate.9Ellingsen JE, Erkisen HM, Rolla G. Extrinsic dental stain caused by stannous fluoride. Scand J Dent Res 1982;90(1):9-13.,17de Baat C, Zweers PGMA, van Loveren C, Vissink A. Medicaments and oral healthcare 5. Adverse effects of medications and over-the-counter drugs on teeth. [In Dutch]. Ned Tijdschr Tandheelkd 2017;124(10):485-91. doi:10.5177/ntvt.2017.10.17142.,29Sensabaugh C, Sagel ME. Stannous fluoride dentifrice with sodium hexametaphosphate: review of laboratory, clinical and practice-based data. J Dent Hyg 2009;83(2):70-8.,30Milleman KR, Creeth JE, Burnett GR, Milleman JL. A randomized clinical trial to evaluate the stain removal efficacy of a sodium phytate dentifrice formulation. J Esthet Rest Dent 2018;30(2):E45-51.
| Table 3. Preventing and Managing ES |
|---|
| Advise patients on tobacco cessation and avoidance of tobacco |
| Advise patients against using betel leaves and areca nut |
| Advise patients on oral hygiene and routine prophylaxis |
| Advise competitive swimmers on the risk of green stain |
| Recommend oral care products that prevent/inhibit stain |
Etiology of IS
IS occurs in dentin in the presence of chromophores containing carbon double-bonds.6Nathoo SA. The chemistry and mechanisms of extrinsic and intrinsic discoloration. J Am Dent Assoc 1997;128:6S-10S. This can be the result of medications, fluorosis, hereditary conditions, systemic diseases, trauma, enamel hypoplasia and use of dental materials.2Addy M, Moran J. Mechanisms of stain formation on teeth, in particular associated with metal ions and antiseptics. Adv Dent Res 1995;9:450-6.,3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.,31Sanchez AR, Rogers RS III, Sheridan PJ. Tetracycline and other tetracycline-derivative staining of the teeth and oral cavity. Int J Dermatol 2004;43:709-15.,32Tredwin C, Scully C, Bagan-Sebastian J-V. Drug-induced dental disorders. Adverse Drug Reaction Bull 2005;232. ISSN 0044-6394.,33Love RM, Chandler NP. A scanning electron and confocal laser microscope investigation of tetracycline-affected human dentine. Int Endod J 1996;29(6):376-81.,34Agrawal P, Singh O, Nigam AK, Upadhyay S. Imatinib-induced dental hyperpigmentation in chronic myeloid leukemia in an adult female. Indian J Pharmacol 2015;47(6):685-6.,35Pendrys DG, Katz RV, Morse DE. Risk factors for enamel fluorosis in a nonfluoridated population. Am J Epidemiol 1996;143(8):808-15.,36Fejerskov O, Manji F, Baelum V. The nature and mechanisms of dental fluorosis in man. J Dent Res 1990;69(special issue):692-700.,37Bittencourt do Valle I, Eduardo VM, Goese TB, Oliviera ZFL, von Zeidler SV. Green teeth in the primary and permanent dentition. J Pediatr 2017;191:275.,38Kahler B, Rossi-Fedele G. A review of tooth discoloration after regenerative endodontic therapy. J Endod 2016;42(4):563-9. In addition, aging plays a role.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.

