Sugar Consumption, Oral and General Health, and Taxation of Sugar-Sweetened Beverages
Sugar is considered a dietary staple. The word “sugar” is the general term for those carbohydrates that are sweet to the taste and are dissolvable in water. Common sugar used to sweeten a wide variety of drinks and foods is sucrose, which is comprised of glucose and fructose.
Excessive consumption of sugar, and specifically consumption of sugar-sweetened beverages (SSB) is linked to a range of disorders, notably an increased risk of cardiovascular disease1Malik VS, Hu FB. Sugar-sweetened beverages and cardiometabolic health: an update of the evidence. Nutrients. 2019;11(8). and diabetes2Imamura F, O’Connor L, Ye Z, Mursu J, Hayashino Y, Bhupathiraju SN, et al. Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta-analysis, and estimation of population attributable fraction. BMJ. 2015;351:h3576.. This risk is mediated through dyslipidemia and obesity3Bosomworth NJ. Approach to identifying and managing atherogenic dyslipidemia: a metabolic consequence of obesity and diabetes. Can Fam Physician. 2013;59(11):1169-80.. As an example of the impact of SSB on the health of the U.S. population, the increased risk of all-cause death was 11% for every additional 12 oz. of SSB consumed daily, and 24% for every additional 12 oz. of fruit juice consumed daily4Collin LJ, Judd S, Safford M, Vaccarino V, Welsh JA. Association of sugary beverage consumption with mortality risk in US adults: A secondary analysis of data from the REGARDS Study. JAMA Netw Open. 2019;2(5):e193121.. The problem of over consumption of SSB exists globally. In a study from South Korea, the percent of strokes attributable to consumption of SSB was 3.1%, and for obesity it was 9.1%. The authors concluded that approaches to reduce the consumption of SSB would have enormous benefits on health, with large healthcare costs savings. The consumption of SSB is seen to be a particular problem among certain segments of the population5Shim JS, Kang NH, Lee JS, Kim KN, Chung HK, Chung HR, et al. Socioeconomic burden of sugar-sweetened beverages consumption in Korea. Nutr Res Pract. 2019;13(2):134-40.. In the United States, more than 50% of Hispanic adults consumed two or more SSB each day, and more than a third consumed three or more SSB each day6Park S, Ayala GX, Sharkey JR, Blanck HM. Knowledge of health conditions associated with sugar-sweetened beverage intake is low among U.S. Hispanic adults. Am J Health Promot. 2019;33(1):39-47.. In this population knowledge about the adverse effects of SSB was very limited. Further, a study of SSB consumption by young people in the U.S. revealed that two of three children and young adults (2 to 19 years of age) consumed one or more SSB each day. This was observed for non-Hispanic white, non-Hispanic black and Hispanic boys and girls, while consumption was markedly lower for non-Hispanic Asians7Rosinger A, Herrick K, Gahche J, Park S. Sugar-sweetened beverage consumption among U.S. adults, 2011-2014. NCHS Data Brief. 2017(270):1-8..
Consumption of SSB and Dental Caries
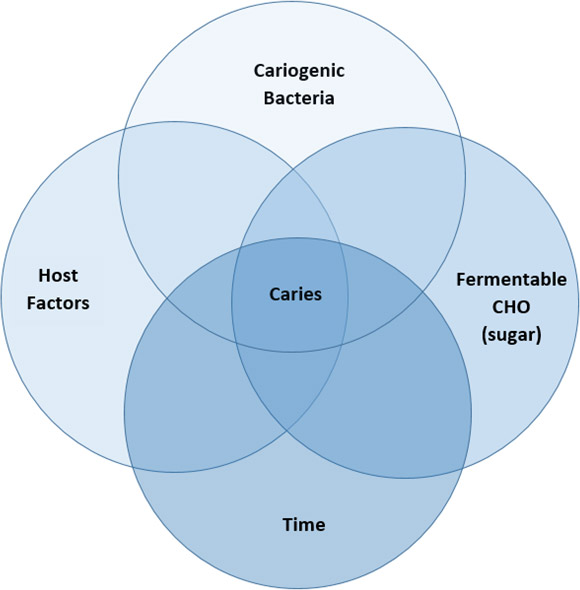
Of importance to the dental profession, the consumption of SSB has been linked to increased prevalence of dental disease, specifically dental caries. Caries is well recognized to be caused by the confluence of several factors, including the presence of cariogenic bacteria, a susceptible host (teeth and related environmental factors such as salivary flow) and fermentable carbohydrate, specifically sucrose. This interaction occurs over time (see Figure 1). Different aspects of this relationship can be modified to reduce the risk of dental caries. One obvious approach is to limit the amount of substrate, here the consumption of sugar. Considering the importance of sugar intake on dental caries, as well as the recognized effect on promotion of obesity, medical and dental providers can work together to deliver an interprofessional message to children and their care-givers about health risks associated with the excessive consumption of sugar8Tinanoff N, Holt K. Introduction to proceedings of healthy futures: engaging the oral health community in childhood obesity prevention national conference. J Public Health Dent. 2017;77 Suppl 1:S5-S7..
