Integrating the 4Ps into Patient Care
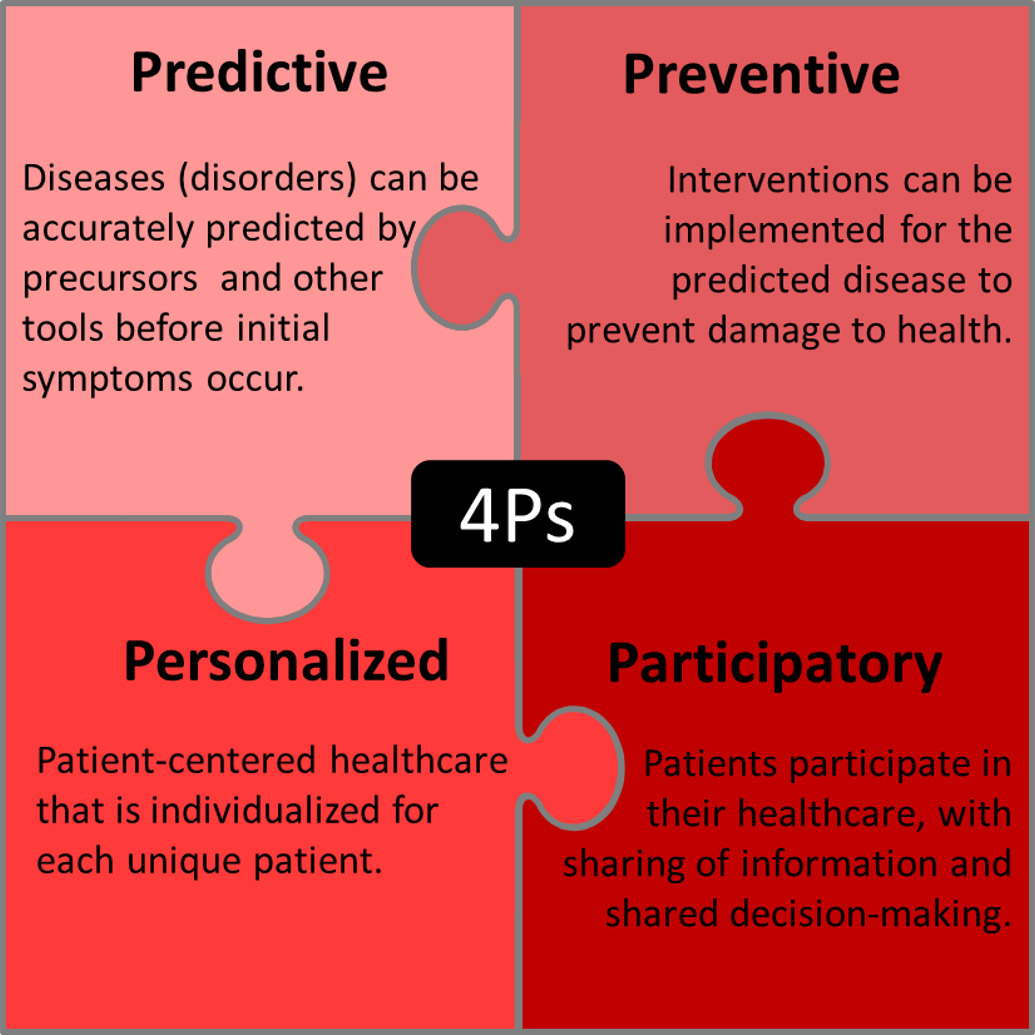
The 4Ps in medicine, also known as P4 medicine, was introduced approximately 16 years ago.1Hood L. Systems biology: integrating technology, biology, and computation. Mech Ageing Dev 2003;124:9-16. This systems biology approach to health and disease integrates lifestyle and environmental factors, biology, biomarkers and ‘omics’ technologies, and clinical data.2Hood L, Flores M. A personal view on systems medicine and the emergence of proactive P4 medicine: predictive, preventive, personalized and participatory. N Biotechnol 2012;29(6):613-24.,3Cesario A, Auffray C, Russo P, Hood L. P4 medicine needs P4 education. Curr Pharmaceut De 2014;20,000-000. ‘Omic’ technologies include but are not limited to genomics, epigenomics, transcriptomics, proteomics and metabolomics.3Cesario A, Auffray C, Russo P, Hood L. P4 medicine needs P4 education. Curr Pharmaceut De 2014;20,000-000.,4Hood L. Systems biology and p4 medicine: past, present, and future. Rambam Maimonides Med J 2013;4(2):e0012.,5Liebsch C, Pitchika V, Pink C, Samietz S, Kastenmüller G, Artati A, Suhre K, Adamski J, Nauck M, Völzke H, Friedrich N, Kocher T, Holtfreter B, Pietzner M. The Saliva Metabolome in Association to Oral Health Status. J Dent Res 2019;98(6):642-651. doi: 10.1177/0022034519842853. The 4Ps represent ‘Predictive’, ‘Preventive’, ‘Personalized’ and ‘Participatory.’6Pulciani S, Di Lonardo A, Fagnani C, Taruscio D. P4 medicine versus Hippocrates. Ann Ist Super Sanita 2017;53(3):185-91. (Figure 1) ‘Predictive’ and ‘preventive’ refer to the ability to predict and prevent disease, while ‘personalized’ refers to patient-centered healthcare that is individualized for each unique patient. Participatory refers to patient participation in the care of their health together with healthcare personnel, sharing of information and shared decision-making.
