The Dangers of Sugar-Sweetened Beverages: Dental Professionals Must Respond
The threat to health posed by over-consumption of sugar-sweetened beverages (SSB) is well documented. These beverages include sodas, energy and vitamin drinks, fruit juice and other soft drinks containing added sugars.1Bleich SN, Vercammen KA. The negative impact of sugar-sweetened beverages on children’s health: an update of the literature. BMC Obesity 2018;5:6,2Hu FB. Resolved: There is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes Rev 2013;14(8):606-19.,3Luger M, Lafontan M, Bes-Rastrollo M, Winzer E, Yumuk V, Farpour-Lambert N. Sugar-sweetened beverages and weight gain in children and adults: A systematic review from 2013 to 2015 and a comparison with previous studies. Obes Facts 2017;10:674-93. SSB promote weight gain and the adverse health effects associated with being overweight or obese.2Hu FB. Resolved: There is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes Rev 2013;14(8):606-19.,3Luger M, Lafontan M, Bes-Rastrollo M, Winzer E, Yumuk V, Farpour-Lambert N. Sugar-sweetened beverages and weight gain in children and adults: A systematic review from 2013 to 2015 and a comparison with previous studies. Obes Facts 2017;10:674-93.
This has led to a call for renewed efforts to reduce SSB consumption, including taxation, labeling changes and behavioral interventions.4Lee BY, Ferguson MC, Hertenstein DL, Adam A, Zenkov E, Wang PI, Wong MS, Gittelsohn J, Mui Y, Brown ST. Simulating the impact of sugar-sweetened beverage warning labels in three cities. Am J Prev Med 2018;54(2):197-204. doi: 10.1016/j.amepre.2017.11.003.,5Abdel Rahman A, Jomaa L, Kahale LA, Adair P, Pine C. Effectiveness of behavioral interventions to reduce the intake of sugar-sweetened beverages in children and adolescents: a systematic review and meta-analysis. Nutr Rev 2018;76(2):88-107. doi: 10.1093/nutrit/nux061. The role of dental professionals in this effort must also be considered. This is in relationship to the larger issue of dental professionals applying a common risk factor approach to emphasize the importance of prevention as fundamental to controlling the development and progression of many oral and systemic diseases.
Health Impact of SSB
In a systematic review of 30 studies conducted between January 2013 and October 2015, a significant association was found for SSB consumption and weight gain in children and adults.3Luger M, Lafontan M, Bes-Rastrollo M, Winzer E, Yumuk V, Farpour-Lambert N. Sugar-sweetened beverages and weight gain in children and adults: A systematic review from 2013 to 2015 and a comparison with previous studies. Obes Facts 2017;10:674-93. Further, in an Australian study of children 2 to 16 years-of-age, consuming at least 2 servings of SSB daily (>250 g/day) carried a 26% greater risk of being overweight or obese compared to consuming less.6Grimes CA, Riddell LJ, Campbell KJ, Nowson CA. Dietary salt intake, sugar-sweetened beverage consumption, and obesity risk. Pediatrics 2013;131(1):14-21. A majority of studies in another review also support a relationship between SSB consumption and insulin resistance in children and adolescents.1Bleich SN, Vercammen KA. The negative impact of sugar-sweetened beverages on children’s health: an update of the literature. BMC Obesity 2018;5:6. Since childhood obesity is associated with asthma, attention-deficit disorder, and reduced quality of life and educational achievement,7Bussiek P-BV, De Poli C, Bevan G. A scoping review protocol to map the evidence on interventions to prevent overweight and obesity in children. BMJ Open 2018;8:e019311. reduction in SSB consumption is an important public health initiative. Studies further highlight a relationship between adult consumption of SSB, and diabetes mellitus (DM) and cardiovascular disease, with a direct dose-response observed for long-term weight gain and DM.2Hu FB. Resolved: There is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes Rev 2013;14(8):606-19. Globally, an estimated 184,000 deaths per year are associated with intake of SSB, with 72.3%, 24.2% and 3.5% of these deaths attributed to DM, cardiovascular disease and cancers, respectively.8Singh GM, Micha R, Khatibzadeh S, Lim S, Ezzati M, Mozaffarian D; Global Burden of Diseases Nutrition and Chronic Diseases Expert Group (NutriCoDE). Estimated global, regional, and national disease burdens related to sugar-sweetened beverage consumption in 2010. Circulation 2015;132:639-66. (Figure 1)