An important contributing factor to the development of caries is consumption of SSB. This risk has been identified in many countries and across the life course. Consumption of SSB is recognized as a risk factor for early childhood caries (ECC). In Switzerland, a study of young children with ECC who required general anesthesia for caries treatment focused on parental responses to identify risk factors for ECC. Consumption of SSB before bed was identified as one risk factor9Kraljevic I, Filippi C, Filippi A. Risk indicators of early childhood caries (ECC) in children with high treatment needs. Swiss Dent J. 2017;127(5):398-410..
A study from Taiwan of children with severe ECC tabulated parental responses from both native and immigrant children. Here the combination of SSB and snacking had an important effect on susceptibility to severe EEC10Lin YC, Chang CS, Ho PS, Lee CH, Chen JH, Huang HL. Immigrant-native differences in sugar-sweetened beverage and snack consumption and preventive behaviors associated with severe early childhood caries: A large-scale survey in Taiwan. Int J Environ Res Public Health. 2019 Mar 22;16(6):1047. 2019.. In Japan, a study of first grade children (6 to 7 years old) also identified SSB consumption and frequent snacking as risk factors for dental caries, explaining more than 70% of the association. Self-control was an underlying explanatory factor, as the failure to control these drinking and eating habits were important to the development of caries11Matsuyama Y, Fujiwara T, Ochi M, Isumi A, Kato T. Self-control and dental caries among elementary school children in Japan. Community Dent Oral Epidemiol. 2018;46(5):465-71..
A study from Georgia of the caries experience of third grade children indicated that on average the children drank nearly two SSB per day. After adjustment for demographic and maternal variables, the analysis revealed that each additional SSB consumed was associated with a 22% increase in caries experience12Wilder JR, Kaste LM, Handler A, Chapple-McGruder T, Rankin KM. The association between sugar-sweetened beverages and dental caries among third-grade students in Georgia. J Public Health Dent. 2016;76(1):76-84.. The authors suggested that dentists, physicians, and other healthcare workers must work together to deliver a consistent message about the adverse effects of SSB on both dental caries and obesity.
A study of 12-year-old children from Poland reported that even a small decrease in SSB consumption can have beneficial effects by reducing the prevalence of dental caries. Using national data on sugar consumption and the caries rate, even a modest reduction in sugar consumption was associated with a measurable reduction in the caries rate, and vice-versa13Olczak-Kowalczyk D, Turska A, Gozdowski D, Kaczmarek U. Dental caries level and sugar consumption in 12-year-old children from Poland. Adv Clin Exp Med. 2016;25(3):545-50..
An Australian study examined the effect of drinking SSB on the reported occurrence of a toothache or avoidance of certain foods due to oral problems, measured by the oral health impact (OHI). This study, which included 3,671 adolescents (mean age of 13.2 years), reported that increased consumption of SSB (at least one cup per day) was associated with greater OHI. Sports and energy drinks were a concern14Hardy LL, Bell J, Bauman A, Mihrshahi S. Association between adolescents’ consumption of total and different types of sugar-sweetened beverages with oral health impacts and weight status. Aust N Z J Public Health. 2018;42(1):22-6..