Together, the 4Ps represent an integrative, pro-active approach to healthcare.7Sagner M, McNeil A, Puskac P, Auffray C, Price ND, Hood L, et al. The P4 health spectrum – A predictive, preventive, personalized and participatory continuum for promoting healthspan. Prog Cardiovasc Dis 2017;59(5):506-21.,8Louis R, Roche N. Personalised medicine: are we ready? Eur Respir Rev 2017;26:170088. https://doi.org/10.1183/16000617.0088-2017. P4 medicine has mainly focused on chronic non-communicable diseases which represent the greatest health burden globally.3Cesario A, Auffray C, Russo P, Hood L. P4 medicine needs P4 education. Curr Pharmaceut De 2014;20,000-000.,8Louis R, Roche N. Personalised medicine: are we ready? Eur Respir Rev 2017;26:170088. https://doi.org/10.1183/16000617.0088-2017.,9Bousquet J, Anto JM, Sterk PJ, Adcock IM, Chung KF, Roca J, et al. Systems medicine and integrated care to combat chronic noncommunicable diseases. Genome Med 2011;3(7):43. However, this approach is also being applied to inherited disorders and other diseases.10van Karnebeek CDM, Wortmann SB, Tarailo-Graovac M, Langeveld M, Ferreira CR, van de Kamp JM, et al. The role of the clinician in the multi-omics era: are you ready? J Inherited Metabolic Dis 2018;41:571-82.
P4 Dentistry
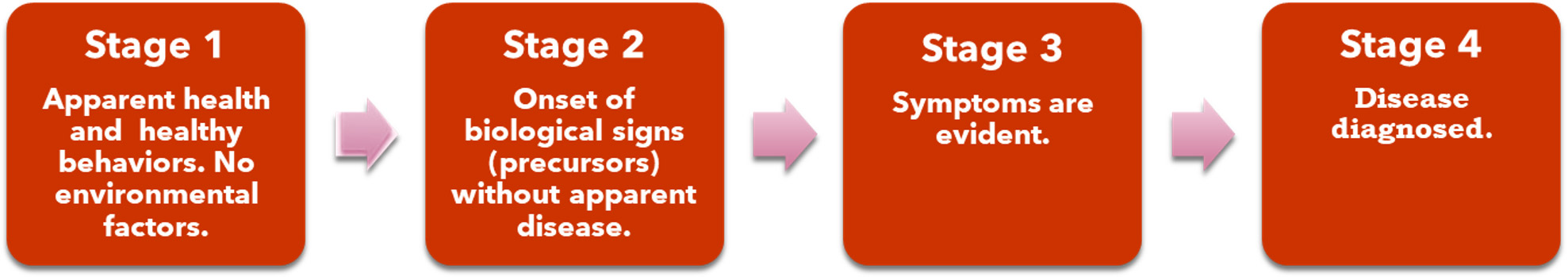
A systems biology approach can benefit oral and systemic health. Four stages have been described for the health-disease continuum 7Sagner M, McNeil A, Puskac P, Auffray C, Price ND, Hood L, et al. The P4 health spectrum – A predictive, preventive, personalized and participatory continuum for promoting healthspan. Prog Cardiovasc Dis 2017;59(5):506-21.,8Louis R, Roche N. Personalised medicine: are we ready? Eur Respir Rev 2017;26:170088. https://doi.org/10.1183/16000617.0088-2017. (Figure 2). Stage A represents apparent health along with healthy behaviors and no environmental factors; stage B represents the onset of disease precursors without apparent disease, stage C ensues when symptoms are evident and Stage D exists when a diagnosis has occurred.7Sagner M, McNeil A, Puskac P, Auffray C, Price ND, Hood L, et al. The P4 health spectrum – A predictive, preventive, personalized and participatory continuum for promoting healthspan. Prog Cardiovasc Dis 2017;59(5):506-21.,8Louis R, Roche N. Personalised medicine: are we ready? Eur Respir Rev 2017;26:170088. https://doi.org/10.1183/16000617.0088-2017. If disease can be accurately predicted at the patient level, targeted interventions to prevent the disease from occurring become possible rather than reactively treating its manifestations.7Sagner M, McNeil A, Puskac P, Auffray C, Price ND, Hood L, et al. The P4 health spectrum – A predictive, preventive, personalized and participatory continuum for promoting healthspan. Prog Cardiovasc Dis 2017;59(5):506-21. Personalized care and patient participation are also essential for this approach to succeed.
