Introduction
Plain film radiolography, providing a 2-dimensional visualization of mineralized structures of the teeth and jaws, is an essential component of dental diagnosis. However, interpretation of standard radiography is limited by overlapping of anatomic structures. In contrast, introduction of digital imaging marked the beginning of a new era in interpretive visualization, which provides additional diagnostic information and therefore improved treatment planning. This has become a particularly important advance in consideration of some of the newer clinical procedures (i.e., dental implantology). Digital imaging of the head and neck (cone beam computed tomography or CBCT) uses collected digital information to reconstruct a 3-dimensional image of the anatomy.
The development and introduction of dental CBCT occurred between 1995 and 1999.1T, Ekholm M, Siiskonen T, Kortesniemi M. Dental cone beam CT: An updated review. Phys Med. 2021 Aug;88:193–217. The underlying principles of CBCT include an x-ray tube on one side of the head and an image detector on the other. As the unit rotates, there is either continuous or pulsed x-ray exposure (pulsed exposure is preferred in dental CBCT to reduce the radiation exposure). The “cone” in cone beam CT refers to the shape of the x-ray beam. The images are then reconstructed using computer algorithms, which are continuously upgraded to improve the quality of the images. Artificial intelligence is now being utilized to enhance image reconstruction.
CBCT systems are currently grouped into 3 categories, based on the field of view (FOV):
- Large: greater than 15cm scan volume height
- Medium: from 10-15 cm scan volume height
- Small: less than 10 cm scan volume height
Both standing and seated patient positioning systems are available. Selection of the appropriate system is dependent on the expected needs of the provider. Many systems are available. The review by Kassalainen and colleagues1T, Ekholm M, Siiskonen T, Kortesniemi M. Dental cone beam CT: An updated review. Phys Med. 2021 Aug;88:193–217. lists the characteristics of more than 70 systems. A comprehensive summary of the technical characteristics of the systems, as well as the underlying physics of CBCT, is provided in that review.
Use of CBCT in Clinical Dental Practice
The advantages of CBCT have led to this new diagnostic imaging being widely evaluated for application in clinical practice. In some cases, CBCT has become a standard part of patient care, while other disciplines, either limited or very targeted use is currently recommended. It is important to emphasize that while there is an inherent attraction of visualizing an anatomical structure in 3-dimenions versus 2-dimensions, the concerns of additional radiation exposure, clinical benefits and cost must be considered when deciding to use CBCT.
Implantology
In 2012, the International Congress of Oral Implantologists endorsed the use of CBCT for treatment planning for dental implants, with specific indications for making linear measurements, assessing the anatomy of the edentulous area in three dimensions, awareness and avoidance of critical anatomical structures in the surgical area, and construction of surgical guides. This statement also noted that the decision to use CBCT in cases involving implants must be based on the individual needs and conditions of the patient, and that scans should be obtained after a thorough medical-dental history has been taken, and the patient examined. Also noted was that the smallest field of view should be used, and the entire scan must be reviewed for other abnormal findings. 2E, Rios HF, Ganz SD, An CH, Resnik R, Reardon GT, et al. Use of cone beam computed tomography in implant dentistry: the International Congress of Oral Implantologists consensus report. Implant Dent. 2012 Apr;21(2):78–86.
A review of the use of CBCT in implantology, sponsored by the American Academy of Periodontology, was based on a broad review of the literature and examined use in three areas: diagnosis and assessment of outcomes, treatment planning, and characterization of the anatomy. The review stated that this technology has certain applications in implant dentistry. The authors concluded that CBCT is an adjunct to conventional 2-dimensional radiography, and concern was raised about radiation exposure. Therefore, this imaging technique is to be used when there will be clear benefits to patients.3HF, Borgnakke WS, Benavides E. The Use of Cone‐Beam Computed Tomography in Management of Patients Requiring Dental Implants: An American Academy of Periodontology Best Evidence Review. J Periodontol. 2017 Oct;88(10):946–59. Nevertheless, the use of CBCT in dental implantology has become an accepted part of diagnosis and treatment planning, especially in offices that have ready availability of that technology.
Periodontology
There are potential applications of CBCT in the diagnosis of periodontal disease. Even when considering clinical findings, a challenging aspect of traditional periodontal diagnosis is reliance on 2-dimensional radiography to visualize 3-dimensional anatomy of periodontal defects. Such knowledge can help when making the decision about retention or extraction of teeth, as well as help with pre-surgical planning when regenerative procedures are considered.
A review published in 2017 examined the literature on the use of CBCT in managing inflammatory periodontitis. 4DM, Bassir SH. When Is Cone‐Beam Computed Tomography Imaging Appropriate for Diagnostic Inquiry in the Management of Inflammatory Periodontitis? An American Academy of Periodontology Best Evidence Review. J Periodontol. 2017 Oct;88(10):978–98. Three questions were examined:
- “Clinical situation: In patients with periodontitis, what (if any) clinical situations/conditions exist when CBCT imaging improves diagnostic acumen and subsequently treatment recommendation compared with two-dimensional radiographic interpretation?”
