An Update on Tooth Whitening
The desire to improve one’s appearance, including through the removal of dental stains, has existed for hundreds of years,1A history of toothwhitening. Available at: https://www.seattletimes.com/seattle-news/health/a-history-of-tooth-whitening/. with early efforts aimed at reducing extrinsic (surface) stain, albeit often using highly abrasive materials. Extrinsic stain can be reduced and controlled through prophylaxis, brushing with an appropriate toothpaste, the incorporation of stain-inhibiting agents in toothpastes, and by avoiding coffee, tea, wine, spicy food and other substances as well as habits such as tobacco smoking and betel nut chewing.2Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.,3Sruthy Prathap H, Vinitha R, Boloor A, Rao AS. Extrinsic stains and management: A new insight. J Acad Indus Res 2013;1(8):435. ,4Savitz DA, Meyer RE, Tanzer JM, Mirvish SS, Lewin F. Public health implications of smokeless tobacco use as a harm reduction strategy. Am J Public Health 2006;96(11):1934-9. In contrast, intrinsic stain (IS) is present within the dental hard tissue and requires the use of tooth whitening (bleaching) agents.2Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16. IS can result from internalized extrinsic stain, fluorosis, hereditary conditions, systemic diseases, enamel hypoplasia, medications, trauma and dental materials.3Sruthy Prathap H, Vinitha R, Boloor A, Rao AS. Extrinsic stains and management: A new insight. J Acad Indus Res 2013;1(8):435. In addition, aging results in a yellowed appearance and changes in tooth surface morphology make teeth appear darker.5Ten Bosch JJ, Coops CC. Tooth color and reflectance as related to light scattering and enamel hardness. J Dent Res 1995;74:374-80.
Treatment options
Tooth whitening was introduced for the removal of intrinsic stain more than three decades ago and has become one of the most frequently requested and performed esthetic procedures in dentistry.6Plotino G, Buono L, Grande NM, et al. Nonvital tooth bleaching: a review of the literature and clinical procedures. J Endod 2008;34(4):394-407. In-office and at-home whitening (IO; AH) can be performed with gels containing hydrogen peroxide (HP), or carbamide peroxide (CP) which breaks down into HP and urea (e.g., 20% CP breaks down into 6% HP and 14% urea). While beyond the scope of this article, the ‘walking bleach’ method used to treat endodontically-treated discolored teeth also involves the use of hydrogen peroxide.7American Dental Association, ADA Council on Scientific Affairs. Tooth whitening/bleaching: Treatment considerations for dentists and their patients. 2009, revised 2010. Available at: https://www.ada.org/~/media/ADA/About%20the%20ADA/Files/ada_house_of_delegates_whitening_report.ashx IO is typically performed with 25% to 40% HP gels and may be assisted by light, lasers or ionic technology. Home-use products contain lower concentrations, typically ranging from 10% to 33% CP and up to 14% HP. These include dentist-supervised take-home tooth whitening kits with custom trays and unit-dose disposable trays; ionic technology and most recently an extended contact rapid dry-on film containing hydrogen peroxide; store- and internet-sourced gels, strips, and disposable trays.8Pinto MM, Gonçalves ML, Mota AC, et al. Controlled clinical trial addressing teeth whitening with hydrogen peroxide in adolescents: a 12-month follow-up. Clinics (Sao Paulo) 2017;72(3):161-70. ,9Carlos NR, Bridi EC, Amaral F, et al. Efficacy of home-use bleaching agents delivered in customized or prefilled disposable trays: A randomized clinical trial. Oper Dent 2017;42(1):30-40.,10https://www.colgateprofessional.com/products/optic-white,11Jeong Y, Bang S, Ahn J. Evaluation of Tooth Whitening Strips’ Effectiveness and Usability. IADR abstract 0945, 2021 IADR/AADR/CADR General Session (Virtual Experience). Available at: https://iadr.abstractarchives.com/abstract/21iags-3570479/evaluation-of-tooth-whitening-strips-effectiveness-and-usability,12Peng C, Park S, de Sousa FB, et al. Enhanced teeth whitening by nanofluidic transport of hydrogen peroxide into enamel with electrokinetic flows. Dent Mater 2019 Sep 19. doi: 10.1016/j.dental.2019.08.118. Other options include the use of a varnish, and laser whitening. (Table 1)
Table 1. In-office and Home-use Whitening Options
| In-Office Options | Home-use Options |
|---|---|
| 25% to 40% HP | 10% to 33% CP |
| Light-activation | 5% to 14% HP |
| Use of enzymes | Dentist-supervised kits with trays; unit dose disposable trays |
| Laser whitening | Gels, strips, pens, disposable trays |
| LED light-activation | Extended contact formulation |
| Whitening varnish | Ionic technology |
Patient Expectations and Satisfaction
According to one survey, the majority of people believe a brighter smile leads to a happier, more successful life.13American Academy of Cosmetic Dentistry. 