Figure 2. Stages for health-disease
Prediction and Prevention in P4 Dentistry
Individual elements related to the 4Ps already exist in dentistry. For example, the use of risk assessment tools for periodontal disease, dental caries and oral cancer are intended to predict risk and provide guidance on the type and level of preventive care required to prevent disease. Evidence supports the use of validated electronic periodontal risk assessment tools.11Lang NP, Suvan JE, Tonetti MS. Risk factor assessment tools for the prevention of periodontitis progression a systematic review. J Clin Periodontol 2015;42(S16):S59-70. A wide range of research is now being conducted using biomarkers and non-invasive tests.12Bartold PM. Lifestyle and periodontitis: The emergence of personalized periodontics. Periodontol 2000 2018;78(1):7-11.
Predictive screening tests being developed include biomarkers in saliva, gingival crevicular fluid (GCF) and blood. Antibodies have been found that may be predictive for Sjӧgren’s syndrome (SS) and its severity, and can be detected up to 20 years prior to patients receiving a diagnosis of SS.13Theander E, Jonsson R, Sjöström B, et al. Prediction of Sjögrens Syndrome years before diagnosis and identification of patients with early onset and severe disease course by autoantibody profiling. Arthritis Rheumatol 2015;67(9):2427-36. While SS cannot at the current time be prevented or cured, this biomarker would predict it and promote pre-emptive education and personalized care such that, for example, the increased risk of dental caries as a sequelae of SS could be managed and oral disease prevented. In the future, it can be hoped that a method of preventing the primary condition could be found that could be applied following predictive tests. Another example is chairside testing for hemoglobin A1c (HbA1c) using gingival crevicular blood as a patient-friendly and accessible method of screening for diabetes mellitus.14Rosedale MT, Strauss SM. Diabetes screening at the periodontal visit: Patient and provider experiences with two screening approaches. Int J Dent Hyg 2012;10(4):250-8. Patients also reported that they learned more about their overall health and risk for diabetes associated with periodontal disease.
‘Inflammaging’ refers to low-grade chronic inflammation that is now known to be part of the aging process.15Franceschi C, Campisi J. Chronic Inflammation (Inflammaging) and Its Potential Contribution to Age-Associated Diseases. J Gerontol 2014 Series A;69 (Suppl 1):S4-S9. https://doi.org/10.1093/gerona/glu057 In addition, chronic systemic inflammation from various sources increases risk for Type 2 diabetes mellitus and cardiovascular disease.16Dregan A, Charlton J, Chowienczyk P, Gulliford MC. Chronic inflammatory disorders and risk of type 2 diabetes mellitus, coronary heart disease, and stroke: a population-based cohort study. Circulation 2014;130(10):837-44. doi: 10.1161/CIRCULATIONAHA.114.009990. Biomarkers associated with ‘inflammaging’ include elevated levels of interleukin-6 (IL-6), C-reactive protein (CRP) and other pro-inflammatory biomarkers.15Franceschi C, Campisi J. Chronic Inflammation (Inflammaging) and Its Potential Contribution to Age-Associated Diseases. J Gerontol 2014 Series A;69 (Suppl 1):S4-S9. https://doi.org/10.1093/gerona/glu057 Similarly, IL-6, CRP, IL-1β, MMP-8 and other biomarkers, alone and in combination, are being researched as biomarkers for periodontitis and its severity.17González-Ramírez J, Serafín-Higuera N, Mancilla MCS, Martínez-Coronilla G, Famanía-Bustamante J, López ALL. Use of Biomarkers for the Diagnosis of Periodontitis. InTech Open, March 25, 2019. doi: 10.5772/intechopen.85394,18Korte DL, Kinney J. Personalized medicine: an update of salivary biomarkers for periodontal diseases. Periodontol 2000 2016;70:26-37. In metabolomic research, it has been found that salivary metabolites change with oral health status and aging.5Liebsch C, Pitchika V, Pink C, Samietz S, Kastenmüller G, Artati A, Suhre K, Adamski J, Nauck M, Völzke H, Friedrich N, Kocher T, Holtfreter B, Pietzner M. The Saliva Metabolome in Association to Oral Health Status. J Dent Res 2019;98(6):642-651. doi: 10.1177/0022034519842853. In particular, the bacterial metabolite phenylacetate is regarded as promising as a biomarker given its association with periodontitis.5Liebsch C, Pitchika V, Pink C, Samietz S, Kastenmüller G, Artati A, Suhre K, Adamski J, Nauck M, Völzke H, Friedrich N, Kocher T, Holtfreter B, Pietzner M. The Saliva Metabolome in Association to Oral Health Status. J Dent Res 2019;98(6):642-651. doi: 10.1177/0022034519842853. At the current time, research is ongoing to find a robust biomarker, or a combination of biomarkers, predictive for periodontal disease and its severity. Other advances can personalize treatment and chemotherapeutics. If found, together these would represent a true paradigm shift and promote 4P-based prevention and treatment.