The effect of the consumption of SSB on the oral health status of adults has been examined for U.S. adults with diabetes mellitus. The adjusted odds ratio of having at least six teeth extracted was 2.35 (p=0.0018) if the person drank two or more SSB per day. The authors attributed the increase in the number of extractions to increased sugar consumption associated with SSB. They did note, however, that the reasons for tooth loss were complex15Wiener RC, Shen C, Findley PA, Sambamoorthi U, Tan X. The association between diabetes mellitus, sugar-sweetened beverages, and tooth loss in adults: Evidence from 18 states. J Am Dent Assoc. 2017;148(7):500-9 e4..
A review of the relationship of sugar consumption and dental caries in children came to several important conclusions16Chi DL, Scott JM. Added sugar and dental caries in children: A scientific update and future steps. Dent Clin North Am. 2019;63(1):17-33.:
- Sugar consumption is strongly associated with the caries rate in the United States.
- SSB are the major source of added sugar in children’s diets.
- Sugar intake is associated with several socioeconomic factors, including product availability, and food and drink habits in the home.
- Behavioral interventions should be introduced to reduce sugar intake by children.
- Dental professionals should consider ways to assess sugar intake by children and address this issue in their practices.
- There is benefit to society when interventions are introduced to reduce SSB usage. Societal approaches include a ban on such drinks in schools, placing labels on these drinks that warn of the health risks, and a tax on SSB.
Taxation of SSB
The concept of taxing SSB to reduce consumption represents one public health approach to reduction of risk for chronic diseases and disorders, including obesity (and its strong link to development of diabetes) and dental caries. The case for taxation of SSB is very direct. As the cost of these drinks increase, consumption will decrease. This approach is believed to have the greatest impact on poor communities where consumption of these drinks is high. In these communities the increased cost would be particularly impactful on the decision to purchase these drinks.
A systematic review and meta-analysis of taxation of SSB examined both the political response and public view of taxation of SSB17Eykelenboom M, van Stralen MM, Olthof MR, Schoonmade LJ, Steenhuis IHM, Renders CM, et al. Political and public acceptability of a sugar-sweetened beverages tax: A mixed-method systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2019;16(1):78.. This review emphasized that taxes are generally viewed with skepticism by the public, and less than half of the individuals in the surveyed populations supported a tax on SSB, even as a strategy to reduce obesity. However, if the revenue from that tax was used to pay for health-related initiatives, the two-thirds of the public would be supportive. Another important aspect of any such program was transparency regarding the purpose of the tax.
The introduction of a tax on SSB results in a reduction in both purchase and consumption of SSB18Teng AM, Jones AC, Mizdrak A, Signal L, Genc M, Wilson N. Impact of sugar-sweetened beverage taxes on purchases and dietary intake: Systematic review and meta-analysis. Obes Rev. 2019;20(9):1187-204.. In the United States, the first municipality to implement a tax on SSB was Berkeley California, and after one year a decrease in sales of SSB was reported19Silver LD, Ng SW, Ryan-Ibarra S, Taillie LS, Induni M, Miles DR, et al. Changes in prices, sales, consumer spending, and beverage consumption one year after a tax on sugar-sweetened beverages in Berkeley, California, US: A before-and-after study. PLoS Med. 2017;14(4):e1002283.. A report from Mexico indicated that a tax on SSB was associated with a reduction in the purchase of SSB, and the greatest reduction was seen for those who purchased the most SSB. This was thought to be particularity important since these individuals are at greatest risk for obesity-related disorders, including diabetes and cardiovascular diseases20Ng SW, Rivera JA, Popkin BM, Colchero MA. Did high sugar-sweetened beverage purchasers respond differently to the excise tax on sugar-sweetened beverages in Mexico? Public Health Nutr. 2018:1-7.. A systematic review of the effect of a tax on SSB examined both purchase of SSB and effects on weight, as modified by socio-economic status. The review determined that there was less weight gain across all socio-economic strata, with a greater benefit to those in the lower strata21Backholer K, Sarink D, Beauchamp A, Keating C, Loh V, Ball K, et al. The impact of a tax on sugar-sweetened beverages according to socio-economic position: A systematic review of the evidence. Public Health Nutr. 2016;19(17):3070-84..