2012 Whitening Survey. Available at: https://aacd.com/proxy/files/Publications%20and%20Resources/Whitening%20Survey_Aug12(1).pdf. Having whiter teeth is also reported to result in more positive perceptions about an individual’s intellect, appeal and relationships, and to have a positive psychosocial impact and effect on patients’ self-perception of their smiles.14Joiner A, Luo W. Tooth colour and whiteness: A review. J Dent 2017;67S:S3-10.,15Lajnert V, Kovacevic Pavicic D, Pavlic A, Pokrajac-Bulian A, Spalj S. Smile Aesthetics Satisfaction Scale: development and validation of a new brief five-item measure of satisfaction with smile aesthetics in adults and the elderly. Int Dent J 2018;68(3):162-70.,16Angel P, Bersezio C, Estay J, et al. Color stability, psychosocial impact, and effect on self-perception of esthetics of tooth whitening using low-concentration (6%) hydrogen peroxide. Quintessence Int 2018;49(7):557-66. Simply asking patients on the medical history form if they are interested, or asking during an appointment if they have a special event that they are going to can result in patients requesting this minimally invasive and esthetically pleasing treatment. In addition, as the restrictions associated with the COVID-19 pandemic have lessened, a rise in demand for cosmetic dentistry has been seen.17Silva D. Dentists see rise in cosmetic dentistry requests as pandemic restrictions ease. June 16, 2021. Available at: https://www.nbcnews.com/news/us-news/dentists-see-rise-cosmetic-dentistry-requests-pandemic-restrictions-ease-n1271005. Dental hygienists can advise patients during routine prophylaxis and discuss whitening options.
Expectations must be managed, and misconceptions dispelled to avoid patient dissatisfaction. Tooth color varies by individual and some dentitions whiten more than others.18Rezende M, Loguercio AD, Kossatz S, Reis A. Predictive factors on the efficacy and risk/intensity of tooth sensitivity of dental bleaching: A multi regression and logistic analysis. J Dent 2016;45:1-6. Generally, greater whitening has been observed for teeth that are darker at baseline and for younger patients.18Rezende M, Loguercio AD, Kossatz S, Reis A. Predictive factors on the efficacy and risk/intensity of tooth sensitivity of dental bleaching: A multi regression and logistic analysis. J Dent 2016;45:1-6. Promising an improvement based on a specific number of shades is ill-advised. In addition, extended tooth whitening over a period of months may be required for patients with resistant IS, such as tetracycline stains.19Botelho MG, Chan AWK, Newsome PRH, McGrath CP, Lam WYH. A randomized controlled trial of home bleaching of tetracycline-stained teeth. J Dent 2017;67:29-35. (Figure 1) Treatment options and their efficacy, potential duration of treatment, cost, shade mismatch of pre-existing restorations after whitening, side effects and their prevention and management should be discussed. Patients should also be aware that relapse may occur over time and can reversed with additional whitening.20Kwon SR, Wertz PW. Review of the mechanism of tooth whitening. J Esthet Restor Dent 2015;27(5):240-57.
IO and AH are safe when properly performed, routinely provided for adults and can benefit children and adolescents.7American Dental Association, ADA Council on Scientific Affairs. Tooth whitening/bleaching: Treatment considerations for dentists and their patients. 2009, revised 2010. Available at: https://www.ada.org/~/media/ADA/About%20the%20ADA/Files/ada_house_of_delegates_whitening_report.ashx,21American Association of Pediatric Dentists. Council on Clinical Affairs. Policy on the use of dental bleaching for child and adolescent patients. Revised 2019. Available at: https://www.aapd.org/media/Policies_Guidelines/P_Bleaching.pdf Tooth whitening is not recommended for the primary or mixed dentition, and young patients should be supervised.21American Association of Pediatric Dentists. Council on Clinical Affairs. Policy on the use of dental bleaching for child and adolescent patients. Revised 2019. Available at: https://www.aapd.org/media/Policies_Guidelines/P_Bleaching.pdf Dentist-supervised tooth whitening is recommended as part of an overall treatment plan, and enables the management of any side effects.7American Dental Association, ADA Council on Scientific Affairs. Tooth whitening/bleaching: Treatment considerations for dentists and their patients. 2009, revised 2010. Available at: https://www.ada.org/~/media/ADA/About%20the%20ADA/Files/ada_house_of_delegates_whitening_report.ashx,21American Association of Pediatric Dentists. Council on Clinical Affairs. Policy on the use of dental bleaching for child and adolescent patients. Revised 2019. Available at: https://www.aapd.org/media/Policies_Guidelines/P_Bleaching.pdf Defective restorations and dental caries should be treated prior to whitening. The stain’s etiology, prognosis, treatment efficacy, patient preference, cost and predicted compliance are considerations in determining how to treat a patient. Whitening kiosks/spas where unsupervised whitening occurs also exist. Options that are not dentist-supervised are not recommended.7American Dental Association, ADA Council on Scientific Affairs. Tooth whitening/bleaching: Treatment considerations for dentists and their patients. 2009, revised 2010. Available at: https://www.ada.org/~/media/ADA/About%20the%20ADA/Files/ada_house_of_delegates_whitening_report.ashx
Mechanism of action for HP
Stain molecules contain chromophores bonded together by carbon double bonds. During tooth whitening, HP diffuses into tooth structure through enamel nanopores approximately 2 to 6 nanometers in diameter and then interacts with stain molecules.12Peng C, Park S, de Sousa FB, et al. Enhanced teeth whitening by nanofluidic transport of hydrogen peroxide into enamel with electrokinetic flows. Dent Mater 2019 Sep 19. doi: 10.1016/j.dental.2019.08.118.,20Kwon SR, Wertz PW. Review of the mechanism of tooth whitening. J Esthet Restor Dent 2015;27(5):240-57. HP breaks down, producing free radicals that break the double bonds in stain molecules, thereby altering light absorption and reflection of light, and rendering teeth whiter in appearance. HP oxidizes organic material changing it into more opaque and whiter material.18Rezende M, Loguercio AD, Kossatz S, Reis A. Predictive factors on the efficacy and risk/intensity of tooth sensitivity of dental bleaching: A multi regression and logistic analysis. J Dent 2016;45:1-6.