Patient Participation and Personalized Care
Patient-centered (personalized) care has been defined as care ‘provided in a respectful manner, assures open and ongoing sharing of useful information in an ongoing manner and supports and encourages the participation of patients and their families.19Newell S, Jordan Z. The patient experience of patient-centered communication with nurses in the hospital setting: a qualitative systematic review protocol. JBI Database System Rev Implement Rep 2015;13(1):76-87. doi: 10.11124/jbisrir-2015-1072. Patient participation involves shared decision-making with the patient’s provider, active involvement and self-care.20Truglio-Londrigan M, Slyer JT, Singleton JK, Worral P. A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. JBI Libr Syst Rev 2012;10(58):4633-46. Recommendations for shared decision-making include a number of steps.21Thériault G, Bell NR, Grad R, Singh H, Szafran O. Teaching shared decision making: An essential competency. Canadian Family Physician 2019;65:514-6. Once it has been agreed a decision needs to be made, it is recommended that options and alternatives should be provided in an unbiased manner along with decision aids as necessary. Potential risk and benefits should be described, and quantified using numbers rather than percentages. Following this, it is recommended that patient preferences be discussed, the outcomes of different options, and more information provided on specific aspects of the decision-making. (Figure 3)
Patients in one study defined non-participation as interactions that were not patient-centered.22Catrine A, Ekman I, Ehnfors M. Considering patient non-participation in health care. Health Expectations 2008;11:263-71. This meant not being listened to, the absence of recognition of their individual needs, and information that was either received but not understood or not provided. A patient’s ability to participate and share in decision making also varies with age, socio-economic status, education and culture.20Truglio-Londrigan M, Slyer JT, Singleton JK, Worral P. A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. JBI Libr Syst Rev 2012;10(58):4633-46. In addition, provider understanding of patients’ levels of health literacy is essential.7Sagner M, McNeil A, Puskac P, Auffray C, Price ND, Hood L, et al. The P4 health spectrum – A predictive, preventive, personalized and participatory continuum for promoting healthspan. Prog Cardiovasc Dis 2017;59(5):506-21. Patient participation is promoted when information is individualized and the patient’s knowledge is recognized, and when patient decision-making involves knowledge and needs.23Eldh AC, Ekman I, Ehnfors M. Conditions for patient participation and non-participation in health care. Nurs Ethics 2006;13(5):503-14. Effective communication between patient and provider is essential for patient participation and personalized care.
Communication and Integrating the 4Ps
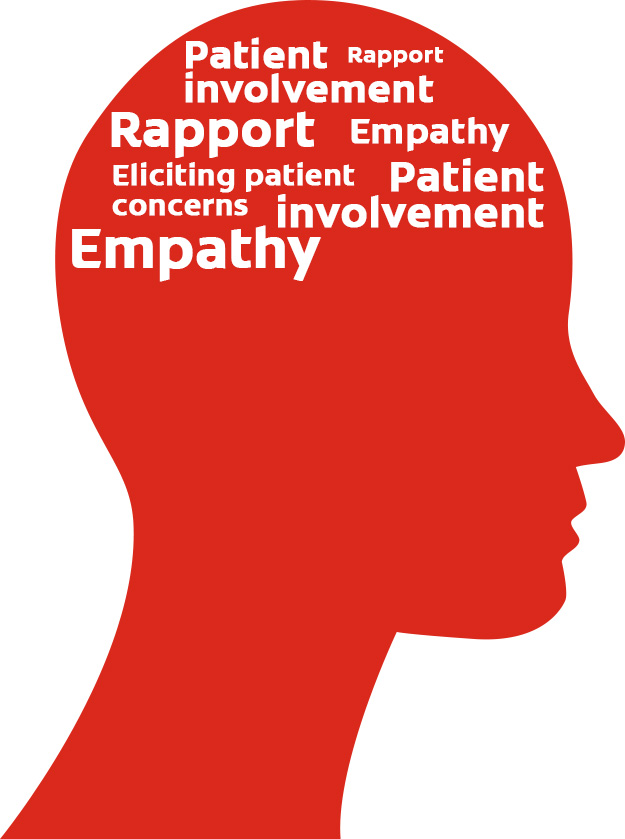
Patient-centered communication has been defined as ‘communication that invites and encourages the patient to participate and negotiate in decision-making regarding their own care’.19Newell S, Jordan Z. The patient experience of patient-centered communication with nurses in the hospital setting: a qualitative systematic review protocol. JBI Database System Rev Implement Rep 2015;13(1):76-87. doi: 10.11124/jbisrir-2015-1072. In a recent systematic review, it was found that establishing rapport, eliciting patient concerns, demonstrating empathy and involvement in their treatment plans are regarded by patients as important for effective patient-centered communication. (Figure 4) Goals within ‘Healthy People 2020’ include increasing the percentage of healthcare providers noted by patients to always listen to them, provide understandable information and to have satisfactory communication skills.24U.S. Department of Health and Human Services. 2011. Healthy People.gov: http://www.healthypeople.gov/2020/default.aspx