Analysis of the impact of a tax on SSB on health outcomes suggest that such a tax reduces consumption of SSB and leads to weight control and weight reduction. Estimates of the effect of a 10% tax on SSB from South Africa indicates a reduction in the number of deaths related to type 2 diabetes, and a reduction in the number of catastrophic health care-related expenditures22Saxena A, Stacey N, Puech PDR, Mudara C, Hofman K, Verguet S. The distributional impact of taxing sugar-sweetened beverages: Findings from an extended cost-effectiveness analysis in South Africa. BMJ Glob Health. 2019;4(4):e001317..
The beneficial effect on health outcomes and expenditures are expected to be pronounced in countries with a heavy disease burden. Mexico has a very high prevalence of diabetes mellitus and cardiovascular disease and in 2014 the country instituted a national tax on SSB. Using established models of the risk for cardiovascular disease, an analysis indicated that a 10% decrease in SSB consumption (due to the tax) would, over a 10 year period, result in nearly 190,000 fewer new cases of diabetes, more than 20,000 fewer myocardial infarctions and strokes, and almost 19,000 fewer deaths. The cost savings would approach $1 billion. The greatest beneficial effect would be seen for the youngest group of adults in their analysis (35-44 years of age;23Sanchez-Romero LM, Penko J, Coxson PG, Fernandez A, Mason A, Moran AE, et al. Projected impact of Mexico’s sugar-sweetened beverage tax policy on diabetes and cardiovascular disease: A modeling study. PLoS Med. 2016;13(11):e1002158.).
Figure 1. The development of dental caries requires 4 components: cariogenic bacteria (i.e. Streptococcus mutans), host factors (including teeth, saliva), fermentable carbohydrate (CHO, specifically sucrose as the substare), all interacting over time.
The Effect of Taxation of SSB on Oral Health
The beneficial effects of a tax on SSB on oral health have been evaluated by projecting changes in the caries rate and the cost of dental treatment, in consideration of age and socioeconomic status. These analyses suggest important beneficial effects. Using a 20% tax rate on SSB, a model analyzed the impact of such a tax in Germany24Schwendicke F, Thomson WM, Broadbent JM, Stolpe M. Effects of taxing sugar-sweetened beverages on caries and treatment costs. J Dent Res. 2016;95(12):1327-32.. The caries rate would decrease, particularly in younger men with a lower income.
Another modelling exercise utilized data from the Netherlands, and evaluated a number of outcomes, including the number of carious lesions that were prevented and the lifetime expenditure that was saved as a result of the reduced need for restorative dental care. Their results indicate prevention of more than one million carious lesions, with a savings of more than 150 million euros. The revenue realized from such a tax would amount to nearly 3.5 billion euros25Jevdjevic M, Trescher AL, Rovers M, Listl S. The caries-related cost and effects of a tax on sugar-sweetened beverages. Public Health. 2019;169:125-32.. Another model which examined data from Australia suggested that a 20% tax on SSB would result in nearly 4 million fewer decayed, missing or filled teeth during a 10-year period, and cost savings of $660 million (Australian). They did caution about a potential adverse effect of such a tax, which is a financial burden on the population26Sowa PM, Keller E, Stormon N, Lalloo R, Ford PJ. The impact of a sugar-sweetened beverages tax on oral health and costs of dental care in Australia. Eur J Public Health. 2019;29(1):173-7..
Oral health care professionals must assume an active role in advising their patients, particularly pediatric patients and their caregivers, about the importance of reducing sugar consumption. A focus on SSB is one important way to have that discussion. This effort will be enhanced with an interprofessional approach to practice, as dental, medical and other healthcare providers deliver a consistent and broad message about the general health and oral health benefits that will be realized with reduction in the consumption of SSB.
A tax on sugar sweetened beverages leads to a reduction in the consumption of sugar. This limits the availability of fermentable CHO and results in a reduction in the development of dental caries.
Conclusions
The review of the impact of a tax on SSB suggests the following:
- A tax on SSB, generally in the range of 20%, can be expected to reduce consumption of SSB.