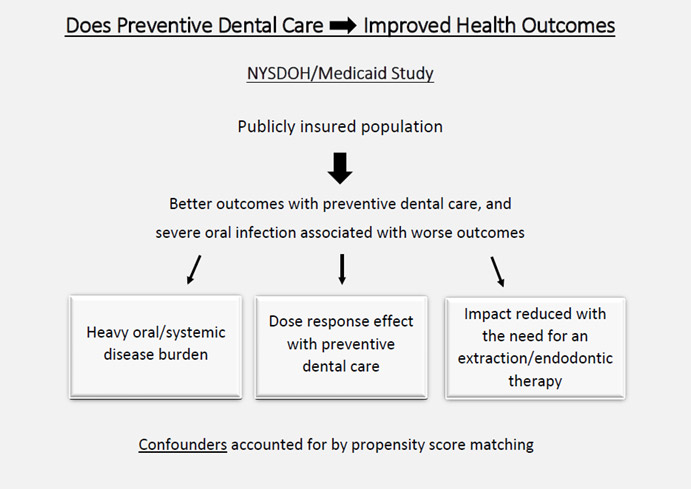
Measuring and Communicating Shade Changes
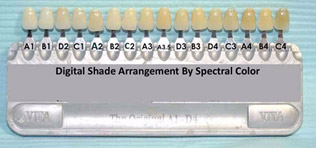
Options for measuring shade (color and whiteness) prior to, during and at the conclusion of tooth whitening include shade guides, spectrophotometers, colorimeters, spectroradiometers and digital imaging systems.14Joiner A, Luo W. Tooth colour and whiteness: A review. J Dent 2017;67S:S3-10. A Vita Classical shade guide is often used in the dental office with the 16 shades rearranged, or a Vita Bleachedguide 3D-MASTER with 29 shades may be used. (Figures 2,3)
- Figure 2. Vita Classic rearranged for whitening assessment
- Figure 3. Vita Bleachedguide 3D-MASTER
Keeping a record of the baseline shade as well as an image with the patient smiling and a pre-whitening intraoral image allows for comparison with post-whitening images. Patients may no longer remember the original shade/think there has not been much change. Taking before and after images and showing these on a computer/tablet/iPad lets patients see the difference side-by-side, in turn helping to manage patient satisfaction.
Efficacy of HP and CP gels
IO, AH and combination treatments are equally effective in achieving the end result. (Figure 3) However, IO, or a combination of IO and AH, are generally faster than AH alone. A mean shade change of 3 is reported for one 45-minute treatment with 35% HP.18Rezende M, Loguercio AD, Kossatz S, Reis A. Predictive factors on the efficacy and risk/intensity of tooth sensitivity of dental bleaching: A multi regression and logistic analysis. J Dent 2016;45:1-6. In a randomized controlled trial with 75 subjects, treatment effect was the same for AH with 10% HP used one hour/day for 15 days, IO with 40% HP used 40 minutes daily for 3 days, and one IO session of 30 minutes followed by 15 days of AH.22Dourado Pinto AV, Carlos NR, Amaral FLBD, et al. At-home, in-office and combined dental bleaching techniques using hydrogen peroxide: Randomized clinical trial evaluation of effectiveness, clinical parameters and enamel mineral content. Am J Dent 2019;32(3):124-32. The combination treatment was the fastest. In another study, no between-treatment differences in color change were observed for 35% and 38% HP and 10% and 20% CP gels.23Basting RT, Amaral FL, França FM, Flório FM. Clinical comparative study of the effectiveness of and tooth sensitivity to 10% and 20% carbamide peroxide home-use and 35% and 38% hydrogen peroxide in-office bleaching materials containing desensitizing agents. Oper Dent 2012;37(5):464-73. Other studies corroborate these findings.24de Geus JL, Wambier LM, Kossatz S, Loguercio AD, Reis A. At-home vs in-office bleaching: A systematic review and meta-analysis. Oper Dent 2016;41(4):341-56.,25Vaez SC, Correia A, Santana TR, et al. Is a single preliminary session of in-office bleaching beneficial for the effectiveness of at-home tooth bleaching? A randomized controlled clinical trial. Oper Dent 2019;44(4):E180-89.