Figure 2. Severe tetracycline staining
Image courtesy of Dr. Joyce Bassett
Tetracycline and derivatives
Tetracycline chelates with calcium ions during tooth development, becoming incorporated into tooth structure.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.,31Sanchez AR, Rogers RS III, Sheridan PJ. Tetracycline and other tetracycline-derivative staining of the teeth and oral cavity. Int J Dermatol 2004;43:709-15.,32Tredwin C, Scully C, Bagan-Sebastian J-V. Drug-induced dental disorders. Adverse Drug Reaction Bull 2005;232. ISSN 0044-6394. The resulting discoloration is yellow, gray or brown; with/without banding; and, fluoresces when exposed to UV light.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16. (Figure 2) In addition, the root dentin of affected teeth has been found to contain fewer dentinal tubules and to exhibit altered crystal formation.33Love RM, Chandler NP. A scanning electron and confocal laser microscope investigation of tetracycline-affected human dentine. Int Endod J 1996;29(6):376-81. The severity and pattern of IS depends on the dose, age of the patient and duration of use.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.,31Sanchez AR, Rogers RS III, Sheridan PJ. Tetracycline and other tetracycline-derivative staining of the teeth and oral cavity. Int J Dermatol 2004;43:709-15. Tetracycline derivatives administered during dental development also cause IS.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.,32Tredwin C, Scully C, Bagan-Sebastian J-V. Drug-induced dental disorders. Adverse Drug Reaction Bull 2005;232. ISSN 0044-6394. Long-duration use of minocycline by adults, however, may also cause blue-grayish coronal discoloration and black/green roots, believed to be due to calcium-minocycline complexes in dentin.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.,32Tredwin C, Scully C, Bagan-Sebastian J-V. Drug-induced dental disorders. Adverse Drug Reaction Bull 2005;232. ISSN 0044-6394. It is worth noting that ciprofloxacin and imatinib mesylate may cause discoloration, neither of which is a tetracycline derivative.32Tredwin C, Scully C, Bagan-Sebastian J-V. Drug-induced dental disorders. Adverse Drug Reaction Bull 2005;232. ISSN 0044-6394.,34Agrawal P, Singh O, Nigam AK, Upadhyay S. Imatinib-induced dental hyperpigmentation in chronic myeloid leukemia in an adult female. Indian J Pharmacol 2015;47(6):685-6.
Dental Fluorosis
Dental fluorosis is characterized by enamel hypomineralization and porosities. It results from the ingestion of excessive amounts of fluoride, from all sources in total, over an extended period of time during tooth development and prior to pre-eruptive enamel maturation.35Pendrys DG, Katz RV, Morse DE. Risk factors for enamel fluorosis in a nonfluoridated population. Am J Epidemiol 1996;143(8):808-15.,36Fejerskov O, Manji F, Baelum V. The nature and mechanisms of dental fluorosis in man. J Dent Res 1990;69(special issue):692-700. Mild dental fluorosis manifests as barely discernable chalky areas or white striae. In contrast, severe fluorosis results in extensive brown/black stain, and pitted and brittle enamel.35Pendrys DG, Katz RV, Morse DE. Risk factors for enamel fluorosis in a nonfluoridated population. Am J Epidemiol 1996;143(8):808-15. Severe dental fluorosis occurs in geographic areas with endemic fluorosis caused by well water with naturally-occurring extremely high levels of fluoride.
Hereditary and systemic conditions and diseases
Amelogenesis imperfecta (AI) and dentinogenesis imperfecta (DI) are hereditary conditions with several variants. Enamel dysmineralization occurs with AI, and tooth discoloration may be mild and chalky, yellow or yellowish-brown.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16. DI type 1 manifests with enamel that chips off, leaving exposed dentin that is bluish/brown, opalesces and wears quickly. Congenital hyperbilirubinemia causes green IS, believed to be due to bile pigments deposited in the organic matrix of dentin during its formation.37Bittencourt do Valle I, Eduardo VM, Goese TB, Oliviera ZFL, von Zeidler SV. Green teeth in the primary and permanent dentition. J Pediatr 2017;191:275. Other etiologies for green IS include hemolytic anemia and internal hemorrhaging. Alkaptonuria manifests orally as brown stain in the permanent dentition. Congenital erythropoietic porphyria, which is rare, results in systemic build-up of porphyrins and red-brown IS in the primary and secondary dentition. Other rare conditions also result in IS.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.
Enamel Hypoplasia
The chalky defects associated with enamel hypoplasia can be the result of fetal injury, systemic diseases in young children, and local damage to a developing permanent tooth during trauma/infection to the overlying primary tooth.
Trauma
Pulpal trauma and pulpal remnants following root canal therapy cause grey to black discoloration, mainly derived from blood pigments.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16. Initially, a pinkish color may occur when pulpal bleeding related to trauma occurs and may disappear if revascularization occurs.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.