- “Intervention: Does CBCT imaging improve the accuracy of a diagnostic assessment and establishment of a prognosis in the analysis of furcation and/or intrabony defects? Is the execution of therapy improved and facilitated, or is it therapeutically challenged?”
- “Outcomes: Does the use of CBCT imaging provide superior short-term or long-term clinical outcomes, more favorable patient-reported outcomes, or more consistent clinical treatment decisions affecting tooth prognosis (as measured by defect fill, improvements in bone anatomy, mobility patterns, and ultimate tooth survival?)”.
A total of 890 citations were reviewed, but after consideration of inclusion criteria, only 12 studies were included in the analysis. The following conclusions were reached:
- While there is limited evidence that both intrabony and furcation defects can be better visualized with CBCT, there is only limited evidence that such visualization can enhance the approach to treatment for either type of defect.
- Similarly, there is only very limited evidence that use of CBCT can enhance treatment outcome on either the short-term or long-term.
- Lastly, there is no evidence that the use of CBCT when treating intrabony or furcation defects improves patient-identified outcomes.
The authors suggested that use of CBCT in selected situations, and in limited, defined areas. This approach will limit radiation exposure to patients.
A recent review examined current and future radiographic evaluation of periodontal diseases 5R, Fontenele RC, Lahoud P, Shujaat S, Bornstein MM. Radiographic diagnosis of periodontal diseases - Current evidence versus innovations. Periodontol 2000. 2024 June;95(1):51–69. agreed with the conclusions of Kim and Bassir4DM, Bassir SH. When Is Cone‐Beam Computed Tomography Imaging Appropriate for Diagnostic Inquiry in the Management of Inflammatory Periodontitis? An American Academy of Periodontology Best Evidence Review. J Periodontol. 2017 Oct;88(10):978–98. . Radiographic assessment of periodontal disease should include 2-dimensional imaging and judicious use of CBCT. They noted the adverse effect of high-density artifacts in the CBCT images. However, they also note that in the future, use of artificial intelligence systems will enhance diagnostic accuracy of CBCT.
Endodontics
A review of the use of CBCT in clinical endodontic treatment identified a number of advantages and limitations of this application. 6F, Brown L, Parashos P. CBCT in contemporary endodontics. Aust Dent J [Internet]. 2023 June [cited 2025 Nov 3];68(S1). Available from: https://onlinelibrary.wiley.com/doi/10.1111/adj.12995 The primary advantage is improved visualization of complex anatomy in 3 dimensions (i.e., maxillary molar root canal morphology). This characteristic helps solve problems associated with 2-dimnesional radiographic visualization, specifically superimposition, and anatomic distortion. The identified limitations are the effect of artifacts in the field of view and excess/unnecessary exposure to ionizing radiation. The authors argue for consideration of benefit and risk.
The specific uses for CBCT in endodontic therapy are numerous and include:
- Identifying complex root canal morphology.
- Identification of anatomic deformities, including fractures and external root resorption.
- Anatomic evaluation prior to surgical endodontic retreatment.
- Necessary visualization of planned replantation and autotransplantation of teeth.
- Treatment of teeth with an existing root canal filling.
- Identify hard to visualize changes in the periapical area.
- Identification of calcified or previously untreated canals.
- Identification of subtle periapical changes that would not be obvious on 2-dimensional radiographs.
However, the diagnostic value of using CBCT should be considered against the following potential adverse considerations:
- Increased dose of radiation.
- No perceived benefit.
- Additional cost to the patient.
- Availability of an on-site CBCT machine (cost, space to house and shield the machine).
The evidence suggests that CBCT provides an accurate assessment of the main endodontic canals, but accuracy is reduced when identifying smaller diameter canals. This is related to the limit of spatial resolution, as well as the greater effects of even small movements when the CBCT scan is exposed. The authors concluded that a CBCT scan is unnecessary for routine, uncomplicated evaluation of the root canal system. This is also dependent on the clinical familiarity with root canal morphology and use of an operating microscope. CBCT can be useful in identifying the course of the canal in the mid and apical third of the root. CBT was of greater value when dealing with more complex internal anatomy, for example with C-shaped and acute canal curvatures, anatomic abnormalities such as taurodontism.