Consumption of SSB is clearly associated with dental caries. Third graders in one study from the United States were found to consume an average of 2 SSB per day.9Wilder JR, Kaste LM, Handler A, Chapple-McGruder T, Rankin KM. The association between sugar-sweetened beverages and dental caries among third-grade students in Georgia. J Public Health Dent 2016;76:76-84. After adjusting for socioeconomic status and maternal oral health, a 22% increase in dental caries was found for each additional SSB consumed daily. Greater SSB consumption has also been found to result in up to a four-fold increased risk of severe early childhood caries.10Evans EW, Hayes C, Palmer CA, Bermudez OI, Cohen SA, Must A. Dietary intake and severe early childhood caries in low-income, young children. J Acad Nutr Diet 2013;113(8):1057-61. In adolescents, intake of SSB has been found to be associated with toothache and food avoidance due to dental discomfort, with consumption of energy and sports drinks noted to be of particular concern.11Hardy LL, Bell J, Bauman A, Mihrshahi S. Association between adolescents’ consumption of total and different types of sugar-sweetened beverages with oral health impacts and weight status. Aust N Z J Public Health 2018;42(1):22-6. doi: 10.1111/1753-6405.12749.
Effect of Reduced Intake of SSB
Recent randomized controlled clinical trials have confirmed health improvements following reduced intake of SSB.1Bleich SN, Vercammen KA. The negative impact of sugar-sweetened beverages on children’s health: an update of the literature. BMC Obesity 2018;5:6.,2Hu FB. Resolved: There is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obes Rev 2013;14(8):606-19.,12de Ruyter JC, Olthof MR, Seidell JC, Katan MB. A trial of sugar-free or sugar-sweetened beverages and body weight in children. N Engl J Med 2012;367(15):1397-406. In a Dutch study, more than 600 children 4 to 11 years-of-age, and of normal weight, received 8 oz. (250 ml) of a sugar-free drink or an SSB daily for 18 months. Reduced weight gain was observed in the group receiving sugar-free drinks.12de Ruyter JC, Olthof MR, Seidell JC, Katan MB. A trial of sugar-free or sugar-sweetened beverages and body weight in children. N Engl J Med 2012;367(15):1397-406. In another study, among English children ages 7 to 11 years, fewer children in the group receiving 4 educational sessions that discouraged SSB consumption were overweight at the end of the school year than in the control group, although this benefit was not sustained.13James J, Thomas P, Kerr D. Preventing childhood obesity: two year followup results from the Christchurch obesity prevention programme in schools (CHOPPS). BMJ 2007;335(7623):762. In a third study with more than 200 adolescents, weight reductions were again observed in the intervention group at the end of 12 months, but not sustained.14Ebbeling CB, Feldman HA, Chomitz VR, Antonelli TA, Gortmaker SL, Osganian SK, Ludwig DS. A randomized trial of sugar-sweetened beverages and adolescent body weight. N Engl J Med 2012;367(15):1407-16.
Policy Interventions to Reduce SSB Consumption
Placement of health warning labels on SSB regarding their association with obesity, DM and tooth decay may reduce intent-to-purchase. In an online survey of more than 2000 parents, 40% of parents would select an SSB with a warning label.