Studies comparing light-activated and light-free tooth whitening are heterogeneous. Greater efficacy has been reported for light-activated whitening.14Joiner A, Luo W. Tooth colour and whiteness: A review. J Dent 2017;67S:S3-10.,26Park S, Kwon SR, Qian F, Wertz PW. The effect of delivery system and light activation on tooth whitening efficacy and hydrogen peroxide penetration. J Esthet Restor Dent 2016;28(5):313-20.14,26 However, in several systematic reviews, no color change differences or in the rate of whitening were found for light-activated and light-free whitening.27Maran BM, Burey A, de Paris Matos T, Loguercio AD, Reis A. In-office dental bleaching with light vs. without light: A systematic review and meta-analysis. J Dent 2018;70:1-13.,28Maran BM, Ziegelmann PK, Burey A, et al. Different light-activation systems associated with dental bleaching: a systematic review and a network meta-analysis. Clin Oral Investig 2019;23(4):1499-1512.,29SoutoMaior JR, de Moraes S, Lemos C, et al. Effectiveness of light sources on in-office dental bleaching: A systematic review and meta-analyses. Oper Dent 2019;44(3):E105-17.
In other research, electrokinetic energy was shown to drive HP gel into enamel nanopores to a greater depth than through standard diffusion-based infiltration.12Peng C, Park S, de Sousa FB, et al. Enhanced teeth whitening by nanofluidic transport of hydrogen peroxide into enamel with electrokinetic flows. Dent Mater 2019 Sep 19. doi: 10.1016/j.dental.2019.08.118. This method uses 35% and 9% HP for IO and AH, respectively. A conducting gel is placed on the occlusal and lingual surfaces of the proprietary tray and the based and catalyst HP gel is mixed in the syringe and placed in the tray on the facial aspect. All gel has to be in contact with the teeth. After switching it on, the device is operated for 30 minutes. It was found that the same shade changes occurred in vitro in 1 hour using this ionic technology as with 3 hours of whitening using a standard technique.
Extended contact formulation
A unique formulation has been introduced that utilizes 6% hydrogen peroxide together with potassium nitrate, contained in a pen for precise application to the tooth surface.10https://www.colgateprofessional.com/products/optic-white Following its application, the solution rapidly dries leaving a thin peroxide-laden film that stays on the surface of the tooth until it is removed and is not affected by exposure to water or saliva. No tray is required, reducing mess and potential discomfort. After the serum has dried, a short wavelength LED device is placed over the teeth for 10 minutes. This delivers a high level of energy, increasing penetration of the hydrogen peroxide into the teeth and reducing the overall time required for whitening.10https://www.colgateprofessional.com/products/optic-white After removing the LED device, the film continues to work while the patient is asleep and is removed during brushing the next morning. This whitening method has been shown in clinical research to significantly whiten teeth in 5 days (Figure 4a,b) and is designed for no sensitivity.
- Figure 4a. Pre-treatment shade (17 Vita Bleachedguide 3D) in a pre-orthodontic patient
- Figure 4b. Shade following 5 days of treatment (7 Vita Bleachedguide 3D)
Images courtesy of Dr. Sibel Antonson
Avoiding and Mitigating Potential Side Effects
Dental sensitivity is the most common side effect of tooth whitening, and reported to occur in from 8% to 66% of patients receiving toothwhitening.21American Association of Pediatric Dentists. Council on Clinical Affairs. Policy on the use of dental bleaching for child and adolescent patients. Revised 2019. Available at: https://www.aapd.org/media/Policies_Guidelines/P_Bleaching.pdf Systematic reviews have confirmed that higher-concentration gels can result in greater risk for sensitivity. However, in a third review no differences in risk were found for high- and low-concentration gels.18Rezende M, Loguercio AD, Kossatz S, Reis A. Predictive factors on the efficacy and risk/intensity of tooth sensitivity of dental bleaching: A multi regression and logistic analysis. J Dent 2016;45:1-6.,24de Geus JL, Wambier LM, Kossatz S, Loguercio AD, Reis A. At-home vs in-office bleaching: A systematic review and meta-analysis. Oper Dent 2016;41(4):341-56.,27Maran BM, Burey A, de Paris Matos T, Loguercio AD, Reis A. In-office dental bleaching with light vs. without light: A systematic review and meta-analysis. J Dent 2018;70:1-13. Results of a review of laser-activated whitening were equivocal.30Kikly A, Jaâfoura S, Sahtout S. Vital laser-activated teeth bleaching and postoperative sensitivity: A systematic review. J Esthet Restor Dent 2019;31(5):441-450. doi: 10.1111/jerd.12482. Study heterogeneity and small sample sizes can confound findings. In a review with a narrower range of variables, the risk of sensitivity was 51% for AH and 62.9% for IO, respectively, and lower for teeth with darker shades at baseline.18Rezende M, Loguercio AD, Kossatz S, Reis A. Predictive factors on the efficacy and risk/intensity of tooth sensitivity of dental bleaching: A multi regression and logistic analysis. J Dent 2016;45:1-6. Risk for hypersensitivity is greater for longer contact times and individuals of younger age.18Rezende M, Loguercio AD, Kossatz S, Reis A. Predictive factors on the efficacy and risk/intensity of tooth sensitivity of dental bleaching: A multi regression and logistic analysis. J Dent 2016;45:1-6.
