Monkeypox: What we need to know
Monkeypox is the latest disease to hit the headlines in a troubling trend for emerging diseases.
The monkeypox virus (MPXV) was identified in a laboratory in 1958, and monkeypox as a disease in humans in 1970.1Brown K, Leggat PA. Human Monkeypox: Current State of Knowledge and Implications for the Future. Trop Med Infect Dis 2016;1(1):8. doi: 10.3390/tropicalmed1010008. Historically, monkeypox was confined to central and western Africa, largely the Democratic Republic of Congo and Central African Republic, where it is endemic.1Brown K, Leggat PA. Human Monkeypox: Current State of Knowledge and Implications for the Future. Trop Med Infect Dis 2016;1(1):8. doi: 10.3390/tropicalmed1010008. The first report of human monkeypox outside of Africa was in the United States in 2003, as a zoonotic disease originating in imported African rodents. The first case in the United Kingdom was transmitted from a patient to a healthcare worker in 2018 and in the same year a case was reported in Israel in an individual who had travelled from Nigeria.2Reuters. UK health care worker contracts rare monkeypox virus in third case. September 26, 2018. https://www.foxnews.com/health/uk-health-care-worker-contracts-rare-monkeypox-virus-in-third-case.,3Vaughan A, Aarons E, Astbury John et al. Two cases of monkeypox imported to the United Kingdom, September 2018. Euro Surveill 2018;23(38):pii=1800509. https://doi.org/10.2807/1560-7917.,4Petersen E, Kantele A, Koopmans M et al. Epidemiologic and Clinical Characteristics, Diagnosis, and Prevention. Infect Dis Clin North Am 2019;33(4):1027-43. doi: 10.1016/j.idc.2019.03.001.
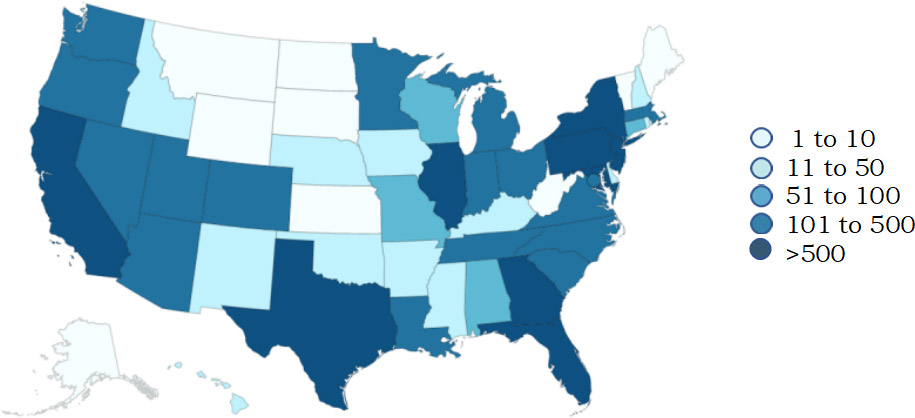
Source: Centers for Disease Control and Prevention (September 1, 2022)
The current outbreak was declared a Public Health Emergency of International Concern by the World Health Organization in July 2022.5World Health Organization. WHO Director-General declares the ongoing monkeypox outbreak a Public Health Emergency of International Concern. July 23, 2022. https://www.who.int/europe/news/item/23-07-2022-who-director-general-declares-the-ongoing-monkeypox-outbreak-a-public-health-event-of-international-concern. As of September 1, 2022 there were 52,090 confirmed cases globally, of which less than 500 are in areas where monkeypox historically has occurred.6CDC. Monkeypox. 2022 Monkeypox Outbreak Global Map. https://www.cdc.gov/poxvirus/monkeypox/response/2022/world-map.html. The first case in the United States was reported on May 15, 2022 and as of September 1, 2022 there were 19,465 confirmed cases of monkeypox.7CDC. Monkeypox. 2022 Outbreak Cases & Data. https://www.cdc.gov/poxvirus/monkeypox/response/2022/index.html. The largest number of cases has been reported in New York, California, Florida, Texas, and Georgia. (Figure 1) The vast majority of cases are in men having sex with men (MSM).7CDC. Monkeypox. 2022 Outbreak Cases & Data. https://www.cdc.gov/poxvirus/monkeypox/response/2022/index.html. What is believed to be the first death in the United States caused by MPXV was reported on August 30th, in an individual with a severely weakened immune system.8Pisani J. Texas Reports First Death of Person Diagnosed With Monkeypox. Wall Street Journal, August 30, 2022. https://www.msn.com/en-us/health/medical/texas-reports-first-death-of-person-diagnosed-with-monkeypox/ar-AA11hJ5B?ocid=msedgntp&cvid=a05972c7550846fa8f970c66b6c5322e. Globally, as of the same date 15 deaths have been reported including in other countries where monkeypox is not usually seen.
What is MPXV?
