Integrating the 4Ps into Patient Care
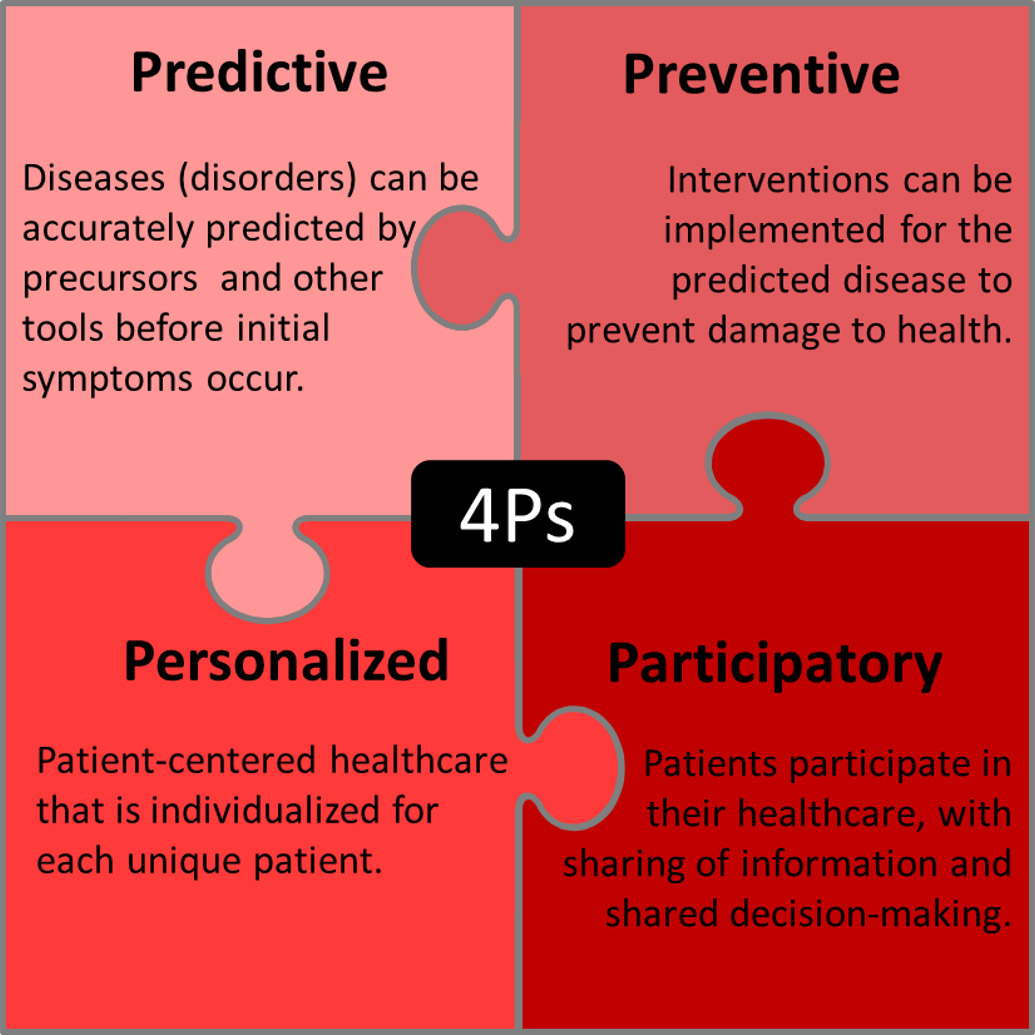
The 4Ps in medicine, also known as P4 medicine, was introduced approximately 16 years ago.1Hood L. Systems biology: integrating technology, biology, and computation. Mech Ageing Dev 2003;124:9-16. This systems biology approach to health and disease integrates lifestyle and environmental factors, biology, biomarkers and ‘omics’ technologies, and clinical data.2Hood L, Flores M. A personal view on systems medicine and the emergence of proactive P4 medicine: predictive, preventive, personalized and participatory. N Biotechnol 2012;29(6):613-24.,3Cesario A, Auffray C, Russo P, Hood L. P4 medicine needs P4 education. Curr Pharmaceut De 2014;20,000-000. ‘Omic’ technologies include but are not limited to genomics, epigenomics, transcriptomics, proteomics and metabolomics.3Cesario A, Auffray C, Russo P, Hood L. P4 medicine needs P4 education. Curr Pharmaceut De 2014;20,000-000.,4Hood L. Systems biology and p4 medicine: past, present, and future. Rambam Maimonides Med J 2013;4(2):e0012.,5Liebsch C, Pitchika V, Pink C, Samietz S, Kastenmüller G, Artati A, Suhre K, Adamski J, Nauck M, Völzke H, Friedrich N, Kocher T, Holtfreter B, Pietzner M. The Saliva Metabolome in Association to Oral Health Status. J Dent Res 2019;98(6):642-651. doi: 10.1177/0022034519842853. The 4Ps represent ‘Predictive’, ‘Preventive’, ‘Personalized’ and ‘Participatory.’6Pulciani S, Di Lonardo A, Fagnani C, Taruscio D. P4 medicine versus Hippocrates. Ann Ist Super Sanita 2017;53(3):185-91. (Figure 1) ‘Predictive’ and ‘preventive’ refer to the ability to predict and prevent disease, while ‘personalized’ refers to patient-centered healthcare that is individualized for each unique patient. Participatory refers to patient participation in the care of their health together with healthcare personnel, sharing of information and shared decision-making.