Indications for CBCT may include unusual or atypical anatomy and when the anatomy cannot be visualized by 2-dimensional radiography. Further, CBCT is not recommended for the identification of an apical radiolucency but can be considered when clinical evidence is conflicting. In addition, CBCT is not needed for evaluation of broken endodontic instruments in a root canal, as 2-dimensional radiography is adequate. However, CBCT does provide greater information about root perforations than 2-dimensional films. If a perforation is suspected but cannot be clearly identified using conventional radiography, use of CBCT should be considered. However, if a crack or vertical fracture is suspected, CBCT is not believed to provide greater information than 2-dimensional radiography. In these cases, clinical illumination and surgical exploration for supracentral cracks are indicated. CBCT should be considered for identification of specific location and extent for cervical root resorption. This will aid in treatment planning. CBCT is also suggested when inflammatory root resorption and external inflammatory root resorption is suspected. When acute trauma occurs, traditional radiographic and clinical information are often adequate for diagnosis. However, identification of fractures of the tooth root, which may also involve the alveolar bone, can be enhanced with CBCT. If endodontic surgery is planned, CBCT is recommended to more accurately plan the surgery, avoiding unnecessarily extending the surgical site. Patient outcomes have not been adequately addressed in reference to the benefit of using CBCT. Further, the importance of the clinician’s knowledge in the area radiographic interpretation is a particularly important consideration.
The authors 6F, Brown L, Parashos P. CBCT in contemporary endodontics. Aust Dent J [Internet]. 2023 June [cited 2025 Nov 3];68(S1). Available from: https://onlinelibrary.wiley.com/doi/10.1111/adj.12995 conclude that CBCT should be used in endodontic treatment to add to, and enhance, treatment planning. Judicious application is suggested. Further, additional longitudinal clinical research is needed to determine how the information provided by CBCT can affect the clinical outcome.
CBCT figures prominently in the discussion of the future of surgical endodontics. This imaging technique is considered an essential part of the evaluation when the goal is treatment of root-end pathology, as well as root resection and perforation repair. Combined with the dental operating microscope and piezoelectric bone surgery, the outcomes of endodontic surgery have improved. 7FC, Kratchman SI. Present status and future directions: Surgical endodontics. Int Endod J. 2022 Oct;55 Suppl 4:1020–58. Digital guided therapy is another modern approach proposed to enhance the outcome of endodontic surgery. The system, including both static guided (SG) and dynamic guided (DG) endodontics, utilizes CBCT and either a specific template (SG) or triangulation (DG) to improve endodontic access. While demonstrating positive results, clinical data is mainly provided by case studies and case series. Other clinical trials, including case-control studies with longitudinal outcomes, are needed. 8T, Weiger R, Krastl G. Present status and future directions - Guided endodontics. Int Endod J. 2022 Oct;55 Suppl 4(Suppl 4):995–1002.
Orthodontics:
A large number of orthodontic-related clinical situations have been considered as potentially benefitting from use of CBCT imaging. 9DG, Calil LR, Leal CR, Janson G. Is there a consensus for CBCT use in Orthodontics? Dent Press J Orthod. 2014;19(5):136–49. However, considering the higher dose of radiation, and that most orthodontic patients are children and young adults, CBCT is not routinely used for orthodontic diagnosis. This imaging technique should only be considered when the information gained exceeds the risks associated with increased exposure to ionizing radiation.9DG, Calil LR, Leal CR, Janson G. Is there a consensus for CBCT use in Orthodontics? Dent Press J Orthod. 2014;19(5):136–49. However, there are quite a few special clinical situations that my merit of the use of CBCT. Suggested clinical conditions that may warrant use of CBCT are “retained/impacted permanent teeth; severe craniofacial anomalies, severe facial discrepancies with indication of orthodontic-surgical treatment; and bone irregularities or malformation of TMJ accompanied by signs and symptoms.” An indication in adults is tooth movement in areas of the jaws with limited buccal-lingual width.
Another review expanded the potential indications for CBCT use in orthodontics to include contiguous structures of the dentition. These include cleft lip and cleft palate, root resorption and the presence of supernumerary teeth. Also identified were the need for maxillary expansion, concerns regarding airway morphology and obstructive sleep apnea, and the use of implants for anchorage. 10SD, Nervina JM. CBCT in orthodontics: assessment of treatment outcomes and indications for its use. Dento Maxillo Facial Radiol. 2015;44(1):20140282.
A systematic review of the use of CBCT in pediatric populations found that this imaging modality was valuable when addressing impacted canines and root fractures. Other advantages were seen for assessment of TMJ morphology and evaluation in preparation of surgery for cleft lip and cleft palate. 11Grauwe A, Ayaz I, Shujaat S, Dimitrov S, Gbadegbegnon L, Vande Vannet B, et al. CBCT in orthodontics: a systematic review on justification of CBCT in a paediatric population prior to orthodontic treatment. Eur J Orthod. 2019 Aug 8;41(4):381–9. A subsequent scoping review concluded that use of CBCT in the context of orthodontic treatment was like that reported earlier. Key issues were the clinical situation, how complicated the disorder and subsequent treatment were, and the balance between additional diagnostic information and recognized limitations of CBCT (cost, radiation exposure). 12A, Serra S, Leonardi R. Use of CBCT in Orthodontics: A Scoping Review. J Clin Med. 2024 Nov 18;13(22):6941.