MPXV is a member of the Poxviridae family, under the Orthopox genus.9Quarleri J, Delpino MV, Galvan V. Monkeypox: considerations for the understanding and containment of the current outbreak in non-endemic countries. GeroScience 2022. https://doi.org/10.1007/s11357-022-00611-6. It is an enveloped, double-stranded DNA virus with a diameter of 200 to 250 nanometers.1Brown K, Leggat PA. Human Monkeypox: Current State of Knowledge and Implications for the Future. Trop Med Infect Dis 2016;1(1):8. doi: 10.3390/tropicalmed1010008. There are two clades (groups) within MPXV: Clade 1 (previously known as the Congo Basin Clade) and Clade 11 (previously known as the West African Clade).1Brown K, Leggat PA. Human Monkeypox: Current State of Knowledge and Implications for the Future. Trop Med Infect Dis 2016;1(1):8. doi: 10.3390/tropicalmed1010008.,10UK Health Security Guidance Agency. Guidance. High consequence infectious diseases (HCID). Guidance and information about high consequence infectious diseases and their management in England. Update August 28, 2022. https://www.gov.uk/guidance/high-consequence-infectious-diseases-hcid. Clade 1 is considered a high-consequence infectious disease in the UK.10UK Health Security Guidance Agency. Guidance. High consequence infectious diseases (HCID). Guidance and information about high consequence infectious diseases and their management in England. Update August 28, 2022. https://www.gov.uk/guidance/high-consequence-infectious-diseases-hcid. Clade 11 is less virulent. For Clade 1 the RO is between 0.6 and 1.0 and believed to be lower for Clade 11.1Brown K, Leggat PA. Human Monkeypox: Current State of Knowledge and Implications for the Future. Trop Med Infect Dis 2016;1(1):8. doi: 10.3390/tropicalmed1010008. The current monkeypox outbreak is caused by Clade 11b. Among other orthopox viruses, the most familiar are smallpox (variola) and cowpox. Since smallpox was eradicated and inoculations against smallpox ceased, the number of cases of monkeypox has increased in areas where the disease is endemic, and it is spreading. It is believed that this may be a consequence of cessation of smallpox inoculations, with increased susceptibility to monkeypox disease.11Bunge EM, Hoet B, Chen L et al. The changing epidemiology of human monkeypox-A potential threat? A systematic review. PLoS Negl Trop Dis 2022;16(2):e0010141. doi: 10.1371/journal.pntd.0010141.
Modes of Transmission
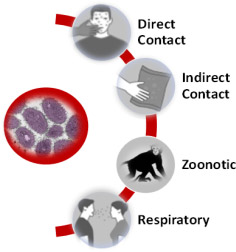
MPXV is transmitted primarily through direct contact. It can also be transmitted through indirect contact, respiratory secretions, and as a zoonotic disease.12CDC. Monkeypox. How It Spreads. Updated July 29, 2022. https://www.cdc.gov/poxvirus/monkeypox/transmission.html,13Guarner J, Johnson BJ, Paddock CD et al. Monkeypox transmission and pathogenesis in prairie dogs. Emerg Infect Dis 2004;10(3):426-31. doi: 10.3201/eid1003.030878.,14Reynolds MG, Yorita KL, Kuehnert MJ et al. Clinical manifestations of human monkeypox influenced by route of infection. J Infect Dis 2006;194(6):773-80. doi: 10.1086/505880.,15Nakouné E, Kazanji M. Monkeypox detection in maculopapular lesions in two young Pygmies in the Central African Republic. Int J Infect Dis 2012;16:e266-e267.,16Parker S, Buller RM. A review of experimental and natural infections of animals with monkeypox virus between 1958 and 2012. Future Virol 2013;8(2):129-57. doi: 10.2217/fvl.12.130. It is not known if asymptomatic transmission occurs.12CDC. Monkeypox. How It Spreads. Updated July 29, 2022. https://www.cdc.gov/poxvirus/monkeypox/transmission.html Direct human-to-human transmission is the most common mode of transmission, involving close (often intimate) contact with the source individual’s rash, scabbed pustules or body fluids (including blood).12CDC. Monkeypox. How It Spreads. Updated July 29, 2022. https://www.cdc.gov/poxvirus/monkeypox/transmission.html Transplacental transmission from mother to fetus is possible, as well as from pregnant women to babies during birth.17Meaney-Delman DM, Galang RR, Petersen BW, Jamieson DJ. A Primer on Monkeypox Virus for Obstetrician–Gynecologists. Diagnosis, Prevention, and Treatment. Obstet Gynecol 2022;140(3):391-7. ,18Kisalu NK, Mokili JL. Toward understanding the outcomes of monkeypox infection in human pregnancy. J Infect Dis 2017;216(7):795-7. (Figure 2) Potential transmission by fecal transplants has been reported, as MPXV has been found in stool samples and rectal swabs.19UPI News. FDA warns of risk of monkeypox infection from fecal transplant treatments. August 24, 2022. https://www.msn.com/en-us/health/medical/fda-warns-of-risk-of-monkeypox-infection-from-fecal-transplant-treatments/ar-AA113xb8. The US Food & Drug Administration has now issued the need for additional protections, including screening, exclusion criteria and informed consent on this risk, for investigational use of fecal transplants obtained on or after March 15, 2022.20U.S. Food & Drug Administration. Safety Alert Regarding Use of Fecal Microbiota for Transplantation and Additional Safety Protections Pertaining to Monkeypox Virus. August 22, 2022. https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/safety-alert-regarding-use-fecal-microbiota-transplantation-and-additional-safety-protections-0.