Together, the 4Ps represent an integrative, pro-active approach to healthcare.7Sagner M, McNeil A, Puskac P, Auffray C, Price ND, Hood L, et al. The P4 health spectrum – A predictive, preventive, personalized and participatory continuum for promoting healthspan. Prog Cardiovasc Dis 2017;59(5):506-21.,8Louis R, Roche N. Personalised medicine: are we ready? Eur Respir Rev 2017;26:170088. https://doi.org/10.1183/16000617.0088-2017. P4 medicine has mainly focused on chronic non-communicable diseases which represent the greatest health burden globally.3Cesario A, Auffray C, Russo P, Hood L. P4 medicine needs P4 education. Curr Pharmaceut De 2014;20,000-000.,8Louis R, Roche N. Personalised medicine: are we ready? Eur Respir Rev 2017;26:170088. https://doi.org/10.1183/16000617.0088-2017.,9Bousquet J, Anto JM, Sterk PJ, Adcock IM, Chung KF, Roca J, et al. Systems medicine and integrated care to combat chronic noncommunicable diseases. Genome Med 2011;3(7):43. However, this approach is also being applied to inherited disorders and other diseases.10van Karnebeek CDM, Wortmann SB, Tarailo-Graovac M, Langeveld M, Ferreira CR, van de Kamp JM, et al. The role of the clinician in the multi-omics era: are you ready? J Inherited Metabolic Dis 2018;41:571-82.
P4 Dentistry
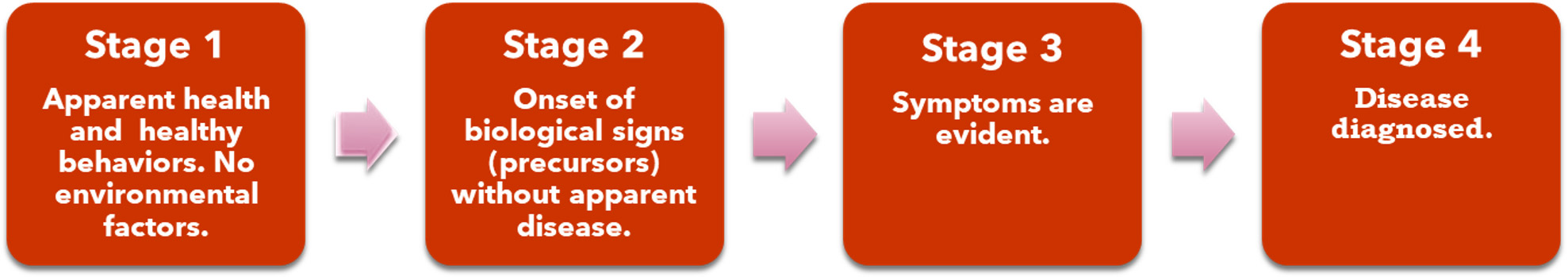
A systems biology approach can benefit oral and systemic health. Four stages have been described for the health-disease continuum 7Sagner M, McNeil A, Puskac P, Auffray C, Price ND, Hood L, et al. The P4 health spectrum – A predictive, preventive, personalized and participatory continuum for promoting healthspan. Prog Cardiovasc Dis 2017;59(5):506-21.,8Louis R, Roche N. Personalised medicine: are we ready? Eur Respir Rev 2017;26:170088. https://doi.org/10.1183/16000617.0088-2017. (Figure 2). Stage A represents apparent health along with healthy behaviors and no environmental factors; stage B represents the onset of disease precursors without apparent disease, stage C ensues when symptoms are evident and Stage D exists when a diagnosis has occurred.7Sagner M, McNeil A, Puskac P, Auffray C, Price ND, Hood L, et al. The P4 health spectrum – A predictive, preventive, personalized and participatory continuum for promoting healthspan. Prog Cardiovasc Dis 2017;59(5):506-21.,8Louis R, Roche N. Personalised medicine: are we ready? Eur Respir Rev 2017;26:170088. https://doi.org/10.1183/16000617.0088-2017. If disease can be accurately predicted at the patient level, targeted interventions to prevent the disease from occurring become possible rather than reactively treating its manifestations.7Sagner M, McNeil A, Puskac P, Auffray C, Price ND, Hood L, et al. The P4 health spectrum – A predictive, preventive, personalized and participatory continuum for promoting healthspan. Prog Cardiovasc Dis 2017;59(5):506-21. Personalized care and patient participation are also essential for this approach to succeed.