- The result of this reduction in consumption of sugar will be improved general health (reduction in obesity, diabetes mellitus and cardiovascular disease) and oral health (reduction in the caries rate).
- As related to dental caries, instituting a tax on SSB by itself cannot be expected to have a dramatic effect on the caries rate in all countries, especially if sugar is consumed in different foods27Urwannachotima N, Hanvoravongchai P, Ansah JP, Prasertsom P, Koh VRY. Impact of sugar-sweetened beverage tax on dental caries: a simulation analysis. BMC Oral Health. 2020;20(1):76..
- Since reduction in sugar intake is an important part of a healthy lifestyle, and impacts medical and dental outcomes, a combined, interprofessional approach to messaging about reduction in sugar consumption is needed for maximum impact. This includes physicians and other medical professionals, dentists and other dental professionals, as well as public health efforts such as a taxation on SSB28Bridge G, Lomazzi M, Bedi R. A call to action: advocating for the integration of oral health promotion and public health via sugar sweetened beverage taxation. Br Dent J. 2019;227(8):663-4.. The integration of oral and general health, with a consistent message about the importance of a healthy lifestyle, is a direction for the future.
- The revenue realized from a tax on SSB should be used to promote general and oral health.
- There are some possible indirect adverse effects of a tax on SSB, which include a financial challenge on local stores and small markets that will see a drop in revenue with a reduction in the sale of SSB.
References
- 1.Dominy SS, et al. Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Sci Adv. 2019;5(1):eaau3333 https://www.ncbi.nlm.nih.gov/pubmed/30746447.
- 2.Sadrameli M, et al. Linking mechanisms of periodontitis to Alzheimer’s disease. Curr Opin Neurol. 2020;33(2):230-8 https://www.ncbi.nlm.nih.gov/pubmed/32097126.
- 3.Borsa L, et al. Analysis the link between periodontal diseases and Alzheimer’s disease: A systematic review. Int J Environ Res Public Health. 2021;18(17) https://www.ncbi.nlm.nih.gov/pubmed/34501899.
- 4.Costa MJF, et al. Relationship of Porphyromonas gingivalis and Alzheimer’s disease: A systematic review of pre-clinical studies. Clin Oral Investig. 2021;25(3):797-806 https://www.ncbi.nlm.nih.gov/pubmed/33469718.
- 5.Munoz Fernandez SS, Lima Ribeiro SM. Nutrition and Alzheimer disease. Clin Geriatr Med. 2018;34(4):677-97 https://www.ncbi.nlm.nih.gov/pubmed/30336995.
- 6.Aquilani R, et al. Is the Brain Undernourished in Alzheimer’s Disease? Nutrients. 2022;14(9) https://www.ncbi.nlm.nih.gov/pubmed/35565839.
- 7.Fukushima-Nakayama Y, et al. Reduced mastication impairs memory function. J Dent Res. 2017;96(9):1058-66 https://www.ncbi.nlm.nih.gov/pubmed/28621563.
- 8.Kim HB, et al. Abeta accumulation in vmo contributes to masticatory dysfunction in 5XFAD Mice. J Dent Res. 2021;100(9):960-7 https://www.ncbi.nlm.nih.gov/pubmed/33719684.
- 9.Miura H, et al. Relationship between cognitive function and mastication in elderly females. J Oral Rehabil. 2003;30(8):808-11 https://www.ncbi.nlm.nih.gov/pubmed/12880404.
- 10.Lexomboon D, et al. Chewing ability and tooth loss: association with cognitive impairment in an elderly population study. J Am Geriatr Soc. 2012;60(10):1951-6 https://www.ncbi.nlm.nih.gov/pubmed/23035667.
- 11.Elsig F, et al. Tooth loss, chewing efficiency and cognitive impairment in geriatric patients. Gerodontology. 2015;32(2):149-56 https://www.ncbi.nlm.nih.gov/pubmed/24128078.
- 12.Kim EK, et al. Relationship between chewing ability and cognitive impairment in the rural elderly. Arch Gerontol Geriatr. 2017;70:209-13 https://www.ncbi.nlm.nih.gov/pubmed/28214402.