Standard options for managing sensitivity include reducing contact time, reducing gel concentration and increasing the interval between whitening sessions. Each of these increases the duration of treatment to achieve the final result using standard techniques. Other methods to reduce the risk of, and manage, sensitivity include pre-treatment with amorphous calcium phosphate (ACP), using a gel that incorporates a desensitizer, and using a desensitizer or low-level laser therapy. IO with 30% HP followed by AH with 10% CP and use of casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) for 15 days was effective in reducing sensitivity in one study.31Oldoini G, Bruno A, Genovesi AM, Parisi L. Effects of amorphous calcium phosphate administration on dental sensitivity during in-office and at-home interventions. Dent J (Basel) 2018;6(4). pii: E52. doi: 10.3390/dj6040052. Pre-treatment with 10% ACP and IO with 30% HP followed by AH with 10% CP containing 15% ACP for 15 days, and a combination of low-level laser therapy and 5,000 ppm fluoride have also been found to be effective.31Oldoini G, Bruno A, Genovesi AM, Parisi L. Effects of amorphous calcium phosphate administration on dental sensitivity during in-office and at-home interventions. Dent J (Basel) 2018;6(4). pii: E52. doi: 10.3390/dj6040052.,32Alencar CM, De Paula BLF, Araújo JLN, et al. Effect of low-level laser therapy combined with 5000 parts per million fluoride dentifrice on postbleaching sensitivity: A clinical, randomized, and double-blind study. J Esthet Restor Dent 2018;30(4):352-9. (Table 2) Pre-treatment with anti-inflammatory and analgesic drugs has also been proposed for the prevention of sensitivity associated with in-office tooth whitening.33Santana MLC, Leal PC, Reis A, Faria-e-Silva AL. Effect of anti-inflammatory and analgesic drugs for the prevention of bleaching-induced tooth sensitivity. A systematic review and meta-analysis. J Am Dent Assoc 2019;150(10):818-29.e4. However, in a recent systematic review with 11 studies, it was concluded that this is ineffective.33Santana MLC, Leal PC, Reis A, Faria-e-Silva AL. Effect of anti-inflammatory and analgesic drugs for the prevention of bleaching-induced tooth sensitivity. A systematic review and meta-analysis. J Am Dent Assoc 2019;150(10):818-29.e4.