Dental procedures and materials
Some dental materials cause IS. In endodontic therapy, teeth treated with a triple antibiotic paste containing minocycline acquire grey IS.38Kahler B, Rossi-Fedele G. A review of tooth discoloration after regenerative endodontic therapy. J Endod 2016;42(4):563-9. Mineral trioxide aggregate, which contains bismuth oxide or another radiopaquer, also causes grey discoloration.38Kahler B, Rossi-Fedele G. A review of tooth discoloration after regenerative endodontic therapy. J Endod 2016;42(4):563-9. Grey/dark grey stain can also occur following use of silver diamine fluoride for the arrestment of dentinal caries, and grey stain occurs adjacent to dental amalgams. (Table 4)
| Table 4. Sources and manifestations of IS | |
|---|---|
| Tetracycline ingestion during tooth development | Yellow, gray or brown, with or without banding |
| Long-duration adult use of minocycline | Blue-grayish coronal discoloration and black/green roots |
| Dental fluorosis | Barely discernable chalky areas or white striae in mild fluorosis. Extensive brown/black stain in severe fluorosis |
| Amelogenesis imperfecta | Range from mild and chalky, to yellow or yellowish-brown |
| Dentinogenesis imperfecta Type 1 | Bluish/brown dentin that opalesces |
| Congenital hyperbilirubinemia; Hemolytic anemia; Internal hemorrhaging | Green stain |
| Alkaptonuria | Brown stain |
| Congenital erythropoietic porphyria | Brown stain |
| Enamel hypoplasia | Chalky white defects |
| Trauma | Grey to black discoloration with necrotic pulp/pulpal remnants |
| Dental materials | Grey with minocycline-containing antibiotic paste; mineral trioxide aggregate; silver diamine fluoride |
| Aging | Yellowish |
Aging
As individuals age, secondary dentin is laid down in the permanent dentition, increasing the depth of dentin and shrinking the pulp chamber. These factors result in a yellowed appearance. Stain also builds up in the absence of intervention over time, and changes in tooth surface morphology result in less refraction and reflection of light making teeth appear to be darker.39Ten Bosch JJ, Coops CC. Tooth color and reflectance as related to light scattering and enamel hardness. J Dent Res 1995;74:374-80.
Preventing and Managing Intrinsic Stain
IS associated with medications, fluorosis and dental materials is preventable. Further, where possible, alternative medications and materials can be used that do not stain, for example, antibiotic pastes that do not contain minocycline can be used during endodontic therapy.38Kahler B, Rossi-Fedele G. A review of tooth discoloration after regenerative endodontic therapy. J Endod 2016;42(4):563-9.
Tetracycline and its derivatives should be avoided during the second and third trimesters of pregnancy, by mothers who are breastfeeding, and in children during tooth development.3Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16. With respect to fluorosis, after teeth have undergone pre-eruptive maturation, they cannot develop fluorosis. This occurs by 6 years-of-age in the permanent dentition, with the exception of third molars. Therefore, until a child reaches this age, it is important to ensure appropriate dosing, use and supervision of products containing fluoride, including dentifrices, to optimize their anti-caries benefit while minimizing the risk of fluorosis. Drinking/using well water containing excessive amounts of fluoride should be avoided (if geographically possible) and it can be pre-treated to remove excess fluoride. Patients and parents should also be advised on the use of sports mouthguards to help prevent sports-related orofacial injuries.
When indicated, treatment of IS in the permanent dentition can be provided with in-office and/or home use tooth bleaching products. Additional options include microabrasion and restorative solutions.
Conclusions
Dental professionals play a key role in advising patients on the etiology of dental stain, its prevention and treatment. Patients and parents/guardians of children should routinely be given advice on diet, appropriate oral hygiene and use of fluoride, tobacco avoidance/cessation, and the prevention of sports-related orofacial trauma. Further, the selection of medications and materials should consider stain as a side effect.