According to the Department of Health and Human Services, approximately 9 in 10 adults are not proficient at using everyday health information.25U.S. Department of Health and Human Services. National Action Plan to Improve Health Literacy. Available at: https://health.gov/communication/hlactionplan/pdf/Health_Literacy_Action_Plan.pdf. In order to communicate effectively, the use of plain language, teach-back, patient-friendly methods and visual aids is recommended.26Podschun G. 5 Oral Health Literacy Programs.” Institute of Medicine. 2013. Oral Health Literacy: Workshop Summary. Washington, DC: The National Academies Press. doi: 10.17226/13484.,27Buerlein JK, Horowitz AM, Child WL. Perspectives of Maryland women regarding oral health during pregnancy and early childhood. J Public Health Dent 2011;71(2):131-5.,28U.S. Department of Health and Human Services. Quick Guide to Health Literacy. Fact Sheet. Available at: https://health.gov/communication/literacy/quickguide/factsbasic.htm#seven. Plain language includes but is not limited to providing key information first or alone to improve understanding, breaking down complex information, and using simple language.29Sheridan SL, Halpern DJ, Viera AJ, Berkman ND, Donahue KE, Crotty K. Interventions for individuals with low health literacy: a systematic review. J Health Commun 2011;16 Suppl 3:30-54. Use of visual and verbal tools including adding icons helps to improve patients’ understanding of numerical data. Visual aids that improve learning and knowledge include supplemental videos, DVDs, models, computer-based and graphics-based information.29Sheridan SL, Halpern DJ, Viera AJ, Berkman ND, Donahue KE, Crotty K. Interventions for individuals with low health literacy: a systematic review. J Health Commun 2011;16 Suppl 3:30-54.,30Strömberg A, Dahlström U, Fridlund B. Computer-based education for patients with chronic heart failure. A randomised, controlled, multicentre trial of the effects on knowledge, compliance and quality of life. Patient Educ Couns 2006;64(1-3):128-35. This has also been shown to help mitigate differences in literacy and educational materials, and to improve home self-care and disease prevention (in this case, dental caries).31Albert NM, Buchsbaum R, Li J. Randomized study of the effect of video education on heart failure healthcare utilization, symptoms, and self-care behaviors. Patient Educ Couns 2007;69(1-3):129-39.,32Davis TC, Mayeaux EJ, Fredrickson D, Bocchini JA Jr, Jackson RH, Murphy PW. Reading ability of parents compared with reading level of pediatric patient education materials. Pediatrics 1994;93(3):460-8.,33Newitter DA, Meiers JC, Kazemi RB. Rx for caries prevention: time line for home care. A software aid for communication of patient instructions for management of dental caries. Oper Dent 2002;27(2):204-7.
Further, patients must understand risk in order to participate in prevention. However, risk is ill-understood, including among well-educated individuals.34Gigerenzer G, Gaissmaier W, Kurz-Milcke E, Schwartz LM, Woloshin S. Helping doctors and patients make sense of health statistics. Psychological science in the public interest. J Am Psych Society 2007;8(2):53-96. Risk, relative risk levels and basic statistical information are problematic concepts.34Gigerenzer G, Gaissmaier W, Kurz-Milcke E, Schwartz LM, Woloshin S. Helping doctors and patients make sense of health statistics. Psychological science in the public interest. J Am Psych Society 2007;8(2):53-96.,35Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making 2001;21(1):37-44. One method recommended to help overcome poor statistical literacy is to use an absolute number, such as 3 in 100 instead of stating ‘a 3% chance.’21Thériault G, Bell NR, Grad R, Singh H, Szafran O. Teaching shared decision making: An essential competency. Canadian Family Physician 2019;65:514-6. Graphic presentations of risk, as used in risk assessment tools, also help to educate patients and improve care. Personalized web pages for patients with individualized education can also be provided.36Yeh YT, Chiu YT, Liu CT, Wu SJ, Lee TI. Development and evaluation of an integrated patient-oriented education management system for diabetes. Stud Health Technol Inform 2006;122:172-5.