Figure 2. Stages for health-disease
Prediction and Prevention in P4 Dentistry
Individual elements related to the 4Ps already exist in dentistry. For example, the use of risk assessment tools for periodontal disease, dental caries and oral cancer are intended to predict risk and provide guidance on the type and level of preventive care required to prevent disease. Evidence supports the use of validated electronic periodontal risk assessment tools.11Lang NP, Suvan JE, Tonetti MS. Risk factor assessment tools for the prevention of periodontitis progression a systematic review. J Clin Periodontol 2015;42(S16):S59-70. A wide range of research is now being conducted using biomarkers and non-invasive tests.12Bartold PM. Lifestyle and periodontitis: The emergence of personalized periodontics. Periodontol 2000 2018;78(1):7-11.
Predictive screening tests being developed include biomarkers in saliva, gingival crevicular fluid (GCF) and blood. Antibodies have been found that may be predictive for Sjӧgren’s syndrome (SS) and its severity, and can be detected up to 20 years prior to patients receiving a diagnosis of SS.13Theander E, Jonsson R, Sjöström B, et al. Prediction of Sjögrens Syndrome years before diagnosis and identification of patients with early onset and severe disease course by autoantibody profiling. Arthritis Rheumatol 2015;67(9):2427-36. While SS cannot at the current time be prevented or cured, this biomarker would predict it and promote pre-emptive education and personalized care such that, for example, the increased risk of dental caries as a sequelae of SS could be managed and oral disease prevented. In the future, it can be hoped that a method of preventing the primary condition could be found that could be applied following predictive tests. Another example is chairside testing for hemoglobin A1c (HbA1c) using gingival crevicular blood as a patient-friendly and accessible method of screening for diabetes mellitus.14Rosedale MT, Strauss SM. Diabetes screening at the periodontal visit: Patient and provider experiences with two screening approaches. Int J Dent Hyg 2012;10(4):250-8. Patients also reported that they learned more about their overall health and risk for diabetes associated with periodontal disease.
‘Inflammaging’ refers to low-grade chronic inflammation that is now known to be part of the aging process.15Franceschi C, Campisi J. Chronic Inflammation (Inflammaging) and Its Potential Contribution to Age-Associated Diseases. J Gerontol 2014 Series A;69 (Suppl 1):S4-S9. https://doi.org/10.1093/gerona/glu057 In addition, chronic systemic inflammation from various sources increases risk for Type 2 diabetes mellitus and cardiovascular disease.16Dregan A, Charlton J, Chowienczyk P, Gulliford MC. Chronic inflammatory disorders and risk of type 2 diabetes mellitus, coronary heart disease, and stroke: a population-based cohort study. Circulation 2014;130(10):837-44. doi: 10.1161/CIRCULATIONAHA.114.009990. Biomarkers associated with ‘inflammaging’ include elevated levels of interleukin-6 (IL-6), C-reactive protein (CRP) and other pro-inflammatory biomarkers.15Franceschi C, Campisi J. Chronic Inflammation (Inflammaging) and Its Potential Contribution to Age-Associated Diseases. J Gerontol 2014 Series A;69 (Suppl 1):S4-S9. https://doi.org/10.1093/gerona/glu057 Similarly, IL-6, CRP, IL-1β, MMP-8 and other biomarkers, alone and in combination, are being researched as biomarkers for periodontitis and its severity.17González-Ramírez J, Serafín-Higuera N, Mancilla MCS, Martínez-Coronilla G, Famanía-Bustamante J, López ALL. Use of Biomarkers for the Diagnosis of Periodontitis. InTech Open, March 25, 2019. doi: 10.5772/intechopen.85394,18Korte DL, Kinney J. Personalized medicine: an update of salivary biomarkers for periodontal diseases. Periodontol 2000 2016;70:26-37. In metabolomic research, it has been found that salivary metabolites change with oral health status and aging.5Liebsch C, Pitchika V, Pink C, Samietz S, Kastenmüller G, Artati A, Suhre K, Adamski J, Nauck M, Völzke H, Friedrich N, Kocher T, Holtfreter B, Pietzner M. The Saliva Metabolome in Association to Oral Health Status. J Dent Res 2019;98(6):642-651. doi: 10.1177/0022034519842853. In particular, the bacterial metabolite phenylacetate is regarded as promising as a biomarker given its association with periodontitis.5Liebsch C, Pitchika V, Pink C, Samietz S, Kastenmüller G, Artati A, Suhre K, Adamski J, Nauck M, Völzke H, Friedrich N, Kocher T, Holtfreter B, Pietzner M. The Saliva Metabolome in Association to Oral Health Status. J Dent Res 2019;98(6):642-651. doi: 10.1177/0022034519842853. At the current time, research is ongoing to find a robust biomarker, or a combination of biomarkers, predictive for periodontal disease and its severity. Other advances can personalize treatment and chemotherapeutics. If found, together these would represent a true paradigm shift and promote 4P-based prevention and treatment.