Source: Centers for Disease Control and Prevention (September 1, 2022)
Indirect contact transmission occurs via contaminated inanimate objects (fomites), such as cups, tables, bedsheets, and towels.12CDC. Monkeypox. How It Spreads. Updated July 29, 2022. https://www.cdc.gov/poxvirus/monkeypox/transmission.html Contamination of surfaces in the healthcare setting has been confirmed.21Gould S, Atkinson B, Onianwa O et al. Air and surface sampling for monkeypox virus in UK hospitals. Preprint posted July 21, 2022. doi: https://doi.org/10.1101/2022.07.21.22277864. In one study, swabs were obtained from high-touch areas in isolation rooms containing patients with monkeypox and from personal protective equipment (PPE) worn by personnel. Wide-spread contamination of surfaces was found, with 66 of 73 samples testing positive for MPXV. Positive results were also obtained for PPE used while seeing patients or changing bed linen.21Gould S, Atkinson B, Onianwa O et al. Air and surface sampling for monkeypox virus in UK hospitals. Preprint posted July 21, 2022. doi: https://doi.org/10.1101/2022.07.21.22277864.
Respiratory secretions in exhaled large droplets can spread MPXV at short distance from the source individual. It is believed that MPXV does not linger in the air.22Mandavilli A. C.D.C. Dismisses Airborne Transmission of Monkeypox. Some Experts Disagree. June 10, 2022. https://www.nytimes.com/2022/06/10/health/monkeypox-airborne.html. Aerosolized transmission has not been reported.23CDC. Monkeypox Response: Transmission. https://www.cdc.gov/media/releases/2022/0509-monkeypox-transmission.html. However, aerosolized transmission in experimental studies in monkeys has occurred.24Zaucha G, Jahrling P, Geisbert T et al. The Pathology of Experimental Aerosolized Monkeypox Virus Infection in Cynomolgus Monkeys (Macaca fascicularis). Lab Invest 2001;81:1581-600. https://doi.org/10.1038/labinvest.3780373. In the UK, MPXV is included under airborne transmission.10UK Health Security Guidance Agency. Guidance. High consequence infectious diseases (HCID). Guidance and information about high consequence infectious diseases and their management in England. Update August 28, 2022. https://www.gov.uk/guidance/high-consequence-infectious-diseases-hcid. In a study in which air samples were taken before and while changing bed linen in the isolation unit in a hospital setting, 5 of 15 samples showed contamination with MPXV and three of four taken while bed linen was being changed.21Gould S, Atkinson B, Onianwa O et al. Air and surface sampling for monkeypox virus in UK hospitals. Preprint posted July 21, 2022. doi: https://doi.org/10.1101/2022.07.21.22277864.
Zoonotic transmission occurs as a result of direct contact with an infected animal (touch, scratches or bites) and preparing/eating infected meat.1Brown K, Leggat PA. Human Monkeypox: Current State of Knowledge and Implications for the Future. Trop Med Infect Dis 2016;1(1):8. doi: 10.3390/tropicalmed1010008.,4Petersen E, Kantele A, Koopmans M et al. Epidemiologic and Clinical Characteristics, Diagnosis, and Prevention. Infect Dis Clin North Am 2019;33(4):1027-43. doi: 10.1016/j.idc.2019.03.001. Rope squirrels, giant pouched rats and dormice imported to the US in 2003 were infected, the disease was transmitted to prairie dogs, and in turn humans and a rabbit.1Brown K, Leggat PA. Human Monkeypox: Current State of Knowledge and Implications for the Future. Trop Med Infect Dis 2016;1(1):8. doi: 10.3390/tropicalmed1010008.,25Di Giulio DB, Eckburg PB. Human monkeypox: an emerging zoonosis. Lancet Infect Dis 2004;4(1):15-25. doi: 10.1016/s1473-3099(03)00856-9. Affected animals in Africa includes monkeys, chimpanzees and orangutans,1Brown K, Leggat PA. Human Monkeypox: Current State of Knowledge and Implications for the Future. Trop Med Infect Dis 2016;1(1):8. doi: 10.3390/tropicalmed1010008. and MPXV antibodies have been found in several other species. This does not, however, determine potential transmission to humans. The primary reservoir remains unknown.26Nolen LD, Osadebe L, Katomba J et al. Introduction of Monkeypox into a Community and Household: Risk Factors and Zoonotic Reservoirs in the Democratic Republic of the Congo. Am J Trop Med Hyg 2015;93(2):410-5. doi: 10.4269/ajtmh.15-0168. (Figure 2)

Source: Centers for Disease Control and Prevention (September 1, 2022)
Signs and Symptoms of Monkeypox Disease
Signs and symptoms include a rash, malaise, fever, chills, lymphadenopathy, headaches, and myalgia. An estimated 98.6% of individuals with MPVX experience a rash, considered part of the definitive diagnosis.27CDC. Monkeypox Cases by Age and Gender, Race/Ethnicity, and Symptoms. https://www.cdc.gov/poxvirus/monkeypox/response/2022/demographics.html. As shown in Figure 3, in general, for other signs and symptoms the percentage of individuals experiencing a given sign/symptom ranges from 6% to 72.7%.