Table 2
| Prevention and Management of Whitening-associated Sensitivity |
|---|
| Reduce concentration of HP/CP |
| Reduce wear time |
| Increase interval between applications |
| Pre-treatment with amorphous calcium phosphate |
| Incorporation of a desensitizer into whitening gel |
| Use of a desensitizing paste/gel after whitening sessions |
| Low-level laser therapy |
| Low-level laser therapy together with 5,000 ppm fluoride |
Gingival Irritation
Gingival irritation is a less frequent occurrence, and may occur as a result of tray impingement on the gingival tissues or leakage of precise from poorly-fitting whitening trays.34Haywood VB. Nightguard vital bleaching: Current concepts and research. J Am Dent Assoc 1997;127(suppl):19S-25S. Isolation dams must be carefully applied prior to IO and trays for AH must fit well. The use of pen-applied hydrogen peroxide that rapidly dries is an option for avoiding gingival irritation since the serum application is precise and it dries before it could flow and encroach on the gingivae. (Figure 5)
Effect on Tooth Structure
In a review of 55 studies, conflicting results were found for the effect of tooth whitening on tooth structure.35Attin T, Schmidlin PR, Wegehaupt F, Wiegand A. Influence of study design on the impact of bleaching agents on dental enamel microhardness: a review. Dent Mater 2009;25(2):143-57. Immediately after whitening 51% of treatments resulted in reduced enamel hardness, while after a post-treatment interval enamel hardness was not present for 71% of treatments. In recent in vitro studies, reduced microhardness was also found.36Fukuyama M, Kawamoto C, Saikaew P, et al. Effect of topical fluoride application on enamel after in-office bleaching, as evaluated using a novel hardness tester and a transverse microradiography method. Eur J Oral Sci 2017;125(6):471-8.,37Coceska E, Gjorgievska E, Coleman NJ, et al. Enamel alteration following tooth bleaching and remineralization. J Microsc 2016;262(3):232-44.,38Crastechini E, Borges AB, Torres C. Effect of remineralizing gels on microhardness, color and wear susceptibility of bleached enamel. Oper Dent 2019;44(1):76-87. In contrast, in another study no changes in enamel topography were found with scanning electron microscopy.39Farawati FAL, Hsu SM, O'Neill E, et al. Effect of carbamide peroxide bleaching on enamel characteristics and susceptibility to further discoloration. J Prosthet Dent 2019;121(2):340-6. Under conditions similar to the intra-oral environment, i.e., using human saliva and with exposure to fluorides, fewer treatments result in reduced microhardness.35Attin T, Schmidlin PR, Wegehaupt F, Wiegand A. Influence of study design on the impact of bleaching agents on dental enamel microhardness: a review. Dent Mater 2009;25(2):143-57. Additionally, these changes can be prevented or reversed with exposure to fluorides or calcium-based technologies, and are also preventable with use of arginine carbonate and bioactive glass.40Hauss Monteiro DD, Valentim PT, Elias DC, et al. Effect of surface treatments on staining and roughness of bleached enamel. Indian J Dent Res 2019;30(3):393-8.,41Torres C, Zanatta RF, Silva TJ, Borges AB. Effect of calcium and fluoride addition to hydrogen peroxide bleaching gel on tooth diffusion, color, and microhardness. Oper Dent 2019;44(4):424-32.,42Vieira-Junior WF, Ferraz LN, Pini N, et al. Effect of toothpaste use against mineral loss promoted by dental bleaching. Oper Dent 2018;43(2):190-200. Enamel surface alterations with white circular areas observed immediately after whitening resolved within a week in a recent in vivo study with two 20-minute applications of 35% HP one week apart.43De Rosa A, Di Stasio D, Lauritano D, et al. Non-invasive analysis of bleaching effect of hydrogen peroxide on enamel by reflectance confocal microscopy (RCM): study of series of cases. Odontology 2019;107(3):285-90. It is generally recommended that enamel bonding procedures be avoided for a short period after tooth whitening due to the risk of reduced bond strength.44Cheng YL, Musonda J, Cheng H, et al. Effect of surface removal following bleaching on the bond strength of enamel. BMC Oral Health 2019;19(1):50. While tooth whitening is both safe and effective, overzealous and excessive tooth whitening can damage tooth structure.9Carlos NR, Bridi EC, Amaral F, et al. Efficacy of home-use bleaching agents delivered in customized or prefilled disposable trays: A randomized clinical trial. Oper Dent 2017;42(1):30-40. With respect to stain, three recent in vitro studies found no increase in stain propensity for teeth immersed in tea, coffee, wine, beet dye or other natural or artificial dyes after standard tooth whitening procedures.39Farawati FAL, Hsu SM, O'Neill E, et al. Effect of carbamide peroxide bleaching on enamel characteristics and susceptibility to further discoloration. J Prosthet Dent 2019;121(2):340-6.,45Monteiro D, Moreira A, Cornacchia T, Magalhães C. Evaluation of the effect of different enamel surface treatments and waiting times on the staining prevention after bleaching. J Clin Exp Dent 2017;9(5):e677-81.,46Rezende M, Kapuchczinski AC, Vochikovski L, et al. Staining power of natural and artificial dyes after at-home dental bleaching. J Contemp Dent Pract 2019;20(4):424-7.
Other considerations
Considerations include other treatment indicated based on the findings of the comprehensive examination, and whether this can best be performed before, during or after toothwhitening.10https://www.colgateprofessional.com/products/optic-white Lastly, oral hygiene instruction including avoidance of stain-inducing foods, drinks and habits will help to maintain a healthy, attractive smile after treatment.
Conclusions
Dentist-supervised whitening is recommended as part of an overall treatment plan and may include IO, AH, both or include the use of adjunctive technology. Dental hygienists can play an important role in explaining tooth whitening to patients and in practice building. Patient satisfaction is enhanced when expectations are managed, and patients understand the variables and choices in treatment. Tooth whitening has proven to be safe and effective and continues to be a requested and popular minimally invasive treatment with high levels of patient satisfaction.
References
- 1.A history of toothwhitening. Available at: https://www.seattletimes.com/seattle-news/health/a-history-of-tooth-whitening/.
- 2.Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J 2001;190:309-16.
- 3.Sruthy Prathap H, Vinitha R, Boloor A, Rao AS. Extrinsic stains and management: A new insight. J Acad Indus Res 2013;1(8):435.