Patient Participation and Personalized Care
Patient-centered (personalized) care has been defined as care ‘provided in a respectful manner, assures open and ongoing sharing of useful information in an ongoing manner and supports and encourages the participation of patients and their families.19Newell S, Jordan Z. The patient experience of patient-centered communication with nurses in the hospital setting: a qualitative systematic review protocol. JBI Database System Rev Implement Rep 2015;13(1):76-87. doi: 10.11124/jbisrir-2015-1072. Patient participation involves shared decision-making with the patient’s provider, active involvement and self-care.20Truglio-Londrigan M, Slyer JT, Singleton JK, Worral P. A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. JBI Libr Syst Rev 2012;10(58):4633-46. Recommendations for shared decision-making include a number of steps.21Thériault G, Bell NR, Grad R, Singh H, Szafran O. Teaching shared decision making: An essential competency. Canadian Family Physician 2019;65:514-6. Once it has been agreed a decision needs to be made, it is recommended that options and alternatives should be provided in an unbiased manner along with decision aids as necessary. Potential risk and benefits should be described, and quantified using numbers rather than percentages. Following this, it is recommended that patient preferences be discussed, the outcomes of different options, and more information provided on specific aspects of the decision-making. (Figure 3)
Patients in one study defined non-participation as interactions that were not patient-centered.22Catrine A, Ekman I, Ehnfors M. Considering patient non-participation in health care. Health Expectations 2008;11:263-71. This meant not being listened to, the absence of recognition of their individual needs, and information that was either received but not understood or not provided. A patient’s ability to participate and share in decision making also varies with age, socio-economic status, education and culture.20Truglio-Londrigan M, Slyer JT, Singleton JK, Worral P. A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. JBI Libr Syst Rev 2012;10(58):4633-46. In addition, provider understanding of patients’ levels of health literacy is essential.7Sagner M, McNeil A, Puskac P, Auffray C, Price ND, Hood L, et al. The P4 health spectrum – A predictive, preventive, personalized and participatory continuum for promoting healthspan. Prog Cardiovasc Dis 2017;59(5):506-21. Patient participation is promoted when information is individualized and the patient’s knowledge is recognized, and when patient decision-making involves knowledge and needs.23Eldh AC, Ekman I, Ehnfors M. Conditions for patient participation and non-participation in health care. Nurs Ethics 2006;13(5):503-14. Effective communication between patient and provider is essential for patient participation and personalized care.
Communication and Integrating the 4Ps
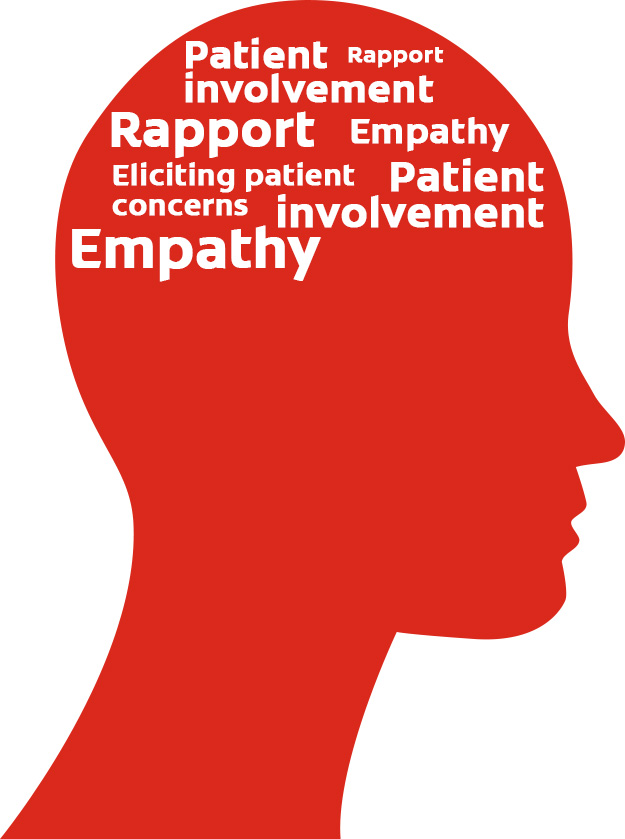
Patient-centered communication has been defined as ‘communication that invites and encourages the patient to participate and negotiate in decision-making regarding their own care’.19Newell S, Jordan Z. The patient experience of patient-centered communication with nurses in the hospital setting: a qualitative systematic review protocol. JBI Database System Rev Implement Rep 2015;13(1):76-87. doi: 10.11124/jbisrir-2015-1072. In a recent systematic review, it was found that establishing rapport, eliciting patient concerns, demonstrating empathy and involvement in their treatment plans are regarded by patients as important for effective patient-centered communication. (Figure 4) Goals within ‘Healthy People 2020’ include increasing the percentage of healthcare providers noted by patients to always listen to them, provide understandable information and to have satisfactory communication skills.24U.S. Department of Health and Human Services. 2011. Healthy People.gov: http://www.healthypeople.gov/2020/default.aspx