As an example of utilization of CBCT in orthodontics, CBCT has been used to assess apical root resorption, a recognized complication of orthodontic treatment. Comparing patients who were treated with fixed appliances versus clear aligners, root resorption was seen more frequently with fixed appliances versus aligners (82% v. 56%; p<0.001). 13Y, Deng S, Mei L, Li Z, Zhang X, Yang C, et al. Prevalence and severity of apical root resorption during orthodontic treatment with clear aligners and fixed appliances: a cone beam computed tomography study. Prog Orthod. 2020 Jan 6;21(1):1. CBCT has also been used to assess both pre-treatment anatomy and changes in the alveolar bone related to orthodontic treatment in adults.
Oral Surgery: Extraction of Mandibular Third Molars and Orthognathic Surgery
Oral surgeons were among the first group of dental providers to embrace the use of CBCT to image structures of the head and neck.
One obvious potential use was prior to removal of mandibular third molars to improve understanding of the local anatomy and avoid injury to the inferior alveolar nerve. However, studies generally agree that compared to panoramic radiology, routine use of CBCT is not indicated for removal of third molars.
A study from Finland 14A, Apajalahti S, Vehmas T, Ventä I. Availability of CBCT and iatrogenic alveolar nerve injuries. Acta Odontol Scand. 2013 Jan;71(1):151–6. reported on national data regarding injuries to the inferior alveolar as related to extraction of mandibular third molars. Comparing the number of CBCT devices in the country, the number of CBCT examinations as well as the number of nerve injuries over a 10-year period, the number of such injuries did not change despite a marked increase in the number of CBCT exams.
Several systematic reviews of this relationship have been published comparing the incidence of alveolar nerve injury when the two imaging techniques were compared. There were no differences between panoramic and CBCT radiography in the prevalence of nerve injury, with use of panoramic radiography showing a small, non-significant advantage. 15Lhano NC, Ribeiro RA, Martins CC, Assis NMSP, Devito KL. Panoramic versus CBCT used to reduce inferior alveolar nerve paresthesia after third molar extractions: a systematic review and meta-analysis. Dento Maxillo Facial Radiol. 2020 May 1;49(4):20190265. Another systematic review concluded that both imaging techniques were comparable in identifying the chance for nerve exposure, but that use of CBCT was associated with a greater chance of predicting exposure during tooth removal. 16VCB, de Toledo Telles-Araujo G, Peralta-Mamani M, Biancardi MR, Rubira CMF, Rubira-Bullen IRF. Diagnostic accuracy of CBCT compared to panoramic radiography in predicting IAN exposure: a systematic review and meta-analysis. Clin Oral Investig. 2021 Aug;25(8):4721–33. A third systematic review 17J, Smalley KR, Ray P, Ali K. Does the addition of cone-beam CT to panoral imaging reduce inferior dental nerve injuries resulting from third molar surgery? A systematic review. BMC Oral Health. 2022 Nov 3;22(1):466. concluded that the use of CBCT (vs panoramic radiography) was not associated with a lower incidence of injury to the inferior alveolar nerve.
However, the anatomic positioning of the inferior alveolar nerve in relationship to the position of the third molar (i.e., when the nerve canal contacted the tooth root) has been shown to be predictive of the chance for nerve injury with tooth removal. 18D, Lin T, Wang Y, Sun C, Yang L, Jiang H, et al. Radiographic features of anatomic relationship between impacted third molar and inferior alveolar canal on coronal CBCT images: risk factors for nerve injury after tooth extraction. Arch Med Sci AMS. 2018 Apr;14(3):532–40. Therefore, the use of CBCT can help the clinician be aware of the risk of nerve injury and inform the patient of that risk prior to the surgery.
Further, Tay et al. 19WZ, Sklavos A, Mian M, Delpachitra S, Chandu A. Radiographic Predictors of Postoperative Inferior Alveolar Nerve Injury in Mandibular Third Molar Surgery. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg. 2025 Jan;83(1):54–61. compared panoramic radiography and CBCT to identify the risk for developing paresthesia after third molar removal. Panoramic findings including a narrow canal and bifid root structure were found to be significantly associated with paresthesia after the surgery. In contrast, no specific CBCT findings were found to be predictive of paresthesia.