Individuals are considered infectious from the onset of symptoms until the rash has resolved and skin has formed over the area. Generally, this takes 2 to 4 weeks after onset of symptoms.28CDC. Monkeypox. Signs and Symptoms. https://www.cdc.gov/poxvirus/monkeypox/symptoms.html. One percent of individuals do not experience a rash and, while multiple lesions are typical, individuals with just one lesion have been diagnosed with monkeypox. The incubation period for monkeypox ranges from 12 days to 3 weeks.28CDC. Monkeypox. Signs and Symptoms. https://www.cdc.gov/poxvirus/monkeypox/symptoms.html. Fever, fatigue, lymphadenopathy, headache, and backache occur during the prodromal phase, lasting up to 4 days.1Brown K, Leggat PA. Human Monkeypox: Current State of Knowledge and Implications for the Future. Trop Med Infect Dis 2016;1(1):8. doi: 10.3390/tropicalmed1010008. The fever subsides prior to the onset of a rash. In contrast to chickenpox, a monkeypox rash consists of lesions at various stages of development and resolution. Oral lesions are often the first signs, developing prior to skin and other potential mucosal lesions (including ocular).
Skin lesions in the facial region typically occur first before spreading out, and lesions can develop over the whole body. The lesions are typically between 2 and 5 mm in diameter, but may reach 1 cm.1Brown K, Leggat PA. Human Monkeypox: Current State of Knowledge and Implications for the Future. Trop Med Infect Dis 2016;1(1):8. doi: 10.3390/tropicalmed1010008.,29Macneil A, Reynolds MG, Braden Z et al. Transmission of atypical varicella-zoster virus infections involving palm and sole manifestations in an area with monkeypox endemicity. Clin Infect Dis 2009;48(1):e6-8. doi:10.1086/595552. After presenting as macules the lesions progress after 1 to 2 days through the stages of papules (1 to 2 days duration), vesicles containing clear fluid (1 to 2 days duration), and pustules containing opaque fluid (5 to 7 days duration).30Kaler J, Hussain A, Flores G et al. Monkeypox: A Comprehensive Review of Transmission, Pathogenesis, and Manifestation. Cureus 2022;14(7):e26531. doi: 10.7759/cureus.26531. Lesions then crust over, and the scabs later fall off. (Figure 4) Areas of hypo- and hyper-pigmentation may be evident after monkeypox lesions have healed.30Kaler J, Hussain A, Flores G et al. Monkeypox: A Comprehensive Review of Transmission, Pathogenesis, and Manifestation. Cureus 2022;14(7):e26531. doi: 10.7759/cureus.26531. Monkeypox lesions are distinct, well defined and umbilicated.
Figure 4. Stages of monkeypox rash
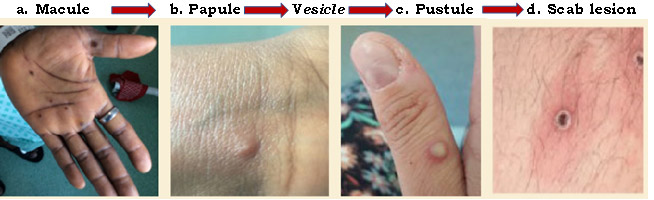
Source: a-c CDC; NHS England and High Consequence Infectious Diseases Network; d CDC; UK Health Security Agency
Most of the signs and symptoms are common to smallpox and to chickenpox (varicella).1Brown K, Leggat PA. Human Monkeypox: Current State of Knowledge and Implications for the Future. Trop Med Infect Dis 2016;1(1):8. doi: 10.3390/tropicalmed1010008.,9Quarleri J, Delpino MV, Galvan V. Monkeypox: considerations for the understanding and containment of the current outbreak in non-endemic countries. GeroScience 2022. https://doi.org/10.1007/s11357-022-00611-6. Lymphadenopathy is a key feature for monkeypox and does not occur with chickenpox or smallpox.25Di Giulio DB, Eckburg PB. Human monkeypox: an emerging zoonosis. Lancet Infect Dis 2004;4(1):15-25. doi: 10.1016/s1473-3099(03)00856-9. ,29Macneil A, Reynolds MG, Braden Z et al. Transmission of atypical varicella-zoster virus infections involving palm and sole manifestations in an area with monkeypox endemicity. Clin Infect Dis 2009;48(1):e6-8. doi:10.1086/595552. (Figure 5) It is important to note that many cases are currently presenting without typical early signs and symptoms (fever, headache, exhaustion, muscle aches and lymphadenopathy). Further, instead of widespread distribution of a rash, cases are presenting with fewer lesions and confined to specific areas of the body.31California Dental Association. Dental practices can reduce the spread of monkeypox through awareness, screening and infection control. July 19, 2022.