According to the Department of Health and Human Services, approximately 9 in 10 adults are not proficient at using everyday health information.25U.S. Department of Health and Human Services. National Action Plan to Improve Health Literacy. Available at: https://health.gov/communication/hlactionplan/pdf/Health_Literacy_Action_Plan.pdf. In order to communicate effectively, the use of plain language, teach-back, patient-friendly methods and visual aids is recommended.26Podschun G. 5 Oral Health Literacy Programs.” Institute of Medicine. 2013. Oral Health Literacy: Workshop Summary. Washington, DC: The National Academies Press. doi: 10.17226/13484.,27Buerlein JK, Horowitz AM, Child WL. Perspectives of Maryland women regarding oral health during pregnancy and early childhood. J Public Health Dent 2011;71(2):131-5.,28U.S. Department of Health and Human Services. Quick Guide to Health Literacy. Fact Sheet. Available at: https://health.gov/communication/literacy/quickguide/factsbasic.htm#seven. Plain language includes but is not limited to providing key information first or alone to improve understanding, breaking down complex information, and using simple language.29Sheridan SL, Halpern DJ, Viera AJ, Berkman ND, Donahue KE, Crotty K. Interventions for individuals with low health literacy: a systematic review. J Health Commun 2011;16 Suppl 3:30-54. Use of visual and verbal tools including adding icons helps to improve patients’ understanding of numerical data. Visual aids that improve learning and knowledge include supplemental videos, DVDs, models, computer-based and graphics-based information.29Sheridan SL, Halpern DJ, Viera AJ, Berkman ND, Donahue KE, Crotty K. Interventions for individuals with low health literacy: a systematic review. J Health Commun 2011;16 Suppl 3:30-54.,30Strömberg A, Dahlström U, Fridlund B. Computer-based education for patients with chronic heart failure. A randomised, controlled, multicentre trial of the effects on knowledge, compliance and quality of life. Patient Educ Couns 2006;64(1-3):128-35. This has also been shown to help mitigate differences in literacy and educational materials, and to improve home self-care and disease prevention (in this case, dental caries).31Albert NM, Buchsbaum R, Li J. Randomized study of the effect of video education on heart failure healthcare utilization, symptoms, and self-care behaviors. Patient Educ Couns 2007;69(1-3):129-39.,32Davis TC, Mayeaux EJ, Fredrickson D, Bocchini JA Jr, Jackson RH, Murphy PW. Reading ability of parents compared with reading level of pediatric patient education materials. Pediatrics 1994;93(3):460-8.,33Newitter DA, Meiers JC, Kazemi RB. Rx for caries prevention: time line for home care. A software aid for communication of patient instructions for management of dental caries. Oper Dent 2002;27(2):204-7.
Further, patients must understand risk in order to participate in prevention. However, risk is ill-understood, including among well-educated individuals.34Gigerenzer G, Gaissmaier W, Kurz-Milcke E, Schwartz LM, Woloshin S. Helping doctors and patients make sense of health statistics. Psychological science in the public interest. J Am Psych Society 2007;8(2):53-96. Risk, relative risk levels and basic statistical information are problematic concepts.34Gigerenzer G, Gaissmaier W, Kurz-Milcke E, Schwartz LM, Woloshin S. Helping doctors and patients make sense of health statistics. Psychological science in the public interest. J Am Psych Society 2007;8(2):53-96.,35Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making 2001;21(1):37-44. One method recommended to help overcome poor statistical literacy is to use an absolute number, such as 3 in 100 instead of stating ‘a 3% chance.’21Thériault G, Bell NR, Grad R, Singh H, Szafran O. Teaching shared decision making: An essential competency. Canadian Family Physician 2019;65:514-6. Graphic presentations of risk, as used in risk assessment tools, also help to educate patients and improve care. Personalized web pages for patients with individualized education can also be provided.36Yeh YT, Chiu YT, Liu CT, Wu SJ, Lee TI. Development and evaluation of an integrated patient-oriented education management system for diabetes. Stud Health Technol Inform 2006;122:172-5.