Use of CBCT as part of treatment planning for removal of mandibular molars is in part governed by variables such as the experience of the clinician and cost of additional imaging. Among oral and maxillofacial surgeons, more experienced surgeons tended to rely on panoramic radiography without the use of CBCT. 20IB, Melo AR, Fernandes AV, Cunningham LL, Laureano Filho JR, Van Sickels JE. Decision making in third molar surgery: a survey of Brazilian oral and maxillofacial surgeons. Int Dent J. 2015 Aug;65(4):169–77. Further, the cost of CBCT is a concern. This imaging modality costs four-times the cost of panoramic radiography, and this would likely be added cost of panoramic radiology. 21LB, Olsen KR, Christensen J, Wenzel A. Image and surgery-related costs comparing cone beam CT and panoramic imaging before removal of impacted mandibular third molars. Dento Maxillo Facial Radiol. 2014;43(6):20140001. A report of the consensus of recognized experts in oral and maxillofacial surgery concluded that while use of CBCT for treatment planning is often used when extraction of mandibular third molars, the concluded that “CBCT radiography has…little effect on the treatment decision of the surgical intervention in comparison to panoramic radiography”. 22Y, Abir R, Manor A, Kaffe I. Are different imaging methods affecting the treatment decision of extractions of mandibular third molars? Dento Maxillo Facial Radiol. 2017 Jan;46(1):20160233.
In contrast, planning for orthognathic surgery should utilize CBCT imaging, as this modality has proven more accurate than pre-CBCT planning efforts.23A, Piffkó J, Lippold C, Segatto E. Accuracy of virtual planning in orthognathic surgery: a systematic review. Head Face Med. 2020 Dec 4;16(1):34. There is a learning curve associated with the use of CBCT for treatment planning for orthognathic surgery 24DM, Baan F, Liebregts J, Nienhuijs M, Bergé S, Maal T, et al. A learning curve in 3D virtual surgical planned orthognathic surgery. Clin Oral Investig. 2023 July;27(7):3907–15. suggesting the need for training and experience when CBCT is utilized in these situations.