Potential complications of severe disease include corneal scarring with permanent loss of vision, secondary infections, pneumonitis, and encephalitis.1Brown K, Leggat PA. Human Monkeypox: Current State of Knowledge and Implications for the Future. Trop Med Infect Dis 2016;1(1):8. doi: 10.3390/tropicalmed1010008.,29Macneil A, Reynolds MG, Braden Z et al. Transmission of atypical varicella-zoster virus infections involving palm and sole manifestations in an area with monkeypox endemicity. Clin Infect Dis 2009;48(1):e6-8. doi:10.1086/595552. Very rarely, infection during pregnancy has led to miscarriage and stillbirth.17Meaney-Delman DM, Galang RR, Petersen BW, Jamieson DJ. A Primer on Monkeypox Virus for Obstetrician–Gynecologists. Diagnosis, Prevention, and Treatment. Obstet Gynecol 2022;140(3):391-7. In previous outbreaks in Africa, fatalities ranged from 1% to 10%,4Petersen E, Kantele A, Koopmans M et al. Epidemiologic and Clinical Characteristics, Diagnosis, and Prevention. Infect Dis Clin North Am 2019;33(4):1027-43. doi: 10.1016/j.idc.2019.03.001. influenced by MPXV clade, immunosuppression status, general health, and availability of care. In the current global outbreak, complications are relatively uncommon.
Oral and Oropharyngeal Manifestations
An estimated 70% of individuals with monkeypox are reported to experience intraoral lesions.32Indiana Department of Health. MONKEYPOX VIRUS. Oral Manifestations. https://www.in.gov/health/oral-health/files/22_Monkeypox-flyer-oral-health.pdf. However, in a recent retrospective case series a different presentation was found for 197 individuals with monkeypox.33Patel A, Bilinska J, Tam J C H et al. Clinical features and novel presentations of human monkeypox in a central London centre during the 2022 outbreak: descriptive case series Br Med J 2022;378:e072410. doi:10.1136/bmj-2022-072410. All were men and, all but one identified as MSM. In this cohort, oral lesions were found in a significantly lower percentage of individuals. Oral lesions can present as ulcerations or erythematous areas, on any area of oral mucosa. In one case study, a patient presented with a tan-grey ulcerated lesion 1 cm across on the tip of the tongue and smaller cluster lesions presenting as vesicles on the anterior ventral (inferior) area.34Peters SM, Hill NB, Halepas S. Oral manifestations of monkeypox: A report of two cases Journal of Oral and Maxillofacial Surgery (2022). https://doi.org/10.1016/j.joms.2022.07.147. Skin lesions developed later. A second patient presented with an ulcerated nodule 1 cm across on the tip of the tongue. Perioral lesions may also be present. In some cases, lesions have a similar appearance to herpes lesions (cold sores), trauma or hand, foot and mouth disease.35Portalatin A. Infectious disease experts call on dentists to monitor monkeypox symptoms: 6 notes. August 15, 2022. https://www.beckersdental.com/clinical-leadership-infection-control/39124-infectious-disease-experts-call-on-dentists-to-monitor-monkeypox-symptoms-6-notes.html?origin=DentalE&utm_source=DentalE&utm_medium=email&utm_content=newsletter&oly_enc_id=1694C1316967A3F. Oropharyngeal manifestations are much less common. In the retrospective case series described above, 13.7% of participants presented with oropharyngeal lesions, and 4.6% presented with redness, swelling, pustules or abscesses in the tonsillar region.32Indiana Department of Health. MONKEYPOX VIRUS. Oral Manifestations. https://www.in.gov/health/oral-health/files/22_Monkeypox-flyer-oral-health.pdf.
Role of Dental Professionals
Healthcare professionals have been ‘urged to be alert for patients who have rash illnesses consistent with monkeypox……’.31California Dental Association. Dental practices can reduce the spread of monkeypox through awareness, screening and infection control. July 19, 2022. As dental professionals, there is an opportunity to review updated medical history forms and look out for signs and symptoms that suggest monkeypox.32Indiana Department of Health. MONKEYPOX VIRUS. Oral Manifestations. https://www.in.gov/health/oral-health/files/22_Monkeypox-flyer-oral-health.pdf. This includes oral, oropharyngeal, and peri-oral lesions, as well as skin rashes. In addition, lymphadenopathy of the submandibular and cervical areas can be detected. If monkeypox is suspected, the patient needs to be referred immediately for medical investigation, testing and a definitive diagnosis. If confirmed, the patient needs to isolate and receive care. Early identification can help to prevent spread through earlier diagnosis and isolation of infected individuals.
Testing and Treatment
Non-variola orthopox/MPXV testing is available and recommended for individuals with a rash or lesions consistent with monkeypox.36CDC. Monkeypox. Non-Variola Orthopoxvirus and Monkeypox Virus Laboratory Testing Data. August 17, 2022. https://www.cdc.gov/poxvirus/monkeypox/response/2022/2022-lab-test.html. Swabs are taken from more than one lesion, with results in a few days. Polymerase chain reaction testing is performed for confirmation.36CDC. Monkeypox. Non-Variola Orthopoxvirus and Monkeypox Virus Laboratory Testing Data. August 17, 2022. https://www.cdc.gov/poxvirus/monkeypox/response/2022/2022-lab-test.html. If exposed to MPXV or at high risk, vaccination against monkeypox is recommended and preventive measures.37CDC. Monkeypox. Prevention. https://www.cdc.gov/poxvirus/monkeypox/prevention.html. Antiviral agents, including TPOXX, can be used to treat patients with monkeypox, under an Expanded Access Investigational New Drug (EA-IND) protocol.37CDC. Monkeypox. Prevention. https://www.cdc.gov/poxvirus/monkeypox/prevention.html.