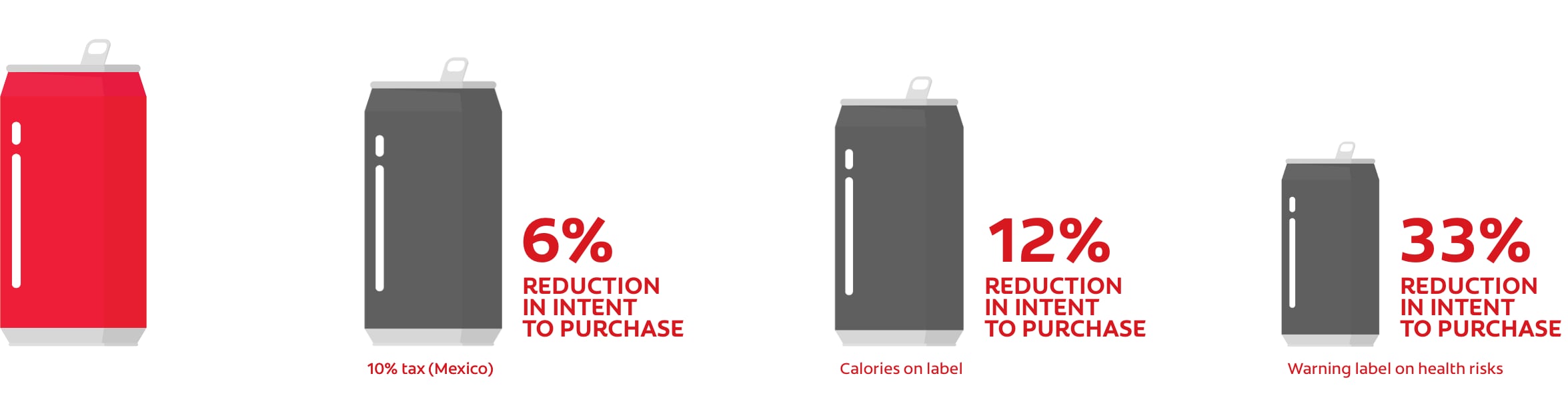
Figure 2.
Influence of taxes and labeling on consumption and selection of SSB
Role of Dental Professionals
A recent review of interventions for Native American children and adolescents in Alaska concluded that a variety of approaches should be emphasized, including education of the entire family and a community-based approach.28Chi DL. Reducing Alaska Native paediatric oral health disparities: a systematic review of oral health interventions and a case study on multilevel strategies to reduce sugar-sweetened beverage intake. Int J Circumpolar Health 2013;72:21066. This analysis emphasized the need for culturally-appropriate interventions. Another review examined interventions that could help children younger than 12 years-of-age.
Two studies involving dental offices were identified, in which dental
In an online survey of pediatric dentists and dental residents, 94% of more than 1600 respondents indicated that they provided information and advice on SSB.26Wright R, Casamassimo PS. Assessing attitudes and actions of pediatric dentists toward childhood obesity and sugar-sweetened beverages. J Pub Health Dent 2017;77:S79-S87. While only 17% offered additional interventions for childhood obesity, a majority of the remaining respondents stated that they would be interested in doing so. Weight and height measurements, and advice were most frequently provided. Other surveys also indicate that few dental professionals provide obesity interventions or are comfortable discussing weight.29Curran AE, Caplan DJ, Lee JY, Paynter L, Gizlice Z, Champagne C, Agans R. Dentists’ attitudes about their role in addressing obesity in patients: a national survey. J Am Dent Assoc 2010;141(11):1307-16.,30Braithwaite AS, Vann J, William F, Switzer BR, Boyd KL, Lee JY. Nutritional counseling practices: how do North Carolina pediatric dentists weigh in? Pediatr Dent 2008;30(6):488-95. (Table 1)
| Table 1. Roles for dental professionals |
|---|
| Nutritional and obesity education for patients |
| Patient education on a healthy lifestyle and physical activity |
| Community-based education |
| Medical referrals for overweight and at-risk individuals |
| Motivational interviewing and active listening |
| Weight and height measurements |
Barriers to Interventions by Dental Professionals
Barriers to providing education and other interventions for childhood obesity in the dental office include a perceived lack of parental interest and acceptance, parental dissatisfaction, fear of offending parents and giving the appearance of being judgmental.26Wright R, Casamassimo PS. Assessing attitudes and actions of pediatric dentists toward childhood obesity and sugar-sweetened beverages. J Pub Health Dent 2017;77:S79-S87.,29Curran AE, Caplan DJ, Lee JY, Paynter L, Gizlice Z, Champagne C, Agans R. Dentists’ attitudes about their role in addressing obesity in patients: a national survey. J Am Dent Assoc 2010;141(11):1307-16.,31Lee JY, Caplan DJ, Gizlice Z, Ammerman A, Agans R, Curran AE. US pediatric dentists’ counseling practices in addressing childhood obesity. Pediatr Dent 2012;34(3):245-50.,32Bell KP, Phillips C, Paquette DW, Offenbacher S, Wilder RS. Incorporating oral-systemic evidence into patient care: practice behaviors and barriers of North Carolina dental hygienists. J Dent Hyg 2011;85(2):99-113. Lack of time, the lack of trained personnel, limited personal knowledge or training on nutrition and obesity, absence of appropriate referral options, and lack of or inadequate reimbursement are also barriers.26Wright R, Casamassimo PS. Assessing attitudes and actions of pediatric dentists toward childhood obesity and sugar-sweetened beverages. J Pub Health Dent 2017;77:S79-S87.,29Curran AE, Caplan DJ, Lee JY, Paynter L, Gizlice Z, Champagne C, Agans R. Dentists’ attitudes about their role in addressing obesity in patients: a national survey. J Am Dent Assoc 2010;141(11):1307-16.,31Lee JY, Caplan