CBCT has other applications in the context of head and neck anatomy and pathology. This includes visualization of the maxillary sinus, which has an obvious impact on the use of implants in the maxillary posterior regions.25AWK, Hung KF, Li DTS, Leung YY. The Use of CBCT in Evaluating the Health and Pathology of the Maxillary Sinus. Diagn Basel Switz. 2022 Nov 16;12(11):2819. Avoidance of oral-antral communication following maxillary posterior-tooth extraction is also an important adverse clinical outcome, which can be avoided with better visualization.26YT, Sun R, Wang R, Wang PP, Chen SY, Cai Y. Is CBCT Helpful in Estimating the Risk for Oroantral Communication During Maxillary Posterior Tooth Extraction? J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg. 2025 Nov;83(11):1403–12.
Conclusions:
Introduction of CBCT represents a major advance in oral and dental diagnosis and treatment planning. For decades, the dental profession has relied on 2-dimensional imaging, and now there is a means of visualizing the anatomy in 3-dimensions. Nevertheless, a risk-to-benefit calculation should be considered when deciding to use CBCT. What additional information is gained vs. cost and additional radiation exposure (see Table 1).
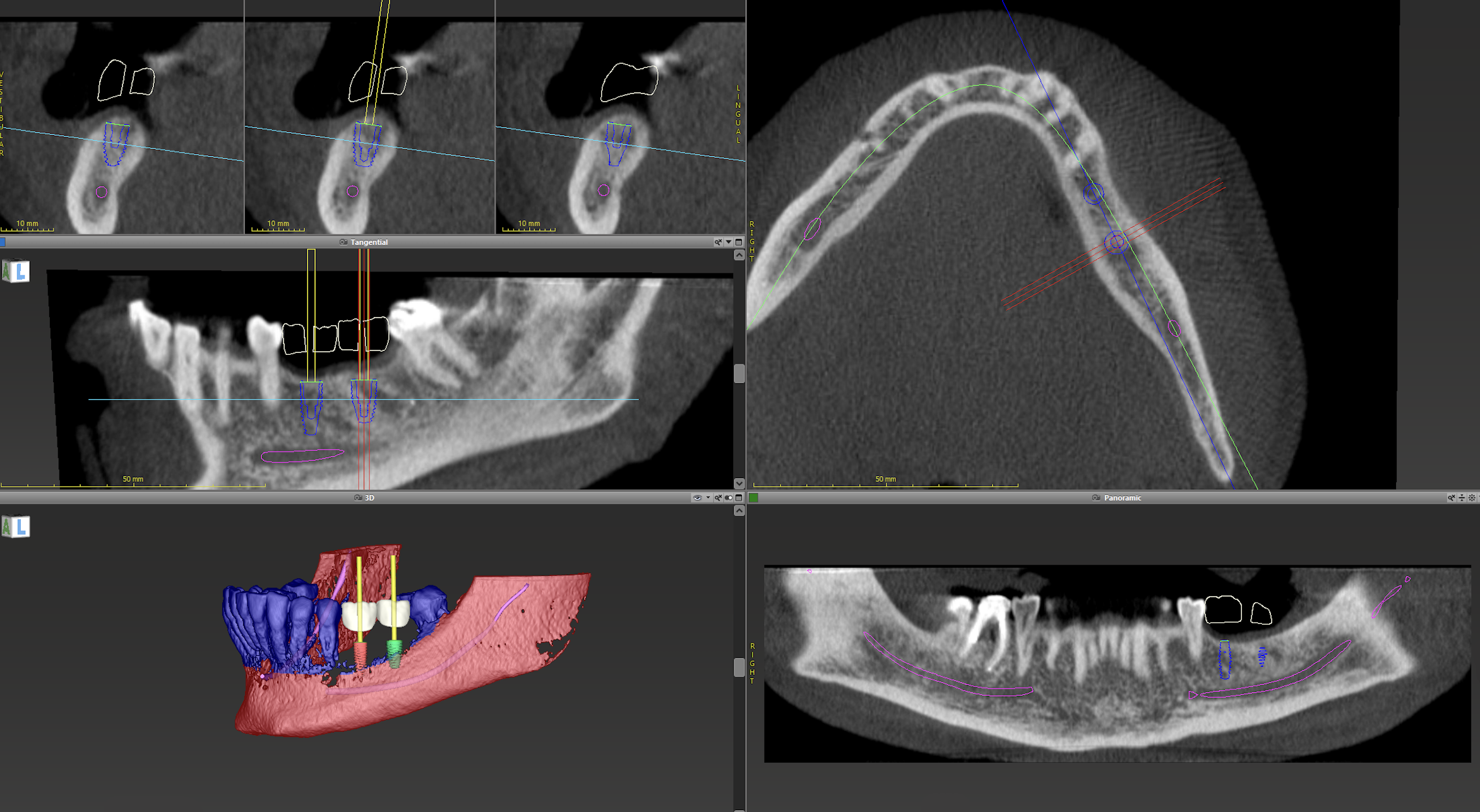
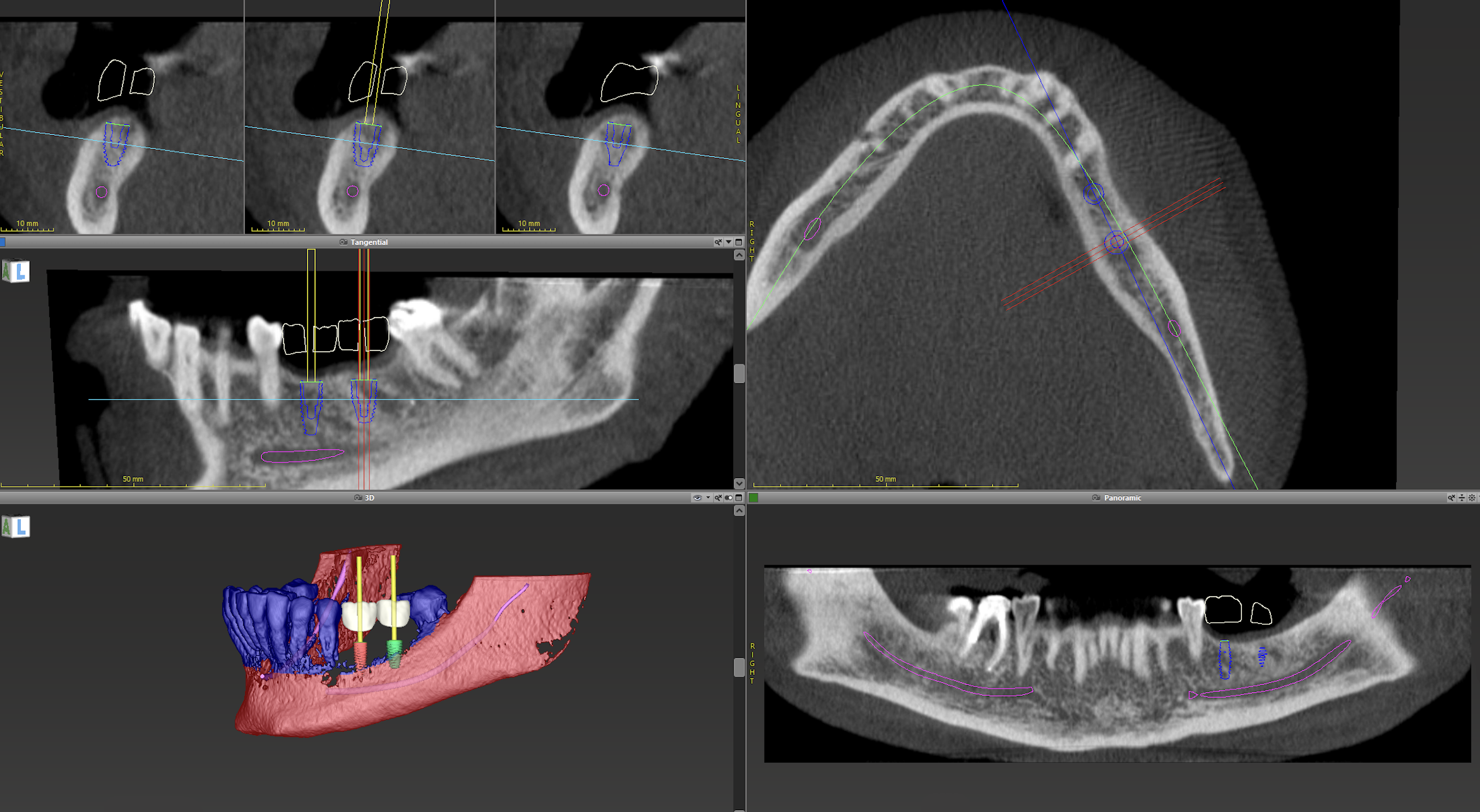
There are certain disciplines, i.e., implantology, that have embraced CBCT as key to treatment planning (see Figure 1). Future developments will likely expand the number of disciplines that regularly utilize CBCT for diagnosis and treatment planning. That will depend on future advances in limiting radiation exposure and greater availability of the technology. Unlike 2-dimensional radiography, for reasons of cost, availability, and the need for clarity as to which clinical situations would benefit from the information, CBCT radiography is not widely available in dental offices.