Vaccines against monkeypox
The vaccine JYNNEOS is FDA-approved against monkeypox (and smallpox) in individuals 18 years-of-age and older and administered as two subcutaneous injections 28 days apart.38CDC. Monkeypox and smallpox vaccine guidance. Updated June 2, 2022. https://www.cdc.gov/poxvirus/monkeypox/clinicians/index.htm. Peak immunity is attained 14 days after the second dose. The vaccine is contraindicated during pregnancy and while breastfeeding. It is also in short supply and is now being used in the US at a 20% dose and given intradermally. The alternative is the ACAM2000 vaccine, which is effective against smallpox. Vaccines against smallpox provide cross-immunity for monkeypox, however there is no efficacy data available in the current outbreak.38CDC. Monkeypox and smallpox vaccine guidance. Updated June 2, 2022. https://www.cdc.gov/poxvirus/monkeypox/clinicians/index.htm. ACAM2000 is available against monkeypox under an EA-IND application.39CDC. Monkeypox. ACAM Vaccine. https://www.cdc.gov/poxvirus/monkeypox/interim-considerations/acam2000-vaccine.html. ACAM2000 should not administered in people who are pregnant or have a weakened immune system or skin conditions such as eczema. More information can be found on the CDC website, including contraindications and potential adverse events.
Infection Control
It is essential to follow infection control protocols to minimize the risk of transmission for all diseases. As part of general infection control guidance, standard precautions are required to prevent the transmission of microorganisms and disease.40CDC. Guidelines for Infection Control in Dental Health-Care Settings — 2003. https://www.cdc.gov/mmwr/PDF/rr/rr5217.pdf. For patient care, this includes appropriate hand hygiene, and PPE consisting of clinical attire, single-use disposable gloves, a face shield that wraps around the face or goggles, and a mask. Transmission-based and stepped-up precautions have additional requirements, including wearing an N95 respirator (or equivalent in other locations).
Patients with confirmed monkeypox or already suspected should be isolating (and as such not visiting a dental office). Patients should be screened prior to any appointment for signs and symptoms suggesting monkeypox infection, and for contacts/potential exposure. In addition, during patient appointments, dental professionals should be alert for signs and symptoms of monkeypox and a history suggesting exposure. It has been noted that aerosol-generating procedures can put dental healthcare personnel at risk of contracting monkeypox when treating patients with suspected or confirmed monkeypox.32Indiana Department of Health. MONKEYPOX VIRUS. Oral Manifestations. https://www.in.gov/health/oral-health/files/22_Monkeypox-flyer-oral-health.pdf.
It is in general recommended for healthcare professionals to wear an N95 respirator (FFP3 or equivalent in other countries) when treating a patient with suspected (or confirmed) monkeypox.41CDC. Infection Prevention and Control of Monkeypox in Healthcare Settings. Updated August 11, 2022. https://www.cdc.gov/poxvirus/monkeypox/clinicians/infection-control-healthcare.html
Considerations for pets and animals
The CDC has advised that ‘veterinarians should consider all mammals susceptible to monkeypox’.42CDC. Monkeypox. Information For Veterinarians. https://www.cdc.gov/poxvirus/monkeypox/veterinarian/index.html. The CDC also advises individuals with monkeypox to avoid contact with pets, domestic animals, and wildlife to prevent transmission.43CDC. Monkeypox. Pets in the Home. https://www.cdc.gov/poxvirus/monkeypox/prevention/pets-in-homes.html. If an infected individual did not have direct contact with pets prior to the onset of symptoms, it is recommended that someone else in another home should look after the pet until the individual has recovered. If it is impossible to avoid caring for pets, the infected individual must avoid direct contact with pets and make sure that they cannot come into contact with contaminated inanimate objects. Advice includes wearing long sleeves and long pants to cover any rash, performing hand hygiene, and wearing gloves and a well-fitting mask or respirator while caring for the pet. More details can be found on the CDC website.43CDC. Monkeypox. Pets in the Home. https://www.cdc.gov/poxvirus/monkeypox/prevention/pets-in-homes.html.
Conclusions
Transmission during the current outbreak is largely by direct contact and infectivity is relatively low. While most cases at this time are in MSM, this does not mean that monkeypox cannot be transmitted to other individuals. Identification, tracing, and isolation are important in combatting transmission. In addition, healthcare professionals need to be alert for a history, signs and symptoms suggestive of monkeypox when seeing patients. Dental professionals are uniquely qualified to identify oral and peri-oral lesions, as well as oropharyngeal lesions. As such, dental professionals can play a significant role in the early identification and referral for testing of individuals suspected of having monkeypox. Early identification of potential cases together with earlier isolation for suspected and confirmed cases lead to reduced opportunity for further transmission.
References
- 1.Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr 2017;17(1):230.doi: 10.1186/s12877-017-0621-2.