Communication style influences its effectiveness and how patients perceive communication and providers. In one study with pediatric dentists, discussions that were empathetic, reassuring and provided positive reinforcement lead to patient perceptions that care was more patient-centered and resulted in greater patient-provider interaction.37Wong HM, Bridges SM, McGrath CP, Yiu CKY, Zayts OA, Au TKF. Impact of prominent themes in clinician-patient conversations on caregiver’s perceived quality of communication with paediatric dental visits. PLoS ONE 2017;12(1):e0169059. In contrast, conversations focused on procedures did not have this effect. Differences in content recall suggest a mismatch between dentists and patients.38Misra S, Daly B, Dunne S, Millar B, Packer M, Asimakopoulou K. Dentist–patient communication: what do patients and dentists remember following a consultation? Implications for patient compliance. Patient Preference and Adherence 2013:7:543-9. Patients recall less information on oral health than dentists recall providing. Studies have reported that patients did not recall information on home care and post-operative instructions.38Misra S, Daly B, Dunne S, Millar B, Packer M, Asimakopoulou K. Dentist–patient communication: what do patients and dentists remember following a consultation? Implications for patient compliance. Patient Preference and Adherence 2013:7:543-9.,39Blinder D, Rotenberg L, Peleg M, Taicher S. Patient compliance to instructions after oral surgical procedures. Int J Oral Maxillofac Surg 2001;30(3):216-9. Knowledge level influences recall, further highlighting the need for training and education, and improved oral health literacy.38Misra S, Daly B, Dunne S, Millar B, Packer M, Asimakopoulou K. Dentist–patient communication: what do patients and dentists remember following a consultation? Implications for patient compliance. Patient Preference and Adherence 2013:7:543-9.
‘There’s an app for that’ is increasingly the case, and an opportunity for oral health education. Apps are available for patient and direct-to-consumer education; as tobacco cessation aids; and for tracking of, and information on, habits and oral hygiene. However, a recent study found that educational opportunities were missed, some apps focused on cosmetic issues while omitting related health information, and usability issues were found.40Tiffany B, Blasi P, Catz SL, McClure JB. Mobile apps for oral health promotion: Content review and heuristic usability analysis. JMIR Mhealth Uhealth 2018;6:e11432. Further, few apps included gain-framed messaging, thereby missing an opportunity to frame behavior change for a positive outcome.
Training
Competencies in interpersonal and communication skills are embodied in the Commission on Dental Accreditation’s standards for Dental and Dental Hygiene programs.41Commission on Dental Accreditation. Accreditation standards for dental education programs. Chicago: 2010. Healthcare providers exhibit a more patient-centered approach if they have received communications training.42Mull, Carrie, “Implementation of a Patient-Centered Communication Model in the Emergency Department” (2017). Doctoral Projects. https://scholarworks.gvsu.edu/kcon_doctoralprojects/46 Effective options for training include all-day or multi-day training, simulated patient encounters, role playing, taping and analyses of interactions. Such encounters can be live simulations or computer-based.42Mull, Carrie, “Implementation of a Patient-Centered Communication Model in the Emergency Department” (2017). Doctoral Projects. https://scholarworks.gvsu.edu/kcon_doctoralprojects/46 In a recent study, pre-clinical dental students participated in interactive communication training that included videoing and analyses of exercises and role playing.43Alvarez S, Schultz J-H. A communication-focused curriculum for dental students – an experiential training approach. BMC Medical Education 2018;18:55. https://doi.org/10.1186/s12909-018-1174-6 Students reported the course to be effective and important. Topics addressed included active listening, taking medical histories, simulated patient-provider interactions, learning about empathy and sympathy, non-verbal communication, self-awareness and self-perception. Further, increased recognition of the importance of patient communication and interaction for optimal health and healthcare has led to an increased focus on communication skills.43Alvarez S, Schultz J-H. A communication-focused curriculum for dental students – an experiential training approach. BMC Medical Education 2018;18:55. https://doi.org/10.1186/s12909-018-1174-6
Conclusions
Using a systems biology approach, diseases and disorders may be predicted and prevented using patient-level information and biomarkers. This approach can also be used to individualize and optimize treatment. More research is required to identify robust biomarkers, to fully understand disease/disorder processes and the most effective prevention regimens and treatments. Digital technologies can play a role and be further developed to offer opportunities for information-gathering, research and data interpretation, and P4-based proactive healthcare. Further, the ability to communicate effectively with patients, and education for oral health literacy, are integral to personalized care and patient participation, and therefore to P4 dentistry overall. In conclusion, integrating the 4Ps into patient care holds promise for improving and optimizing oral and systemic health.
References
- 1.Dominy SS, et al. Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Sci Adv. 2019;5(1):eaau3333 https://www.ncbi.nlm.nih.gov/pubmed/30746447.
- 2.Sadrameli M, et al. Linking mechanisms of periodontitis to Alzheimer’s disease. Curr Opin Neurol. 2020;33(2):230-8 https://www.ncbi.nlm.nih.gov/pubmed/32097126.
- 3.Borsa L, et al. Analysis the link between periodontal diseases and Alzheimer’s disease: A systematic review. Int J Environ Res Public Health. 2021;18(17) https://www.ncbi.nlm.nih.gov/pubmed/34501899.
- 4.Costa MJF, et al. Relationship of Porphyromonas gingivalis and Alzheimer’s disease: A systematic review of pre-clinical studies. Clin Oral Investig. 2021;25(3):797-806 https://www.ncbi.nlm.nih.gov/pubmed/33469718.
- 5.Munoz Fernandez SS, Lima Ribeiro SM. Nutrition and Alzheimer disease. Clin Geriatr Med. 2018;34(4):677-97 https://www.ncbi.nlm.nih.gov/pubmed/30336995.