Diagnosis is an essential initial step in treating patients who are seen with a clinical problem. The availability of a radiographic technique that provides 3-dimensional information is a major advance. However, providers are responsible for examining all aspects of the images provided by CBCT, with the possibility of finding anatomic anomalies or unsuspected pathology that was not the original focus of the decision to obtain CBCT images. Familiarity with interpretation of these images is critical.
Both 2-dimensionl and CBCT radiography have important roles in diagnosis of oral disorders and treatment planning for dental care.27D, Telyakova V. An Overview of Cone-Beam Computed Tomography and Dental Panoramic Radiography in Dentistry in the Community. Tomogr Ann Arbor Mich. 2024 Aug 7;10(8):1222–37. Future diagnostic imaging technologies, including “artificial intelligence in the form of deep learning using convolutional neural networks, dental magnetic resonance imaging, stationary intraoral tomosynthesis, and second-generation cone-beam computed tomography sources based on carbon nanotube technology and multispectral imaging” are on the horizon and may offer even greater improvement in oral diagnostic imaging.
Dental radiology is a dynamic field, and advances in imaging (improved visualization, reduced radiation exposure) may result in even greater application of CBCT in the future. This technology offers the promise of improved diagnostic accuracy and a result the provision of more appropriate dental care.
References
- 1.T, Ekholm M, Siiskonen T, Kortesniemi M. Dental cone beam CT: An updated review. Phys Med. 2021 Aug;88:193–217.
- 2.E, Rios HF, Ganz SD, An CH, Resnik R, Reardon GT, et al. Use of cone beam computed tomography in implant dentistry: the International Congress of Oral Implantologists consensus report. Implant Dent. 2012 Apr;21(2):78–86.
- 3.HF, Borgnakke WS, Benavides E. The Use of Cone‐Beam Computed Tomography in Management of Patients Requiring Dental Implants: An American Academy of Periodontology Best Evidence Review. J Periodontol. 2017 Oct;88(10):946–59.
- 4.DM, Bassir SH. When Is Cone‐Beam Computed Tomography Imaging Appropriate for Diagnostic Inquiry in the Management of Inflammatory Periodontitis? An American Academy of Periodontology Best Evidence Review. J Periodontol. 2017 Oct;88(10):978–98.
- 5.R, Fontenele RC, Lahoud P, Shujaat S, Bornstein MM. Radiographic diagnosis of periodontal diseases - Current evidence versus innovations. Periodontol 2000. 2024 June;95(1):51–69.
- 6.F, Brown L, Parashos P. CBCT in contemporary endodontics. Aust Dent J [Internet]. 2023 June [cited 2025 Nov 3];68(S1). Available from: https://onlinelibrary.wiley.com/doi/10.1111/adj.12995
- 7.FC, Kratchman SI. Present status and future directions: Surgical endodontics. Int Endod J. 2022 Oct;55 Suppl 4:1020–58.
- 8.T, Weiger R, Krastl G. Present status and future directions - Guided endodontics. Int Endod J. 2022 Oct;55 Suppl 4(Suppl 4):995–1002.
- 9.DG, Calil LR, Leal CR, Janson G. Is there a consensus for CBCT use in Orthodontics? Dent Press J Orthod. 2014;19(5):136–49.
- 10.SD, Nervina JM. CBCT in orthodontics: assessment of treatment outcomes and indications for its use. Dento Maxillo Facial Radiol. 2015;44(1):20140282.
- 11.Grauwe A, Ayaz I, Shujaat S, Dimitrov S, Gbadegbegnon L, Vande Vannet B, et al. CBCT in orthodontics: a systematic review on justification of CBCT in a paediatric population prior to orthodontic treatment. Eur J Orthod. 2019 Aug 8;41(4):381–9.