- 4.Savitz DA, Meyer RE, Tanzer JM, Mirvish SS, Lewin F. Public health implications of smokeless tobacco use as a harm reduction strategy. Am J Public Health 2006;96(11):1934-9.
- 5.Ten Bosch JJ, Coops CC. Tooth color and reflectance as related to light scattering and enamel hardness. J Dent Res 1995;74:374-80.
- 6.Plotino G, Buono L, Grande NM, et al. Nonvital tooth bleaching: a review of the literature and clinical procedures. J Endod 2008;34(4):394-407.
- 7.American Dental Association, ADA Council on Scientific Affairs. Tooth whitening/bleaching: Treatment considerations for dentists and their patients. 2009, revised 2010. Available at: https://www.ada.org/~/media/ADA/About%20the%20ADA/Files/ada_house_of_delegates_whitening_report.ashx
- 8.Pinto MM, Gonçalves ML, Mota AC, et al. Controlled clinical trial addressing teeth whitening with hydrogen peroxide in adolescents: a 12-month follow-up. Clinics (Sao Paulo) 2017;72(3):161-70.
- 9.Carlos NR, Bridi EC, Amaral F, et al. Efficacy of home-use bleaching agents delivered in customized or prefilled disposable trays: A randomized clinical trial. Oper Dent 2017;42(1):30-40.
- 10.https://www.colgateprofessional.com/products/optic-white
- 11.Jeong Y, Bang S, Ahn J. Evaluation of Tooth Whitening Strips’ Effectiveness and Usability. IADR abstract 0945, 2021 IADR/AADR/CADR General Session (Virtual Experience). Available at: https://iadr.abstractarchives.com/abstract/21iags-3570479/evaluation-of-tooth-whitening-strips-effectiveness-and-usability
- 12.Peng C, Park S, de Sousa FB, et al. Enhanced teeth whitening by nanofluidic transport of hydrogen peroxide into enamel with electrokinetic flows. Dent Mater 2019 Sep 19. doi: 10.1016/j.dental.2019.08.118.
- 13.American Academy of Cosmetic Dentistry. 2012 Whitening Survey. Available at: https://aacd.com/proxy/files/Publications%20and%20Resources/Whitening%20Survey_Aug12(1).pdf.
- 14.Joiner A, Luo W. Tooth colour and whiteness: A review. J Dent 2017;67S:S3-10.
- 15.Lajnert V, Kovacevic Pavicic D, Pavlic A, Pokrajac-Bulian A, Spalj S. Smile Aesthetics Satisfaction Scale: development and validation of a new brief five-item measure of satisfaction with smile aesthetics in adults and the elderly. Int Dent J 2018;68(3):162-70.
- 16.Angel P, Bersezio C, Estay J, et al. Color stability, psychosocial impact, and effect on self-perception of esthetics of tooth whitening using low-concentration (6%) hydrogen peroxide. Quintessence Int 2018;49(7):557-66.
- 17.Silva D. Dentists see rise in cosmetic dentistry requests as pandemic restrictions ease. June 16, 2021. Available at: https://www.nbcnews.com/news/us-news/dentists-see-rise-cosmetic-dentistry-requests-pandemic-restrictions-ease-n1271005.
- 18.Rezende M, Loguercio AD, Kossatz S, Reis A. Predictive factors on the efficacy and risk/intensity of tooth sensitivity of dental bleaching: A multi regression and logistic analysis. J Dent 2016;45:1-6.
- 19.Botelho MG, Chan AWK, Newsome PRH, McGrath CP, Lam WYH. A randomized controlled trial of home bleaching of tetracycline-stained teeth. J Dent 2017;67:29-35.
- 20.Kwon SR, Wertz PW. Review of the mechanism of tooth whitening. J Esthet Restor Dent 2015;27(5):240-57.
- 21.American Association of Pediatric Dentists. Council on Clinical Affairs. Policy on the use of dental bleaching for child and adolescent patients. Revised 2019. Available at: https://www.aapd.org/media/Policies_Guidelines/P_Bleaching.pdf
- 22.Dourado Pinto AV, Carlos NR, Amaral FLBD, et al. At-home, in-office and combined dental bleaching techniques using hydrogen peroxide: Randomized clinical trial evaluation of effectiveness, clinical parameters and enamel mineral content. Am J Dent 2019;32(3):124-32.
- 23.Basting RT, Amaral FL, França FM, Flório FM. Clinical comparative study of the effectiveness of and tooth sensitivity to 10% and 20% carbamide peroxide home-use and 35% and 38% hydrogen peroxide in-office bleaching materials containing desensitizing agents. Oper Dent 2012;37(5):464-73.
- 24.de Geus JL, Wambier LM, Kossatz S, Loguercio AD, Reis A. At-home vs in-office bleaching: A systematic review and meta-analysis. Oper Dent 2016;41(4):341-56.