- 6.Aquilani R, et al. Is the Brain Undernourished in Alzheimer’s Disease? Nutrients. 2022;14(9) https://www.ncbi.nlm.nih.gov/pubmed/35565839.
- 7.Fukushima-Nakayama Y, et al. Reduced mastication impairs memory function. J Dent Res. 2017;96(9):1058-66 https://www.ncbi.nlm.nih.gov/pubmed/28621563.
- 8.Kim HB, et al. Abeta accumulation in vmo contributes to masticatory dysfunction in 5XFAD Mice. J Dent Res. 2021;100(9):960-7 https://www.ncbi.nlm.nih.gov/pubmed/33719684.
- 9.Miura H, et al. Relationship between cognitive function and mastication in elderly females. J Oral Rehabil. 2003;30(8):808-11 https://www.ncbi.nlm.nih.gov/pubmed/12880404.
- 10.Lexomboon D, et al. Chewing ability and tooth loss: association with cognitive impairment in an elderly population study. J Am Geriatr Soc. 2012;60(10):1951-6 https://www.ncbi.nlm.nih.gov/pubmed/23035667.
- 11.Elsig F, et al. Tooth loss, chewing efficiency and cognitive impairment in geriatric patients. Gerodontology. 2015;32(2):149-56 https://www.ncbi.nlm.nih.gov/pubmed/24128078.
- 12.Kim EK, et al. Relationship between chewing ability and cognitive impairment in the rural elderly. Arch Gerontol Geriatr. 2017;70:209-13 https://www.ncbi.nlm.nih.gov/pubmed/28214402.
- 13.Kim MS, et al. The association between mastication and mild cognitive impairment in Korean adults. Medicine (Baltimore). 2020;99(23):e20653 https://www.ncbi.nlm.nih.gov/pubmed/32502052.
- 14.Cardoso MG, et al. Relationship between functional masticatory units and cognitive impairment in elderly persons. J Oral Rehabil. 2019;46(5):417-23 https://www.ncbi.nlm.nih.gov/pubmed/30614023.
- 15.Popovac A, et al. Oral health status and nutritional habits as predictors for developing alzheimer’s disease. Med Princ Pract. 2021;30(5):448-54 https://www.ncbi.nlm.nih.gov/pubmed/34348313.
- 16.Park T, et al. More teeth and posterior balanced occlusion are a key determinant for cognitive function in the elderly. Int J Environ Res Public Health. 2021;18(4) https://www.ncbi.nlm.nih.gov/pubmed/33669490.
- 17.Lin CS, et al. Association between tooth loss and gray matter volume in cognitive impairment. Brain Imaging Behav. 2020;14(2):396-407 https://www.ncbi.nlm.nih.gov/pubmed/32170642.
- 18.Kumar S, et al. Oral health status and treatment need in geriatric patients with different degrees of cognitive impairment and dementia: a cross-sectional study. J Family Med Prim Care. 2021;10(6):2171-6 https://www.ncbi.nlm.nih.gov/pubmed/34322409.
- 19.Delwel S, et al. Chewing efficiency, global cognitive functioning, and dentition: A cross-sectional observational study in older people with mild cognitive impairment or mild to moderate dementia. Front Aging Neurosci. 2020;12:225 https://www.ncbi.nlm.nih.gov/pubmed/33033478.
- 20.Da Silva JD, et al. Association between cognitive health and masticatory conditions: a descriptive study of the national database of the universal healthcare system in Japan. Aging (Albany NY). 2021;13(6):7943-52 https://www.ncbi.nlm.nih.gov/pubmed/33739304.
- 21.Galindo-Moreno P, et al. The impact of tooth loss on cognitive function. Clin Oral Investig. 2022;26(4):3493-500 https://www.ncbi.nlm.nih.gov/pubmed/34881401.
- 22.Stewart R, et al. Adverse oral health and cognitive decline: The health, aging and body composition study. J Am Geriatr Soc. 2013;61(2):177-84 https://www.ncbi.nlm.nih.gov/pubmed/23405916.
- 23.Dintica CS, et al. The relation of poor mastication with cognition and dementia risk: A population-based longitudinal study. Aging (Albany NY). 2020;12(9):8536-48 https://www.ncbi.nlm.nih.gov/pubmed/32353829.
- 24.Kim MS, Han DH. Does reduced chewing ability efficiency influence cognitive function? Results of a 10-year national cohort study. Medicine (Baltimore). 2022;101(25):e29270 https://www.ncbi.nlm.nih.gov/pubmed/35758356.
- 25.Ko KA, et al. The Impact of Masticatory Function on Cognitive Impairment in Older Patients: A Population-Based Matched Case-Control Study. Yonsei Med J. 2022;63(8):783-9 https://www.ncbi.nlm.nih.gov/pubmed/35914761.
- 26.Garre-Olmo J. [Epidemiology of Alzheimer’s disease and other dementias]. Rev Neurol. 2018;66(11):377-86 https://www.ncbi.nlm.nih.gov/pubmed/29790571.