ES is avoidable, while IS may or may not be avoidable depending on the etiology. For pre-existing ES, routine prophylaxis will remove discoloration. Pre-existing IS can typically be treated using tooth bleaching, microabrasion or a combination of these. It is essential to be able to identify the cause of dental stain in order to be able to offer advice on treatment options and stain prevention.
References
- 1.A history of toothwhitening. Available at: https://www.seattletimes.com/seattle-news/health/a-history-of-tooth-whitening/.
- 2.Addy M, Moran J. Mechanisms of stain formation on teeth, in particular associated with metal ions and antiseptics. Adv Dent Res 1995;9:450-6.
- 3.Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.
- 4.Proctor GB, Pramanik R, Carpenter GH. Salivary proteins interact with dietary constituents to modulate tooth staining. J Dent Res 2005;84(1):73-8.
- 5.Eriksen HM, Nordbø H, Kantanen H, Ellingsen JE. Chemical plaque control and extrinsic tooth discoloration. A review of possible mechanisms. J Clin Periodontol 1985;12:345-50.
- 6.Nathoo SA. The chemistry and mechanisms of extrinsic and intrinsic discoloration. J Am Dent Assoc 1997;128:6S-10S.
- 7.Hattab FN, Qudeimat MA, Al-Rimawi HS. Dental discoloration: An overview. J Esthet Dent 1999;11:291-310.
- 8.Azer SS, Hague AL, Johnston WM. Effect of pH on tooth discoloration from food colorant in vitro. J Dent 2010;38(2):e106-e9.
- 9.Ellingsen JE, Erkisen HM, Rolla G. Extrinsic dental stain caused by stannous fluoride. Scand J Dent Res 1982;90(1):9-13.
- 10.Sruthy Prathap H, Vinitha R, Boloor A, Rao AS. Extrinsic stains and management: A new insight. J Acad Indus Res 2013;1(8):435.
- 11.Savitz DA, Meyer RE, Tanzer JM, Mirvish SS, Lewin F. Public health implications of smokeless tobacco use as a harm reduction strategy. Am J Public Health 2006;96(11):1934-9.
- 12.Evans V. Living well. Top 10 teeth-staining foods. Available at: https://www.bupa.co.uk/newsroom/ourviews/teeth-staining-foods.
- 13.Eriksen HM, Nordbø H. Extrinsic discoloration of teeth. J Clin Periodontol 1978;5(4):229-36.
- 14.Żyła T, Kawala B, Antoszewska-Smith J, Kawala M. Black stain and dental caries: A review of the literature. Biomed Res Int 2015:469392.
- 15.Koch MJ, Bove M, Schroff J, Perlea P, Garcia-Godoy F, Staehle HJ. Black stain and dental caries in schoolchildren in Potenza, Italy. ASDC J Dent Child. 2001;68(5-6):353-5,02.
- 16.Li Y, Zhang Q, Zhang F, Liu R, Liu H, Chen F. Analysis of the microbiota of black stain in the primary dentition. PLoS One 2015;10(9):e0137030. Available at: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0137030
- 17.de Baat C, Zweers PGMA, van Loveren C, Vissink A. Medicaments and oral healthcare 5. Adverse effects of medications and over-the-counter drugs on teeth. [In Dutch]. Ned Tijdschr Tandheelkd 2017;124(10):485-91. doi:10.5177/ntvt.2017.10.17142.
- 18.Escartin JL, Arnedo A, Pinto V, Vela MJ. A study of dental staining among competitive swimmers. Community Dent Oral Epidemiol 2000;28(1):10-7.
- 19.Scheper WA, van Nieuw Amerongen A, Eijkman MA. Oral conditions in swimmers. [Article in Dutch] Ned Tijdschr Tandheelkd 2005;112(4):147-8.
- 20.Lobene R, Hefferren J, and Dentifrice Function Committee. Clinical response of non-abrasive dentifrice use in dental hygienists. J Dent Res 1996;75:88.
- 21.American Dental Association. Oral Health Topics. Toothpaste. Center for Scientific Information, ADA Science Institute. Updated August 2018. Available at: https://www.ada.org/en/member-center/oral-health-topics/toothpastes.