DJ, Gizlice Z, Ammerman A, Agans R, Curran AE. US pediatric dentists’ counseling practices in addressing childhood obesity. Pediatr Dent 2012;34(3):245-50.,32Bell KP, Phillips C, Paquette DW, Offenbacher S, Wilder RS. Incorporating oral-systemic evidence into patient care: practice behaviors and barriers of North Carolina dental hygienists. J Dent Hyg 2011;85(2):99-113. Eighty-one percent of respondents believed that parents accept advice on SSB consumption while only 14% and 7%, respectively, held the same belief with respect to obesity education and screening.26Wright R, Casamassimo PS. Assessing attitudes and actions of pediatric dentists toward childhood obesity and sugar-sweetened beverages. J Pub Health Dent 2017;77:S79-S87. In contrast, in another study the dental setting was considered appropriate for height and weight measurements, and information on a healthy diet and physical activity, by 88% and 95% of parents, respectively.33Tavares M, Chomitz V. A healthy weight intervention for children in a dental setting: a pilot study. J Am Dent Assoc 2009;140(3):313-6. In a 2017 systematic review only three studies were found that reported nutritional or obesity-related training in dental and dental hygiene schools.34Divaris K, Bhaskar V, McGraw KA. Pediatric obesity-related curricular content and training in dental schools and dental hygiene programs: systematic review and recommendations. J Public Health Dent 2017;77(Suppl 1):S96-S103. The World Health Organization, however, recommends that nutritional training be incorporated globally into the dental curriculum.35Moynihan P. Sugars and dental caries: Evidence for setting a recommended threshold for intake 1–3. Adv Nutr 2016;7:149-56.
Conclusions
Reducing intake of SSB requires the efforts of the entire community, including active participation and collaboration by all members of the health care team.9Wilder JR, Kaste LM, Handler A, Chapple-McGruder T, Rankin KM. The association between sugar-sweetened beverages and dental caries among third-grade students in Georgia. J Public Health Dent 2016;76:76-84. Dental professionals can to play an important role in this effort by educating patients on the risks associated with SSB, and by influencing policy.36Sanghavi A, Siddiqui NJ. Advancing oral health policy and advocacy to prevent childhood obesity and reduce children’s consumption of sugar-sweetened beverages. J Public Health Dent 2017;77(Suppl 1):S88-S95. Standardized training and continuing education programs are required to provide dental professionals with the knowledge to fulfil this role.35Moynihan P. Sugars and dental caries: Evidence for setting a recommended threshold for intake 1–3. Adv Nutr 2016;7:149-56. Further research is required on interprofessional collaboration to address childhood obesity and oral disease, and on evidence-based interventions that will be most effective.7Bussiek P-BV, De Poli C, Bevan G. A scoping review protocol to map the evidence on interventions to prevent overweight and obesity in children. BMJ Open 2018;8:e019311.,24Dooley D, Moultrie NM, Sites E, Crawford PB. Primary care interventions to reduce childhood obesity and sugar-sweetened beverage consumption: Food for thought for oral health professionals. J Public Health Dent 2017;77(Suppl 1):S104-S127.,25Mallonee LF, Boyd LD, Stegeman C. A scoping review of skills and tools oral health professionals need to engage children and parents in dietary changes to prevent childhood obesity and consumption of sugar-sweetened beverages. J Public Health Dent 2017;77(Suppl 1):S128-S135. In the meantime, there is increasing awareness among dental professionals of their role in educating patients and parents on both dental caries and childhood obesity.36Sanghavi A, Siddiqui NJ. Advancing oral health policy and advocacy to prevent childhood obesity and reduce children’s consumption of sugar-sweetened beverages. J Public Health Dent 2017;77(Suppl 1):S88-S95.