Communication style influences its effectiveness and how patients perceive communication and providers. In one study with pediatric dentists, discussions that were empathetic, reassuring and provided positive reinforcement lead to patient perceptions that care was more patient-centered and resulted in greater patient-provider interaction.37Wong HM, Bridges SM, McGrath CP, Yiu CKY, Zayts OA, Au TKF. Impact of prominent themes in clinician-patient conversations on caregiver’s perceived quality of communication with paediatric dental visits. PLoS ONE 2017;12(1):e0169059. In contrast, conversations focused on procedures did not have this effect. Differences in content recall suggest a mismatch between dentists and patients.38Misra S, Daly B, Dunne S, Millar B, Packer M, Asimakopoulou K. Dentist–patient communication: what do patients and dentists remember following a consultation? Implications for patient compliance. Patient Preference and Adherence 2013:7:543-9. Patients recall less information on oral health than dentists recall providing. Studies have reported that patients did not recall information on home care and post-operative instructions.38Misra S, Daly B, Dunne S, Millar B, Packer M, Asimakopoulou K. Dentist–patient communication: what do patients and dentists remember following a consultation? Implications for patient compliance. Patient Preference and Adherence 2013:7:543-9.,39Blinder D, Rotenberg L, Peleg M, Taicher S. Patient compliance to instructions after oral surgical procedures. Int J Oral Maxillofac Surg 2001;30(3):216-9. Knowledge level influences recall, further highlighting the need for training and education, and improved oral health literacy.38Misra S, Daly B, Dunne S, Millar B, Packer M, Asimakopoulou K. Dentist–patient communication: what do patients and dentists remember following a consultation? Implications for patient compliance. Patient Preference and Adherence 2013:7:543-9.
‘There’s an app for that’ is increasingly the case, and an opportunity for oral health education. Apps are available for patient and direct-to-consumer education; as tobacco cessation aids; and for tracking of, and information on, habits and oral hygiene. However, a recent study found that educational opportunities were missed, some apps focused on cosmetic issues while omitting related health information, and usability issues were found.40Tiffany B, Blasi P, Catz SL, McClure JB. Mobile apps for oral health promotion: Content review and heuristic usability analysis. JMIR Mhealth Uhealth 2018;6:e11432. Further, few apps included gain-framed messaging, thereby missing an opportunity to frame behavior change for a positive outcome.
Training
Competencies in interpersonal and communication skills are embodied in the Commission on Dental Accreditation’s standards for Dental and Dental Hygiene programs.41Commission on Dental Accreditation. Accreditation standards for dental education programs. Chicago: 2010. Healthcare providers exhibit a more patient-centered approach if they have received communications training.42Mull, Carrie, “Implementation of a Patient-Centered Communication Model in the Emergency Department” (2017). Doctoral Projects. https://scholarworks.gvsu.edu/kcon_doctoralprojects/46 Effective options for training include all-day or multi-day training, simulated patient encounters, role playing, taping and analyses of interactions. Such encounters can be live simulations or computer-based.42Mull, Carrie, “Implementation of a Patient-Centered Communication Model in the Emergency Department” (2017). Doctoral Projects. https://scholarworks.gvsu.edu/kcon_doctoralprojects/46 In a recent study, pre-clinical dental students participated in interactive communication training that included videoing and analyses of exercises and role playing.43Alvarez S, Schultz J-H. A communication-focused curriculum for dental students – an experiential training approach. BMC Medical Education 2018;18:55. https://doi.org/10.1186/s12909-018-1174-6 Students reported the course to be effective and important. Topics addressed included active listening, taking medical histories, simulated patient-provider interactions, learning about empathy and sympathy, non-verbal communication, self-awareness and self-perception. Further, increased recognition of the importance of patient communication and interaction for optimal health and healthcare has led to an increased focus on communication skills.43Alvarez S, Schultz J-H. A communication-focused curriculum for dental students – an experiential training approach. BMC Medical Education 2018;18:55. https://doi.org/10.1186/s12909-018-1174-6
Conclusions
Using a systems biology approach, diseases and disorders may be predicted and prevented using patient-level information and biomarkers. This approach can also be used to individualize and optimize treatment. More research is required to identify robust biomarkers, to fully understand disease/disorder processes and the most effective prevention regimens and treatments. Digital technologies can play a role and be further developed to offer opportunities for information-gathering, research and data interpretation, and P4-based proactive healthcare. Further, the ability to communicate effectively with patients, and education for oral health literacy, are integral to personalized care and patient participation, and therefore to P4 dentistry overall. In conclusion, integrating the 4Ps into patient care holds promise for improving and optimizing oral and systemic health.
References
- 1.Zimmerli B, Jeger F, Lussi A. Bleaching of nonvital teeth. A clinically relevant literature review. Schweiz Monatsschr Zahnmed 2010;120(4):306-20.
- 2.Brunton PA, Burke FJT, Sharif MO et al. Contemporary dental practice in the UK in 2008: Aspects of direct restorations, endodontics, and bleaching. Br Dent J 2012;212:63-7.
- 3.Demarco FF, Conde MCM, Ely C et al. Preferences on vital and nonvital tooth bleaching: A survey among dentists from a city of Southern Brazil. Braz Dent J 2013;24:527-31.
- 4.Kahler B. Present status and future directions – Managing discoloured teeth. Int Endod J 2022: Feb 21. doi: 10.1111/iej.13711.
- 5.Nutting EB, Poe GS. Chemical bleaching of discolored endodontically treated teeth. Dent Clin N Am 1967;11:655-62.