- 2.Delara M, Murray L, Jafari B et al. Prevalence and factors associated with polypharmacy: a systematic review and meta-analysis. BMC Geriatr 2022;22:601. https://doi.org/10.1186/s12877-022-03279-x.
- 3.Salive ME. Multimorbidity in older adults. Epidemiol Rev 2013:1-9.
- 4.Błeszyńska-Marunowska E, Jagiełło K, Grodzicki T et al. Prevalence, predisposing factors and strategies to reduce polypharmacy among older patients in Poland. Pol Arch Intern Med 2022 Sep 28:16347. doi: 10.20452/pamw.16347.
- 5.Thomson WM, Ferguson CA, Janssens BE et al. Xerostomia and polypharmacy among dependent older New Zealanders: a national survey. Age and Ageing 2021;50(1):248-51. https://doi.org/10.1093/ageing/afaa099.
- 6.Remelli F, Ceresini MG, Trevisan C et al. Prevalence and impact of polypharmacy in older patients with type 2 diabetes. Aging Clin Exp Res 2022;34(9):1969-83. doi: 10.1007/s40520-022-02165-1.
- 7.Loya AM, Gonzalez-Stuart A, Rivera JO. Prevalence of polypharmacy, polyherbacy, nutritional supplement use and potential product interactions among older adults living on the United States-Mexico border: a descriptive, questionnaire-based study. Drugs Aging 2009;26:423-36.
- 8.Desai M, Park T. Deprescribing practices in Canada: A scoping review. Can Pharm J (Ott) 2022;155(5):249-57. doi: 10.1177/17151635221114114.
- 9.Marengoni A, Angleman S, Melis R et al. Aging with multimorbidity: A systematic review of the literature. Ageing Res Rev 2011;10(4):430-9. https://doi.org/10.1016/j.arr.2011.03.003.
- 10.Betts AC, Murphy CC, Shay LA et al. Polypharmacy and medication fill nonadherence in a population-based sample of adolescent and young adult cancer survivors, 2008-2017. J Cancer Surviv 2022 Nov 8. doi: 10.1007/s11764-022-01274-0. [Epub ahead of print]
- 11.Cheng JJ, Azizoddin AM, Maranzano MJ et al. Polypharmacy in Oncology. Clin Geriatr Med 2022;38(4):705-14. doi: 10.1016/j.cger.2022.05.010.
- 12.Xie L, Gelfand A, Murphy CC et al. Prevalence of polypharmacy and associated adverse outcomes and risk factors among children with asthma in the USA: a cross-sectional study. BMJ Open 2022;12(10):e064708. doi: 10.1136/bmjopen-2022-064708.
- 13.Feinstein JA, Feudtner C, Kempe A, Orth LE. Anticholinergic Medications and Parent-Reported Anticholinergic Symptoms in Neurologically Impaired Children. J Pain Symptom Manage 2022:S0885-3924(22)00952-6. doi: 10.1016/j.jpainsymman.2022.10.013.
- 14.Ikram M, Shaikh NF, Sambamoorthi U. A Linear Decomposition Approach to Explain Excess Direct Healthcare Expenditures Associated with Pain Among Adults with Osteoarthritis. Health Serv Insights 2022;15:11786329221133957. doi: 10.1177/11786329221133957.
- 15.Aguglia A, Natale A, Fusar-Poli L et al. Complex polypharmacy in bipolar disorder: Results from a real-world inpatient psychiatric unit. Psychiatry Res 2022;318:114927. doi: 10.1016/j.psychres.2022.114927.
- 16.Bevilacqua KG, Brinkley C, McGowan J et al. “We are Getting Those Old People Things.” Polypharmacy Management and Medication Adherence Among Adult HIV Patients with Multiple Comorbidities: A Qualitative Study. Patient Prefer Adherence 2022;16:2773-80. doi: 10.2147/PPA.S382005.
- 17.Chertcoff A, Ng HS, Zhu F et al. Polypharmacy and multiple sclerosis: A population-based study. Mult Scler 2022:13524585221122207. doi: 10.1177/13524585221122207. [Epub ahead of print]
- 18.Ye L, Yang-Huang J, Franse CB et al. Factors associated with polypharmacy and the high risk of medication-related problems among older community-dwelling adults in European countries: a longitudinal study. BMC Geriatr 2022;22(1):841. doi: 10.1186/s12877-022-03536-z.
- 19.Davies LE, Spiers G, Kingston A et al. Adverse outcomes of polypharmacy in older people: systematic review of reviews. J Am Med Dir Assoc 2020;21(2):181–7. https://doi.org/10.1016/j.jamda.2019.10.022.
- 20.French DD, Campbell R, Spehar A et al. Outpatient Medications and Hip Fractures in the US. Drugs Aging 2005;22:877-85. https://doi.org/10.2165/00002512-200522100-00006.
- 21.Leelakanok N, Holcombe AL, Lund BC et al. Association between polypharmacy and death: A systematic review and meta-analysis. J Am Pharm Assoc (2003) 2017;57(6):729-38.e10. doi: 10.1016/j.japh.2017.06.002.