References
- 1.Zimmerli B, Jeger F, Lussi A. Bleaching of nonvital teeth. A clinically relevant literature review. Schweiz Monatsschr Zahnmed 2010;120(4):306-20.
- 2.Brunton PA, Burke FJT, Sharif MO et al. Contemporary dental practice in the UK in 2008: Aspects of direct restorations, endodontics, and bleaching. Br Dent J 2012;212:63-7.
- 3.Demarco FF, Conde MCM, Ely C et al. Preferences on vital and nonvital tooth bleaching: A survey among dentists from a city of Southern Brazil. Braz Dent J 2013;24:527-31.
- 4.Kahler B. Present status and future directions – Managing discoloured teeth. Int Endod J 2022: Feb 21. doi: 10.1111/iej.13711.
- 5.Nutting EB, Poe GS. Chemical bleaching of discolored endodontically treated teeth. Dent Clin N Am 1967;11:655-62.
- 6.Pallarés-Serrano A, Pallarés-Serrano S, Pallarés-Serrano A, Pallarés-Sabater A. Assessment of Oxygen Expansion during Internal Bleaching with Enamel and Dentin: A Comparative In Vitro Study. Dent J 2021;9:98. https://doi.org/10.3390/dj9090098.
- 7.Estay J, Angel P, Bersezio C et al. The change of teeth color, whiteness variations and its psychosocial and self-perception effects when using low vs. high concentration bleaching gels: a one-year follow-up. BMC Oral Health 2020;20(1):255. doi: 10.1186/s12903-020-01244-x.
- 8.Haywood VB, Bergeron BE. Bleaching and the Diagnosis of Internal Resorption. Jul 24, 2018. https://decisionsindentistry.com/article/bleaching-and-the-diagnosis-of-internal-resorption/
- 9.Abbott P, Heah SY. Internal bleaching of teeth: an analysis of 255 teeth. Aust Dent J 2009;54(4):326-33. https://onlinelibrary.wiley.com/doi/epdf/10.1111/j.1834-7819.2009.01158.x.
- 10.Sakalli B, Basmaci F, Dalmizrak O. Evaluation of the penetration of intracoronal bleaching agents into the cervical region using different intraorifice barriers. BMC Oral Health 2022;22(1):266. doi: 10.1186/s12903-022-02300-4.
- 11.American Association of Endodontists Clinical Practice Committee. Use of Silver Points. AAE Position Statement. https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/silverpointsstatement.pdf#:~:text=Silver%20points%20have%20been%20shown%20to%20corrode%20spontaneously,retreatment%20and%20replacement%20of%20the%20points%20with%20another.
- 12.Savadkouhi ST, Fazlyab M. Discoloration Potential of Endodontic Sealers: A Brief Review. Iran Endod J 2016;11(4):250-4. doi: 10.22037/iej.2016.20.
- 13.Ahmed HM, Abbott PV. Discolouration potential of endodontic procedures and materials: a review. Int Endod J 2012;45(10):883-97. doi: 10.1111/j.1365-2591.2012.02071.x.
- 14.Krastl G, Allgayer N, Lenherr P et al. Tooth discoloration induced by endodontic materials: a literature review. Dent Traumatol 2013;29(1):2-7. doi: 10.1111/j.1600-9657.2012.01141.x.
- 15.Ioannidis K, Mistakidis I, Beltes P, Karagiannis V. Spectrophotometric analysis of crown discoloration induced by MTA- and ZnOE-based sealers. J Appl Oral Sci 2013;21(2):138-44. doi: 10.1590/1678-7757201302254.