- 27.Stephan BCM, et al. Secular Trends in Dementia Prevalence and Incidence Worldwide: A Systematic Review. J Alzheimers Dis. 2018;66(2):653-80 https://www.ncbi.nlm.nih.gov/pubmed/30347617.
- 28.Lopez OL, Kuller LH. Epidemiology of aging and associated cognitive disorders: Prevalence and incidence of Alzheimer’s disease and other dementias. Handb Clin Neurol. 2019;167:139-48 https://www.ncbi.nlm.nih.gov/pubmed/31753130.
- 29.Ono Y, et al. Occlusion and brain function: mastication as a prevention of cognitive dysfunction. J Oral Rehabil. 2010;37(8):624-40 https://www.ncbi.nlm.nih.gov/pubmed/20236235.
- 30.Kubo KY, et al. Masticatory function and cognitive function. Okajimas Folia Anat Jpn. 2010;87(3):135-40 https://www.ncbi.nlm.nih.gov/pubmed/21174943.
- 31.Chen H, et al. Chewing Maintains Hippocampus-Dependent Cognitive Function. Int J Med Sci. 2015;12(6):502-9 https://www.ncbi.nlm.nih.gov/pubmed/26078711.
- 32.Azuma K, et al. Association between Mastication, the Hippocampus, and the HPA Axis: A Comprehensive Review. Int J Mol Sci. 2017;18(8) https://www.ncbi.nlm.nih.gov/pubmed/28771175.
- 33.Chuhuaicura P, et al. Mastication as a protective factor of the cognitive decline in adults: A qualitative systematic review. Int Dent J. 2019;69(5):334-40 https://www.ncbi.nlm.nih.gov/pubmed/31140598.
- 34.Lopez-Chaichio L, et al. Oral health and healthy chewing for healthy cognitive ageing: A comprehensive narrative review. Gerodontology. 2021;38(2):126-35 https://www.ncbi.nlm.nih.gov/pubmed/33179281.
- 35.Tada A, Miura H. Association between mastication and cognitive status: A systematic review. Arch Gerontol Geriatr. 2017;70:44-53 https://www.ncbi.nlm.nih.gov/pubmed/28042986.
- 36.Ahmed SE, et al. Influence of Dental Prostheses on Cognitive Functioning in Elderly Population: A Systematic Review. J Pharm Bioallied Sci. 2021;13(Suppl 1):S788-S94 https://www.ncbi.nlm.nih.gov/pubmed/34447202.
- 37.Tonsekar PP, et al. Periodontal disease, tooth loss and dementia: Is there a link? A systematic review. Gerodontology. 2017;34(2):151-63 https://www.ncbi.nlm.nih.gov/pubmed/28168759.
- 38.Nangle MR, Manchery N. Can chronic oral inflammation and masticatory dysfunction contribute to cognitive impairment? Curr Opin Psychiatry. 2020;33(2):156-62 https://www.ncbi.nlm.nih.gov/pubmed/31895157.
- 39.Nakamura T, et al. Oral dysfunctions and cognitive impairment/dementia. J Neurosci Res. 2021;99(2):518-28 https://www.ncbi.nlm.nih.gov/pubmed/33164225.
- 40.Weijenberg RAF, et al. Mind your teeth-The relationship between mastication and cognition. Gerodontology. 2019;36(1):2-7 https://www.ncbi.nlm.nih.gov/pubmed/30480331.
- 41.Asher S, et al. Periodontal health, cognitive decline, and dementia: A systematic review and meta-analysis of longitudinal studies. J Am Geriatr Soc. 2022;70(9):2695-709 https://www.ncbi.nlm.nih.gov/pubmed/36073186.
- 42.Lin CS. Revisiting the link between cognitive decline and masticatory dysfunction. BMC Geriatr. 2018;18(1):5 https://www.ncbi.nlm.nih.gov/pubmed/29304748.
- 43.Wu YT, et al. The changing prevalence and incidence of dementia over time – current evidence. Nat Rev Neurol. 2017;13(6):327-39 https://www.ncbi.nlm.nih.gov/pubmed/28497805.
- 44.National Psoriasis Foundation. Soriatane (Acitretin). https://www.psoriasis.org/soriatane-acitretin/.
- 45.National Psoriasis Foundation. Current Biologics on the Market. https://www.psoriasis.org/current-biologics-on-the-market/.
- 46.Dalmády S, Kemény L, Antal M, Gyulai R. Periodontitis: a newly identified comorbidity in psoriasis and psoriatic arthritis. Expert Rev Clin Immunol 2020;16(1):101-8. doi: 10.1080/1744666X.2019.1700113.
:sharpen(level=0):output(format=jpeg)/up/2023/05/Fiona-Collins-thumbnail-1-3.jpg)
:sharpen(level=0):output(format=jpeg)/up/2019/11/Integrating-the-4Ps-into-Patient-Care-2.jpg)