- 25.Vaez SC, Correia A, Santana TR, et al. Is a single preliminary session of in-office bleaching beneficial for the effectiveness of at-home tooth bleaching? A randomized controlled clinical trial. Oper Dent 2019;44(4):E180-89.
- 26.Park S, Kwon SR, Qian F, Wertz PW. The effect of delivery system and light activation on tooth whitening efficacy and hydrogen peroxide penetration. J Esthet Restor Dent 2016;28(5):313-20.
- 27.Maran BM, Burey A, de Paris Matos T, Loguercio AD, Reis A. In-office dental bleaching with light vs. without light: A systematic review and meta-analysis. J Dent 2018;70:1-13.
- 28.Maran BM, Ziegelmann PK, Burey A, et al. Different light-activation systems associated with dental bleaching: a systematic review and a network meta-analysis. Clin Oral Investig 2019;23(4):1499-1512.
- 29.SoutoMaior JR, de Moraes S, Lemos C, et al. Effectiveness of light sources on in-office dental bleaching: A systematic review and meta-analyses. Oper Dent 2019;44(3):E105-17.
- 30.Kikly A, Jaâfoura S, Sahtout S. Vital laser-activated teeth bleaching and postoperative sensitivity: A systematic review. J Esthet Restor Dent 2019;31(5):441-450. doi: 10.1111/jerd.12482.
- 31.Oldoini G, Bruno A, Genovesi AM, Parisi L. Effects of amorphous calcium phosphate administration on dental sensitivity during in-office and at-home interventions. Dent J (Basel) 2018;6(4). pii: E52. doi: 10.3390/dj6040052.
- 32.Alencar CM, De Paula BLF, Araújo JLN, et al. Effect of low-level laser therapy combined with 5000 parts per million fluoride dentifrice on postbleaching sensitivity: A clinical, randomized, and double-blind study. J Esthet Restor Dent 2018;30(4):352-9.
- 33.Santana MLC, Leal PC, Reis A, Faria-e-Silva AL. Effect of anti-inflammatory and analgesic drugs for the prevention of bleaching-induced tooth sensitivity. A systematic review and meta-analysis. J Am Dent Assoc 2019;150(10):818-29.e4.
- 34.Haywood VB. Nightguard vital bleaching: Current concepts and research. J Am Dent Assoc 1997;127(suppl):19S-25S.
- 35.Attin T, Schmidlin PR, Wegehaupt F, Wiegand A. Influence of study design on the impact of bleaching agents on dental enamel microhardness: a review. Dent Mater 2009;25(2):143-57.
- 36.Fukuyama M, Kawamoto C, Saikaew P, et al. Effect of topical fluoride application on enamel after in-office bleaching, as evaluated using a novel hardness tester and a transverse microradiography method. Eur J Oral Sci 2017;125(6):471-8.
- 37.Coceska E, Gjorgievska E, Coleman NJ, et al. Enamel alteration following tooth bleaching and remineralization. J Microsc 2016;262(3):232-44.
- 38.Crastechini E, Borges AB, Torres C. Effect of remineralizing gels on microhardness, color and wear susceptibility of bleached enamel. Oper Dent 2019;44(1):76-87.
- 39.Farawati FAL, Hsu SM, O'Neill E, et al. Effect of carbamide peroxide bleaching on enamel characteristics and susceptibility to further discoloration. J Prosthet Dent 2019;121(2):340-6.
- 40.Hauss Monteiro DD, Valentim PT, Elias DC, et al. Effect of surface treatments on staining and roughness of bleached enamel. Indian J Dent Res 2019;30(3):393-8.
- 41.Torres C, Zanatta RF, Silva TJ, Borges AB. Effect of calcium and fluoride addition to hydrogen peroxide bleaching gel on tooth diffusion, color, and microhardness. Oper Dent 2019;44(4):424-32.
- 42.Vieira-Junior WF, Ferraz LN, Pini N, et al. Effect of toothpaste use against mineral loss promoted by dental bleaching. Oper Dent 2018;43(2):190-200.
- 43.De Rosa A, Di Stasio D, Lauritano D, et al. Non-invasive analysis of bleaching effect of hydrogen peroxide on enamel by reflectance confocal microscopy (RCM): study of series of cases. Odontology 2019;107(3):285-90.
- 44.Cheng YL, Musonda J, Cheng H, et al. Effect of surface removal following bleaching on the bond strength of enamel. BMC Oral Health 2019;19(1):50.
- 45.Monteiro D, Moreira A, Cornacchia T, Magalhães C. Evaluation of the effect of different enamel surface treatments and waiting times on the staining prevention after bleaching. J Clin Exp Dent 2017;9(5):e677-81.
- 46.Rezende M, Kapuchczinski AC, Vochikovski L, et al. Staining power of natural and artificial dyes after at-home dental bleaching. J Contemp Dent Pract 2019;20(4):424-7.