- 16.Santos LGPD, Chisini LA, Springmann CG et al. Alternative to Avoid Tooth Discoloration after Regenerative Endodontic Procedure: A Systematic Review. Braz Dent J 2018;29(5):409-18. doi: 10.1590/0103-6440201802132.
- 17.Watts A, Addy M. Tooth discoloration and staining: a review of the literature. Br Dent J 2001;190:309-16.
- 18.Pink tooth of Mummery. https://medical-dictionary.thefreedictionary.com/Pink+Tooth+of+Mummery.
- 19.Haywood VB. History, safety, and effectiveness of current bleaching techniques and applications of the nightguard vital bleaching technique. Quintessence Int 1992:23:471-88. http://www.quintpub.com/userhome/qi/qi_23_7_haywood_6.pdf
- 20.Bersezio C, Ledezma P, Mayer C et al. Effectiveness and effect of non-vital bleaching on the quality of life of patients up to 6 months post-treatment: a randomized clinical trial. Clin Oral Investig 2018;22(9):3013-9. doi: 10.1007/s00784-018-2389-y.
- 21.Popescu AD, Purcarea MV, Georgescu RV et al. Vital and Non-Vital Tooth Bleaching Procedures: A Survey Among Dentists From Romania. Rom J Oral Rehab 2021;13(3):59-71. https://www.rjor.ro/wp-content/uploads/2021/10/VITAL-AND-NON-VITAL-TOOTH-BLEACHING-PROCEDURES-A-SURVEY-AMONG-DENTISTS-FROM-ROMANIA.pdf.
- 22.Zarean P, Zarean P, Ravaghi A et al. Comparison of MTA, CEM Cement, and Biodentine as Coronal Plug during Internal Bleaching: An In Vitro Study. Int J Dent 2020;2020:8896740. doi: 10.1155/2020/8896740.
- 23.Canoglu E, Gulsahi K, Sahin C et al. Effect of bleaching agents on sealing properties of different intraorifice barriers and root filling materials. Med Oral Patol Oral Cir Bucal 2012;17 (4):e710-5. http://www.medicinaoral.com/medoralfree01/v17i4/medoralv17i4p710.pdf
- 24.Amato A, Caggiano M, Pantaleo G, Amato M. In-office and walking bleach dental treatments on endodontically-treated teeth: 25 years follow-up. Minerva Stomatol 2018;67(6):225-30.
- 25.Lim MY, Lum SOY, Poh RSC et al. An in vitro comparison of the bleaching efficacy of 35% carbamide peroxide with established intracoronal bleaching agents. Int Endod J 2004;37(7):483-8. doi: 10.1111/j.1365-2591.2004.00829.x.
- 26.Yui KCK, Rodrigues JR, Mancini MNG et al. Ex vivo evaluation of the effectiveness of bleaching agents on the shade alteration of blood-stained teeth. Int Endod J 2008;41(6):485-92. doi: 10.1111/j.1365-2591.2008.01379.x.
- 27.Warren MA, Wong M, Ingram TA III. An in vitro comparison of bleaching agents on the crowns and roots of discolored teeth. J Endod 1990;16:463-7.
- 28.Rotstein I, Mor C, Friedman S. Prognosis of intracoronal bleaching with sodium perborate preparations in vitro: 1-year study. J Endod 1993;19:10-2.
- 29.Weiger R, Kuhn A, Lost C. In vitro comparison of various types of sodium perborate used for intracoronal bleaching of discolored teeth. J Endod 1994;20:338-41.
- 30.Amato M, Scaravilli MS, Farella M, Riccitiello F. Bleaching teeth treated endodontically: long-term evaluation of a case series. J Endod 2006;32:376-8.
- 31.Abou-Rass M. Long-term prognosis of intentional endodontics and internal bleaching of tetracycline-stained teeth. Compend Contin Educ Dent 1998;19:1034-44.
- 32.Anitua E, Zabalegui B, Gil J, Gascon F. Internal bleaching of severe tetracycline discolorations: four-year clinical evaluation. Quintessence Int 1990;21(10):783-8.
- 33.Gorr S-U, Brigman HV, Anderson JC, Hirsch EB. The antimicrobial peptide DGL13K is active against drug-resistant gram-negative bacteria and sub-inhibitory concentrations stimulate bacterial growth without causing resistance. PLoS ONE 2022;17(8): e0273504. https://doi.org/10.1371/journal.pone.0273504.