- 13.Kim MS, et al. The association between mastication and mild cognitive impairment in Korean adults. Medicine (Baltimore). 2020;99(23):e20653 https://www.ncbi.nlm.nih.gov/pubmed/32502052.
- 14.Cardoso MG, et al. Relationship between functional masticatory units and cognitive impairment in elderly persons. J Oral Rehabil. 2019;46(5):417-23 https://www.ncbi.nlm.nih.gov/pubmed/30614023.
- 15.Popovac A, et al. Oral health status and nutritional habits as predictors for developing alzheimer’s disease. Med Princ Pract. 2021;30(5):448-54 https://www.ncbi.nlm.nih.gov/pubmed/34348313.
- 16.Park T, et al. More teeth and posterior balanced occlusion are a key determinant for cognitive function in the elderly. Int J Environ Res Public Health. 2021;18(4) https://www.ncbi.nlm.nih.gov/pubmed/33669490.
- 17.Lin CS, et al. Association between tooth loss and gray matter volume in cognitive impairment. Brain Imaging Behav. 2020;14(2):396-407 https://www.ncbi.nlm.nih.gov/pubmed/32170642.
- 18.Kumar S, et al. Oral health status and treatment need in geriatric patients with different degrees of cognitive impairment and dementia: a cross-sectional study. J Family Med Prim Care. 2021;10(6):2171-6 https://www.ncbi.nlm.nih.gov/pubmed/34322409.
- 19.Delwel S, et al. Chewing efficiency, global cognitive functioning, and dentition: A cross-sectional observational study in older people with mild cognitive impairment or mild to moderate dementia. Front Aging Neurosci. 2020;12:225 https://www.ncbi.nlm.nih.gov/pubmed/33033478.
- 20.Da Silva JD, et al. Association between cognitive health and masticatory conditions: a descriptive study of the national database of the universal healthcare system in Japan. Aging (Albany NY). 2021;13(6):7943-52 https://www.ncbi.nlm.nih.gov/pubmed/33739304.
- 21.Galindo-Moreno P, et al. The impact of tooth loss on cognitive function. Clin Oral Investig. 2022;26(4):3493-500 https://www.ncbi.nlm.nih.gov/pubmed/34881401.
- 22.Stewart R, et al. Adverse oral health and cognitive decline: The health, aging and body composition study. J Am Geriatr Soc. 2013;61(2):177-84 https://www.ncbi.nlm.nih.gov/pubmed/23405916.
- 23.Dintica CS, et al. The relation of poor mastication with cognition and dementia risk: A population-based longitudinal study. Aging (Albany NY). 2020;12(9):8536-48 https://www.ncbi.nlm.nih.gov/pubmed/32353829.
- 24.Kim MS, Han DH. Does reduced chewing ability efficiency influence cognitive function? Results of a 10-year national cohort study. Medicine (Baltimore). 2022;101(25):e29270 https://www.ncbi.nlm.nih.gov/pubmed/35758356.
- 25.Ko KA, et al. The Impact of Masticatory Function on Cognitive Impairment in Older Patients: A Population-Based Matched Case-Control Study. Yonsei Med J. 2022;63(8):783-9 https://www.ncbi.nlm.nih.gov/pubmed/35914761.
- 26.Garre-Olmo J. [Epidemiology of Alzheimer’s disease and other dementias]. Rev Neurol. 2018;66(11):377-86 https://www.ncbi.nlm.nih.gov/pubmed/29790571.
- 27.Stephan BCM, et al. Secular Trends in Dementia Prevalence and Incidence Worldwide: A Systematic Review. J Alzheimers Dis. 2018;66(2):653-80 https://www.ncbi.nlm.nih.gov/pubmed/30347617.
- 28.Lopez OL, Kuller LH. Epidemiology of aging and associated cognitive disorders: Prevalence and incidence of Alzheimer’s disease and other dementias. Handb Clin Neurol. 2019;167:139-48 https://www.ncbi.nlm.nih.gov/pubmed/31753130.
- 29.Ono Y, et al. Occlusion and brain function: mastication as a prevention of cognitive dysfunction. J Oral Rehabil. 2010;37(8):624-40 https://www.ncbi.nlm.nih.gov/pubmed/20236235.