- 6.Pallarés-Serrano A, Pallarés-Serrano S, Pallarés-Serrano A, Pallarés-Sabater A. Assessment of Oxygen Expansion during Internal Bleaching with Enamel and Dentin: A Comparative In Vitro Study. Dent J 2021;9:98. https://doi.org/10.3390/dj9090098.
- 7.Estay J, Angel P, Bersezio C et al. The change of teeth color, whiteness variations and its psychosocial and self-perception effects when using low vs. high concentration bleaching gels: a one-year follow-up. BMC Oral Health 2020;20(1):255. doi: 10.1186/s12903-020-01244-x.
- 8.Haywood VB, Bergeron BE. Bleaching and the Diagnosis of Internal Resorption. Jul 24, 2018. https://decisionsindentistry.com/article/bleaching-and-the-diagnosis-of-internal-resorption/
- 9.Abbott P, Heah SY. Internal bleaching of teeth: an analysis of 255 teeth. Aust Dent J 2009;54(4):326-33. https://onlinelibrary.wiley.com/doi/epdf/10.1111/j.1834-7819.2009.01158.x.
- 10.Sakalli B, Basmaci F, Dalmizrak O. Evaluation of the penetration of intracoronal bleaching agents into the cervical region using different intraorifice barriers. BMC Oral Health 2022;22(1):266. doi: 10.1186/s12903-022-02300-4.
- 11.American Association of Endodontists Clinical Practice Committee. Use of Silver Points. AAE Position Statement. https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/silverpointsstatement.pdf#:~:text=Silver%20points%20have%20been%20shown%20to%20corrode%20spontaneously,retreatment%20and%20replacement%20of%20the%20points%20with%20another.
- 12.Savadkouhi ST, Fazlyab M. Discoloration Potential of Endodontic Sealers: A Brief Review. Iran Endod J 2016;11(4):250-4. doi: 10.22037/iej.2016.20.
- 13.Ahmed HM, Abbott PV. Discolouration potential of endodontic procedures and materials: a review. Int Endod J 2012;45(10):883-97. doi: 10.1111/j.1365-2591.2012.02071.x.
- 14.Krastl G, Allgayer N, Lenherr P et al. Tooth discoloration induced by endodontic materials: a literature review. Dent Traumatol 2013;29(1):2-7. doi: 10.1111/j.1600-9657.2012.01141.x.
- 15.Ioannidis K, Mistakidis I, Beltes P, Karagiannis V. Spectrophotometric analysis of crown discoloration induced by MTA- and ZnOE-based sealers. J Appl Oral Sci 2013;21(2):138-44. doi: 10.1590/1678-7757201302254.
- 16.Santos LGPD, Chisini LA, Springmann CG et al. Alternative to Avoid Tooth Discoloration after Regenerative Endodontic Procedure: A Systematic Review. Braz Dent J 2018;29(5):409-18. doi: 10.1590/0103-6440201802132.
- 17.Watts A, Addy M. Tooth discoloration and staining: a review of the literature. Br Dent J 2001;190:309-16.
- 18.Pink tooth of Mummery. https://medical-dictionary.thefreedictionary.com/Pink+Tooth+of+Mummery.
- 19.Haywood VB. History, safety, and effectiveness of current bleaching techniques and applications of the nightguard vital bleaching technique. Quintessence Int 1992:23:471-88. http://www.quintpub.com/userhome/qi/qi_23_7_haywood_6.pdf
- 20.Bersezio C, Ledezma P, Mayer C et al. Effectiveness and effect of non-vital bleaching on the quality of life of patients up to 6 months post-treatment: a randomized clinical trial. Clin Oral Investig 2018;22(9):3013-9. doi: 10.1007/s00784-018-2389-y.
- 21.Popescu AD, Purcarea MV, Georgescu RV et al. Vital and Non-Vital Tooth Bleaching Procedures: A Survey Among Dentists From Romania. Rom J Oral Rehab 2021;13(3):59-71. https://www.rjor.ro/wp-content/uploads/2021/10/VITAL-AND-NON-VITAL-TOOTH-BLEACHING-PROCEDURES-A-SURVEY-AMONG-DENTISTS-FROM-ROMANIA.pdf.
- 22.Zarean P, Zarean P, Ravaghi A et al. Comparison of MTA, CEM Cement, and Biodentine as Coronal Plug during Internal Bleaching: An In Vitro Study. Int J Dent 2020;2020:8896740. doi: 10.1155/2020/8896740.
- 23.Canoglu E, Gulsahi K, Sahin C et al. Effect of bleaching agents on sealing properties of different intraorifice barriers and root filling materials. Med Oral Patol Oral Cir Bucal 2012;17 (4):e710-5. http://www.medicinaoral.com/medoralfree01/v17i4/medoralv17i4p710.pdf
- 24.Amato A, Caggiano M, Pantaleo G, Amato M. In-office and walking bleach dental treatments on endodontically-treated teeth: 25 years follow-up. Minerva Stomatol 2018;67(6):225-30.