- 34.Peters SM, Hill NB, Halepas S. Oral manifestations of monkeypox: A report of two cases Journal of Oral and Maxillofacial Surgery (2022). https://doi.org/10.1016/j.joms.2022.07.147.
- 35.Portalatin A. Infectious disease experts call on dentists to monitor monkeypox symptoms: 6 notes. August 15, 2022. https://www.beckersdental.com/clinical-leadership-infection-control/39124-infectious-disease-experts-call-on-dentists-to-monitor-monkeypox-symptoms-6-notes.html?origin=DentalE&utm_source=DentalE&utm_medium=email&utm_content=newsletter&oly_enc_id=1694C1316967A3F.
- 36.CDC. Monkeypox. Non-Variola Orthopoxvirus and Monkeypox Virus Laboratory Testing Data. August 17, 2022. https://www.cdc.gov/poxvirus/monkeypox/response/2022/2022-lab-test.html.
- 37.CDC. Monkeypox. Prevention. https://www.cdc.gov/poxvirus/monkeypox/prevention.html.
- 38.CDC. Monkeypox and smallpox vaccine guidance. Updated June 2, 2022. https://www.cdc.gov/poxvirus/monkeypox/clinicians/index.htm.
- 39.CDC. Monkeypox. ACAM Vaccine. https://www.cdc.gov/poxvirus/monkeypox/interim-considerations/acam2000-vaccine.html.
- 40.CDC. Guidelines for Infection Control in Dental Health-Care Settings — 2003. https://www.cdc.gov/mmwr/PDF/rr/rr5217.pdf.
- 41.CDC. Infection Prevention and Control of Monkeypox in Healthcare Settings. Updated August 11, 2022. https://www.cdc.gov/poxvirus/monkeypox/clinicians/infection-control-healthcare.html
- 42.CDC. Monkeypox. Information For Veterinarians. https://www.cdc.gov/poxvirus/monkeypox/veterinarian/index.html.
- 43.CDC. Monkeypox. Pets in the Home. https://www.cdc.gov/poxvirus/monkeypox/prevention/pets-in-homes.html.
- 44.Cheng YL, Musonda J, Cheng H, et al. Effect of surface removal following bleaching on the bond strength of enamel. BMC Oral Health 2019;19(1):50.
- 45.Monteiro D, Moreira A, Cornacchia T, Magalhães C. Evaluation of the effect of different enamel surface treatments and waiting times on the staining prevention after bleaching. J Clin Exp Dent 2017;9(5):e677-81.
- 46.Rezende M, Kapuchczinski AC, Vochikovski L, et al. Staining power of natural and artificial dyes after at-home dental bleaching. J Contemp Dent Pract 2019;20(4):424-7.
- 47.Mickenautsch S, Yengopal V. Effect of xylitol versus sorbitol: a quantitative systematic review of clinical trials. Int Dent J 2012;62(4):175-88.
- 48.Rethman MP, Beltrán-Aguilar ED, Billings RJ, Burne RA, Clark M, Donly KJ, Hujoel PP, Katz BP, Milgrom P, Sohn W, Stamm JW, Watson G, Wolff M, Wright T, Zero D, Aravamudhan K, Frantsve-Hawley J, Meyer DM; for the American Dental Association Council on Scientific Affairs Expert Panel on Nonfluoride Caries-Preventive Agents. Nonfluoride caries-preventive agents. Executive summary of evidence-based clinical recommendations. J Am Dent Assoc 2011;142(9):1065-71.
- 49.Milgrom P, Söderling EM, Nelson S, Chi DL, Nakai Y. Clinical evidence for polyol efficacy. Adv Dent Res 2012; 24(2):112-6.


:sharpen(level=0):output(format=jpeg)/up/2023/05/Fiona-Collins-thumbnail-1-3.jpg)
:sharpen(level=0):output(format=jpeg)/up/2023/05/Ira-Lamster-3.jpg)
:sharpen(level=0):output(format=jpeg)/up/2018/07/The-Dangers-of-Sugar-2.jpg)