- 22.Hilmer SN, Gnjidic D. The anticholinergic burden: from research to practice. Aust Prescr 2022;45(4):118-20. doi: 10.18773/austprescr.2022.031.
- 23.Mur J, Cox SR, Marioni RE et al. Increase in anticholinergic burden from 1990 to 2015: Age-period-cohort analysis in UK biobank. Br J Clin Pharmacol 2022;88(3):983-93. doi: 10.1111/bcp.15045.
- 24.Porcheri C, Mitsiadis TA. Physiology, Pathology and Regeneration of Salivary Glands. Cells 2019;8(9):976. doi: 10.3390/cells8090976.
- 25.Bostock C, McDonald C. Antimuscarinics in Older People: Dry Mouth and Beyond. Dent Update 2016;43(2):186-8, 191. doi: 10.12968/denu.2016.43.2.186.
- 26.Yuan A, Woo SB. Adverse Drug Events in the Oral Cavity. Oral Surg Oral Med Oral Pathol Oral Radiol 2015;119(1):35-47.
- 27.Tan ECK, Lexomboon D, Sandborgh-Englund G et al. Medications That Cause Dry Mouth As an Adverse Effect in Older People: A Systematic Review and Metaanalysis. J Am Geriatr Soc 2018;66(1):76-84. doi: 10.1111/jgs.15151.
- 28.Singh MS, Papas A. Oral Implications of Polypharmacy in the Elderly. Dent Clin N Am 2014;58:783-96. http://dx.doi.org/10.1016/j.cden.2014.07.004.
- 29.Scully C. Drug effects on salivary glands: dry mouth. Oral Dis 2003;9:165–76.
- 30.Storbeck T, Qian F, Marek C et al. Dose-dependent association between xerostomia and number of medications among older adults. Spec Care Dentist 2022;42:225-31. https://doi.org/10.1111/scd.12662.
- 31.Kakkar M, Barmak AB, Arany S. Anticholinergic medication and dental caries status in middle-aged xerostomia patients-a retrospective study. J Dent Sci 2022;17(3):1206-11. doi: 10.1016/j.jds.2021.12.014.
- 32.Nederfors T, Isaksson R, Mörnstad H, Dahlöf C. Prevalence of perceived symptoms of dry mouth in an adult Swedish population – relation to age, sex and pharmacotherapy. Comm Dent Oral Epidemiol 1997;25:211-6. https://doi.org/10.1111/j.1600-0528.1997.tb00928.x.
- 33.Närhi TO, Meurman JH, Ainamo A. Xerostomia and hyposalivation: causes, consequences and treatment in the elderly. Drugs Aging 1999;15(2):103-16. doi: 10.2165/00002512-199915020-00004.
- 34.Okamoto A, Miyachi H, Tanaka K et al. Relationship between xerostomia and psychotropic drugs in patients with schizophrenia: evaluation using an oral moisture meter. J Clin Pharm Ther 2016;41(6):684-688. doi: 10.1111/jcpt.12449.
- 35.Buzalaf MAR, Hannas AR, Kato MT. Saliva and dental erosion. J Appl Oral Sci 2012;20(5). https://doi.org/10.1590/S1678-77572012000500001.
- 36.Jurasic MM, Gibson G, Wehler CJ et al. Caries prevalence and associations with medications and medical comorbidities. J Publ Health Dent 2019; 79:34-43.
- 37.Nieuw Amerongen AV, Veerman ECI. Saliva – the defender of the oral cavity. Oral Dis 2002; 8:12-22. https://doi.org/10.1034/j.1601-0825.2002.1o816.x
- 38.Ohara Y, Iwasaki M, Shirobe M et al. Xerostomia as a key predictor of physical frailty among community-dwelling older adults in Japan: a five-year prospective cohort study from The Otassha Study. Arch Gerontol Geriatr 2022; 99:104608. doi: 10.1016/j.archger.2021.104608.
- 39.Weyant RJ, Tracy SL, Anselmo TT et al; American Dental Association Council on Scientific Affairs Expert Panel on Topical Fluoride Caries Preventive Agents. Topical fluoride for caries prevention: executive summary of the updated clinical recommendations and supporting systematic review. J Am Dent Assoc 2013;144(11):1279-91. doi: 10.14219/jada.archive.2013.0057.
- 40.CDC. Guidelines for Infection Control in Dental Health-Care Settings — 2003. https://www.cdc.gov/mmwr/PDF/rr/rr5217.pdf.
- 41.CDC. Infection Prevention and Control of Monkeypox in Healthcare Settings. Updated August 11, 2022. https://www.cdc.gov/poxvirus/monkeypox/clinicians/infection-control-healthcare.html
- 42.CDC. Monkeypox. Information For Veterinarians. https://www.cdc.gov/poxvirus/monkeypox/veterinarian/index.html.
- 43.CDC. Monkeypox. Pets in the Home. https://www.cdc.gov/poxvirus/monkeypox/prevention/pets-in-homes.html.


:sharpen(level=0):output(format=jpeg)/up/2023/05/Fiona-Collins-thumbnail-1-3.jpg)
:sharpen(level=0):output(format=jpeg)/up/2022/09/monkeypox-2.jpg)