- 22.Soeteman GD, Valkenburg C, Van der Weijden GA, Van Loveren C, Bakker E, Slot DE. Whitening dentifrice and tooth surface discoloration-a systematic review and meta-analysis Int J Dent Hyg. 2018 Feb;16(1):24-35.
- 23.Kakar A, Rustogi K, Zhang YP, Petrone ME, DeVizio W, Proskin HM. A clinical investigation of the tooth whitening efficacy of a new hydrogen peroxide-containing dentifrice J Clin Dent. 2004;15(2):41-5.
- 24.Ghassemi A, Hooper W, Vorwerk L, Domke T, DeSciscio P, Nathoo S. Effectiveness of a new dentifrice with baking soda and peroxide in removing extrinsic stain and whitening teeth J Clin Dent. 2012;23(3):86-91.
- 25.Isaacs RL, Bartizek RD, Owens TS, Walters PA, Gerlach RW. Maintenance of tooth color after prophylaxis: comparison of three dentifrices. J Clin Dent 2001;12(2):51-5.
- 26.Maanen-Schakel NWD van, Slot DE, Bakker EWP, Weijden GA van der. The effect of an oxygenating agent on chlorhexidine-induced extrinsic tooth staining: a systematic review. Int J Dent Hyg 2012;10:198-208.
- 27.Milleman JL, He T, Anastasia MK. Anti-calculus efficacy of a SnF2 dentifrice in a three-month clinical. J Dent Res 2017;96(spec iss A):Abstract 2816.
- 28.Myers CP, Pappas I, Makwana E, Begum-Gafur R, Utgikar N, Alsina MA, Fitzgerald M, Trivedi HM, Gaillard J-F, Masters JG, Sullivan RJ. Solving the problem with stannous fluoride: Formulation, stabilization, and antimicrobial action. J Am Dent Assoc 2019;150)4S):S5-S13.
- 29.Sensabaugh C, Sagel ME. Stannous fluoride dentifrice with sodium hexametaphosphate: review of laboratory, clinical and practice-based data. J Dent Hyg 2009;83(2):70-8.
- 30.Milleman KR, Creeth JE, Burnett GR, Milleman JL. A randomized clinical trial to evaluate the stain removal efficacy of a sodium phytate dentifrice formulation. J Esthet Rest Dent 2018;30(2):E45-51.
- 31.Sanchez AR, Rogers RS III, Sheridan PJ. Tetracycline and other tetracycline-derivative staining of the teeth and oral cavity. Int J Dermatol 2004;43:709-15.
- 32.Tredwin C, Scully C, Bagan-Sebastian J-V. Drug-induced dental disorders. Adverse Drug Reaction Bull 2005;232. ISSN 0044-6394.
- 33.Love RM, Chandler NP. A scanning electron and confocal laser microscope investigation of tetracycline-affected human dentine. Int Endod J 1996;29(6):376-81.
- 34.Agrawal P, Singh O, Nigam AK, Upadhyay S. Imatinib-induced dental hyperpigmentation in chronic myeloid leukemia in an adult female. Indian J Pharmacol 2015;47(6):685-6.
- 35.Pendrys DG, Katz RV, Morse DE. Risk factors for enamel fluorosis in a nonfluoridated population. Am J Epidemiol 1996;143(8):808-15.
- 36.Fejerskov O, Manji F, Baelum V. The nature and mechanisms of dental fluorosis in man. J Dent Res 1990;69(special issue):692-700.
- 37.Bittencourt do Valle I, Eduardo VM, Goese TB, Oliviera ZFL, von Zeidler SV. Green teeth in the primary and permanent dentition. J Pediatr 2017;191:275.
- 38.Kahler B, Rossi-Fedele G. A review of tooth discoloration after regenerative endodontic therapy. J Endod 2016;42(4):563-9.
- 39.Ten Bosch JJ, Coops CC. Tooth color and reflectance as related to light scattering and enamel hardness. J Dent Res 1995;74:374-80.