- 25.Lim MY, Lum SOY, Poh RSC et al. An in vitro comparison of the bleaching efficacy of 35% carbamide peroxide with established intracoronal bleaching agents. Int Endod J 2004;37(7):483-8. doi: 10.1111/j.1365-2591.2004.00829.x.
- 26.Yui KCK, Rodrigues JR, Mancini MNG et al. Ex vivo evaluation of the effectiveness of bleaching agents on the shade alteration of blood-stained teeth. Int Endod J 2008;41(6):485-92. doi: 10.1111/j.1365-2591.2008.01379.x.
- 27.Warren MA, Wong M, Ingram TA III. An in vitro comparison of bleaching agents on the crowns and roots of discolored teeth. J Endod 1990;16:463-7.
- 28.Rotstein I, Mor C, Friedman S. Prognosis of intracoronal bleaching with sodium perborate preparations in vitro: 1-year study. J Endod 1993;19:10-2.
- 29.Weiger R, Kuhn A, Lost C. In vitro comparison of various types of sodium perborate used for intracoronal bleaching of discolored teeth. J Endod 1994;20:338-41.
- 30.Amato M, Scaravilli MS, Farella M, Riccitiello F. Bleaching teeth treated endodontically: long-term evaluation of a case series. J Endod 2006;32:376-8.
- 31.Abou-Rass M. Long-term prognosis of intentional endodontics and internal bleaching of tetracycline-stained teeth. Compend Contin Educ Dent 1998;19:1034-44.
- 32.Anitua E, Zabalegui B, Gil J, Gascon F. Internal bleaching of severe tetracycline discolorations: four-year clinical evaluation. Quintessence Int 1990;21(10):783-8.
- 33.Gorr S-U, Brigman HV, Anderson JC, Hirsch EB. The antimicrobial peptide DGL13K is active against drug-resistant gram-negative bacteria and sub-inhibitory concentrations stimulate bacterial growth without causing resistance. PLoS ONE 2022;17(8): e0273504. https://doi.org/10.1371/journal.pone.0273504.
- 34.Peters SM, Hill NB, Halepas S. Oral manifestations of monkeypox: A report of two cases Journal of Oral and Maxillofacial Surgery (2022). https://doi.org/10.1016/j.joms.2022.07.147.
- 35.Portalatin A. Infectious disease experts call on dentists to monitor monkeypox symptoms: 6 notes. August 15, 2022. https://www.beckersdental.com/clinical-leadership-infection-control/39124-infectious-disease-experts-call-on-dentists-to-monitor-monkeypox-symptoms-6-notes.html?origin=DentalE&utm_source=DentalE&utm_medium=email&utm_content=newsletter&oly_enc_id=1694C1316967A3F.
- 36.CDC. Monkeypox. Non-Variola Orthopoxvirus and Monkeypox Virus Laboratory Testing Data. August 17, 2022. https://www.cdc.gov/poxvirus/monkeypox/response/2022/2022-lab-test.html.
- 37.CDC. Monkeypox. Prevention. https://www.cdc.gov/poxvirus/monkeypox/prevention.html.
- 38.CDC. Monkeypox and smallpox vaccine guidance. Updated June 2, 2022. https://www.cdc.gov/poxvirus/monkeypox/clinicians/index.htm.
- 39.CDC. Monkeypox. ACAM Vaccine. https://www.cdc.gov/poxvirus/monkeypox/interim-considerations/acam2000-vaccine.html.
- 40.CDC. Guidelines for Infection Control in Dental Health-Care Settings — 2003. https://www.cdc.gov/mmwr/PDF/rr/rr5217.pdf.
- 41.CDC. Infection Prevention and Control of Monkeypox in Healthcare Settings. Updated August 11, 2022. https://www.cdc.gov/poxvirus/monkeypox/clinicians/infection-control-healthcare.html
- 42.CDC. Monkeypox. Information For Veterinarians. https://www.cdc.gov/poxvirus/monkeypox/veterinarian/index.html.
- 43.CDC. Monkeypox. Pets in the Home. https://www.cdc.gov/poxvirus/monkeypox/prevention/pets-in-homes.html.
- 44.Cheng YL, Musonda J, Cheng H, et al. Effect of surface removal following bleaching on the bond strength of enamel. BMC Oral Health 2019;19(1):50.
- 45.Monteiro D, Moreira A, Cornacchia T, Magalhães C. Evaluation of the effect of different enamel surface treatments and waiting times on the staining prevention after bleaching. J Clin Exp Dent 2017;9(5):e677-81.
- 46.Rezende M, Kapuchczinski AC, Vochikovski L, et al. Staining power of natural and artificial dyes after at-home dental bleaching. J Contemp Dent Pract 2019;20(4):424-7.


:sharpen(level=0):output(format=jpeg)/up/2023/05/Fiona-Collins-thumbnail-1-3.jpg)
:sharpen(level=0):output(format=jpeg)/up/2019/11/Integrating-the-4Ps-into-Patient-Care-2.jpg)