- 12.A, Serra S, Leonardi R. Use of CBCT in Orthodontics: A Scoping Review. J Clin Med. 2024 Nov 18;13(22):6941.
- 13.Y, Deng S, Mei L, Li Z, Zhang X, Yang C, et al. Prevalence and severity of apical root resorption during orthodontic treatment with clear aligners and fixed appliances: a cone beam computed tomography study. Prog Orthod. 2020 Jan 6;21(1):1.
- 14.A, Apajalahti S, Vehmas T, Ventä I. Availability of CBCT and iatrogenic alveolar nerve injuries. Acta Odontol Scand. 2013 Jan;71(1):151–6.
- 15.Lhano NC, Ribeiro RA, Martins CC, Assis NMSP, Devito KL. Panoramic versus CBCT used to reduce inferior alveolar nerve paresthesia after third molar extractions: a systematic review and meta-analysis. Dento Maxillo Facial Radiol. 2020 May 1;49(4):20190265.
- 16.VCB, de Toledo Telles-Araujo G, Peralta-Mamani M, Biancardi MR, Rubira CMF, Rubira-Bullen IRF. Diagnostic accuracy of CBCT compared to panoramic radiography in predicting IAN exposure: a systematic review and meta-analysis. Clin Oral Investig. 2021 Aug;25(8):4721–33.
- 17.J, Smalley KR, Ray P, Ali K. Does the addition of cone-beam CT to panoral imaging reduce inferior dental nerve injuries resulting from third molar surgery? A systematic review. BMC Oral Health. 2022 Nov 3;22(1):466.
- 18.D, Lin T, Wang Y, Sun C, Yang L, Jiang H, et al. Radiographic features of anatomic relationship between impacted third molar and inferior alveolar canal on coronal CBCT images: risk factors for nerve injury after tooth extraction. Arch Med Sci AMS. 2018 Apr;14(3):532–40.
- 19.WZ, Sklavos A, Mian M, Delpachitra S, Chandu A. Radiographic Predictors of Postoperative Inferior Alveolar Nerve Injury in Mandibular Third Molar Surgery. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg. 2025 Jan;83(1):54–61.
- 20.IB, Melo AR, Fernandes AV, Cunningham LL, Laureano Filho JR, Van Sickels JE. Decision making in third molar surgery: a survey of Brazilian oral and maxillofacial surgeons. Int Dent J. 2015 Aug;65(4):169–77.
- 21.LB, Olsen KR, Christensen J, Wenzel A. Image and surgery-related costs comparing cone beam CT and panoramic imaging before removal of impacted mandibular third molars. Dento Maxillo Facial Radiol. 2014;43(6):20140001.
- 22.Y, Abir R, Manor A, Kaffe I. Are different imaging methods affecting the treatment decision of extractions of mandibular third molars? Dento Maxillo Facial Radiol. 2017 Jan;46(1):20160233.
- 23.A, Piffkó J, Lippold C, Segatto E. Accuracy of virtual planning in orthognathic surgery: a systematic review. Head Face Med. 2020 Dec 4;16(1):34.
- 24.DM, Baan F, Liebregts J, Nienhuijs M, Bergé S, Maal T, et al. A learning curve in 3D virtual surgical planned orthognathic surgery. Clin Oral Investig. 2023 July;27(7):3907–15.
- 25.AWK, Hung KF, Li DTS, Leung YY. The Use of CBCT in Evaluating the Health and Pathology of the Maxillary Sinus. Diagn Basel Switz. 2022 Nov 16;12(11):2819.
- 26.YT, Sun R, Wang R, Wang PP, Chen SY, Cai Y. Is CBCT Helpful in Estimating the Risk for Oroantral Communication During Maxillary Posterior Tooth Extraction? J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg. 2025 Nov;83(11):1403–12.
- 27.D, Telyakova V. An Overview of Cone-Beam Computed Tomography and Dental Panoramic Radiography in Dentistry in the Community. Tomogr Ann Arbor Mich. 2024 Aug 7;10(8):1222–37.
Figure 1: CBCT images as part of implant planning for a partially edentulous mandible
Images courtesy of Dr. David T. Wu, Harvard School of Dental Medicine.
1) Top left panel of 3 images: axial view of implant planning in the lower left mandible
2) Middle left panel: sagittal section - location of inferior alveolar and mental nerve in relation to implant position
3) Bottom left panel: segmentation and 3D rendering of teeth and implant position
4) Top right panel: occlusal view of mandible with implant position
5) Bottom right panel: panoramic projection with position of interior alveolar nerve and dental implant position
Table 1: Current Use of CBCT in Dentistry (1 = routine, 2 = specific use, 3 = limited)
| Discipline | Utilization |
|---|---|
| Implantology | 1 |
| Periodontics | 3 |
| Endodontics | 2 |
| Orthodontics | 2 |
| Oral Surgery: 3rd molar extractions | 3 |
| Oral Surgery: orthognathic surgery | 1 |