- 30.Kubo KY, et al. Masticatory function and cognitive function. Okajimas Folia Anat Jpn. 2010;87(3):135-40 https://www.ncbi.nlm.nih.gov/pubmed/21174943.
- 31.Chen H, et al. Chewing Maintains Hippocampus-Dependent Cognitive Function. Int J Med Sci. 2015;12(6):502-9 https://www.ncbi.nlm.nih.gov/pubmed/26078711.
- 32.Azuma K, et al. Association between Mastication, the Hippocampus, and the HPA Axis: A Comprehensive Review. Int J Mol Sci. 2017;18(8) https://www.ncbi.nlm.nih.gov/pubmed/28771175.
- 33.Chuhuaicura P, et al. Mastication as a protective factor of the cognitive decline in adults: A qualitative systematic review. Int Dent J. 2019;69(5):334-40 https://www.ncbi.nlm.nih.gov/pubmed/31140598.
- 34.Lopez-Chaichio L, et al. Oral health and healthy chewing for healthy cognitive ageing: A comprehensive narrative review. Gerodontology. 2021;38(2):126-35 https://www.ncbi.nlm.nih.gov/pubmed/33179281.
- 35.Tada A, Miura H. Association between mastication and cognitive status: A systematic review. Arch Gerontol Geriatr. 2017;70:44-53 https://www.ncbi.nlm.nih.gov/pubmed/28042986.
- 36.Ahmed SE, et al. Influence of Dental Prostheses on Cognitive Functioning in Elderly Population: A Systematic Review. J Pharm Bioallied Sci. 2021;13(Suppl 1):S788-S94 https://www.ncbi.nlm.nih.gov/pubmed/34447202.
- 37.Tonsekar PP, et al. Periodontal disease, tooth loss and dementia: Is there a link? A systematic review. Gerodontology. 2017;34(2):151-63 https://www.ncbi.nlm.nih.gov/pubmed/28168759.
- 38.Nangle MR, Manchery N. Can chronic oral inflammation and masticatory dysfunction contribute to cognitive impairment? Curr Opin Psychiatry. 2020;33(2):156-62 https://www.ncbi.nlm.nih.gov/pubmed/31895157.
- 39.Nakamura T, et al. Oral dysfunctions and cognitive impairment/dementia. J Neurosci Res. 2021;99(2):518-28 https://www.ncbi.nlm.nih.gov/pubmed/33164225.
- 40.Weijenberg RAF, et al. Mind your teeth-The relationship between mastication and cognition. Gerodontology. 2019;36(1):2-7 https://www.ncbi.nlm.nih.gov/pubmed/30480331.
- 41.Asher S, et al. Periodontal health, cognitive decline, and dementia: A systematic review and meta-analysis of longitudinal studies. J Am Geriatr Soc. 2022;70(9):2695-709 https://www.ncbi.nlm.nih.gov/pubmed/36073186.
- 42.Lin CS. Revisiting the link between cognitive decline and masticatory dysfunction. BMC Geriatr. 2018;18(1):5 https://www.ncbi.nlm.nih.gov/pubmed/29304748.
- 43.Wu YT, et al. The changing prevalence and incidence of dementia over time – current evidence. Nat Rev Neurol. 2017;13(6):327-39 https://www.ncbi.nlm.nih.gov/pubmed/28497805.
- 44.National Psoriasis Foundation. Soriatane (Acitretin). https://www.psoriasis.org/soriatane-acitretin/.
- 45.National Psoriasis Foundation. Current Biologics on the Market. https://www.psoriasis.org/current-biologics-on-the-market/.
- 46.Dalmády S, Kemény L, Antal M, Gyulai R. Periodontitis: a newly identified comorbidity in psoriasis and psoriatic arthritis. Expert Rev Clin Immunol 2020;16(1):101-8. doi: 10.1080/1744666X.2019.1700113.
:sharpen(level=0):output(format=jpeg)/up/2023/05/Ira-Lamster-3.jpg)
:sharpen(level=0):output(format=jpeg)/up/2020/08/sugar-consumption-2.jpg)